Abstract
Purpose
To evaluate the postoperative outcomes of a multimodal perioperative pain management protocol with rectus sheath blocks (RSBs) or intrathecal morphine (ITM) injection for minimally invasive colorectal cancer surgery.
Methods
A total of 112 patients underwent minimally invasive colorectal surgery. Forty-one patients underwent RSB (group 1), whereas 71 patients underwent ITM (group 2) in addition to multimodal pain management using enhanced recovery after the surgery protocol. To adjust for the baseline differences and selection bias, baseline characteristics and postoperative outcomes were compared using propensity score matching.
Results
Forty patients were evaluated in each group. There was no significant difference in the length of hospital stay between the two groups. According to the Comprehensive Complication Index (CCI) score, the postoperative complication rate was significantly lower in the RSB group (3.0 ± 7.8) than in the ITM group (8.1 ± 10.9; p = 0.016). During the first 24 h after surgery, the median postoperative visual analog scale score was significantly higher in the RSB group than in the ITM group (2.0 ± 1.1 vs. 1.5 ± 1.2; p = 0.048). Postoperative morphine use was also significantly higher in the RSB group than in the ITM group in the first 24 h (23.7 ± 19.8 vs 11.6 ± 15.6%; p = 0.003) and 48 h (16.9 ± 24.8 vs. 7.5 ± 11.9; p = 0.036) after surgery. Significant urinary retention occurred after the in the RSB and ITM groups (5% vs. 45%; p < 0.001).
Conclusion
Although the RSB group had higher morphine use during the first 48 h after surgery, the length of hospital stay remained the same and the complications were less in terms of the CCI score. Thus, transperitoneal RSB is a safe and feasible approach for postoperative pain management following minimally invasive procedures.



Similar content being viewed by others
References
Kim MK, Kim JG, Lee G, Won DD, Lee YS, Kye BH et al (2019) Comparison of the effects of an ERAS program and a single-port laparoscopic surgery on postoperative outcomes of colon cancer patients. Sci Rep 9:11998
Dahl JB, Nielsen RV, Wetterslev J, Nikolajsen L, Hamunen K, Kontinen VK et al (2014) Post-operative analgesic effects of paracetamol, NSAIDs, glucocorticoids, gabapentinoids and their combinations: a topical review. Acta Anaesthesiol Scand 58:1165–1181
Kim WJ, Mun JY, Kim HJ, Yoon SH, Han SR, Bae JH et al (2021) Surgical rectus sheath block combined with multimodal pain management reduces postoperative pain and analgesic requirement after single-incision laparoscopic appendectomy: a retrospective study. Int J Colorectal Dis 36:75–82
Lee CS, Park SJ, Hong SH, Shim JW, Chae MS, Han SR et al (2021) Clinical effect of multimodal perioperative pain management protocol for minimally invasive colorectal cancer surgery: Propensity score matching study. Asian J Surg 44:471–475
Virlos I, Clements D, Beynon J, Ratnalikar V, Khot U (2010) Short-term outcomes with intrathecal versus epidural analgesia in laparoscopic colorectal surgery. Br J Surg 97:1401–1406
Shim JW, Cho YJ, Moon HW, Park J, Lee HM, Kim YS et al (2021) Analgesic efficacy of intrathecal morphine and bupivacaine during the early postoperative period in patients who underwent robotic-assisted laparoscopic prostatectomy: a prospective randomized controlled study. BMC Urol 21:30
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Tu RH, Lin JX, Li P, Xie JW, Wang JB, Lu J et al (2018) Comprehensive complication index predicts cancer-specific survival of patients with postoperative complications after curative resection of gastric cancer. Gastroenterol Res Pract 2018:4396018
Nagata J, Watanabe J, Sawatsubashi Y, Akiyama M, Arase K, Minagawa N et al (2017) Novel technique of abdominal wall nerve block for laparoscopic colostomy: Rectus sheath block with transperitoneal approach. World J Gastrointest Surg 9:182–185
Yurashevich M, Habib AS (2019) Monitoring, prevention and treatment of side effects of long-acting neuraxial opioids for post-cesarean analgesia. Int J Obstet Anesth 39:117–128
Han SR, Lee CS, Bae JH, Lee HJ, Yoon MR, Lee DS et al (2021) The additional analgesic effects of transverse abdominis plane block in patients receiving low-dose intrathecal morphine for minimally invasive colorectal surgery: a randomized, single-blinded study. Ann Surg Treat Res 101:221–230
Colibaseanu DT, Osagiede O, Merchea A, Ball CT, Bojaxhi E, Panchamia JK et al (2019) Randomized clinical trial of liposomal bupivacaine transverse abdominis plane block versus intrathecal analgesia in colorectal surgery. Br J Surg 106:692–699
Meylan N, Elia N, Lysakowski C, Tramer MR (2009) Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth 102:156–167
Young J, Macpherson A, Thakerar A, Alexander M (2021) Intrathecal morphine in postoperative analgesia for colorectal cancer surgery: a retrospective study. Pain Med 22:402–406
Tudor EC, Yang W, Brown R, Mackey PM (2015) Rectus sheath catheters provide equivalent analgesia to epidurals following laparotomy for colorectal surgery. Ann R Coll Surg Engl 97:530–533
Gwirtz KH, Young JV, Byers RS, Alley C, Levin K, Walker SG et al (1999) The safety and efficacy of intrathecal opioid analgesia for acute postoperative pain: seven years’ experience with 5969 surgical patients at Indiana University Hospital. Anesth Analg 88:599–604
Sultan P, Halpern SH, Pushpanathan E, Patel S, Carvalho B (2016) The effect of intrathecal morphine dose on outcomes after elective cesarean delivery: a meta-analysis. Anesth Analg 123:154–164
Osaka Y, Kashiwagi M, Nagatsuka Y, Miwa S (2011) [Ultrasound-guided rectus sheath blockade is a safe and accurate method for emergency ileostomy for patients with coagulopathy]. Masui 60:1202–1204
Gurnaney HG, Maxwell LG, Kraemer FW, Goebel T, Nance ML, Ganesh A (2011) Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br J Anaesth 107:790–795
Gehling M, Tryba M (2009) Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: a meta-analysis. Anaesthesia 64:643–651
Skinner AV, Lauder GR (2007) Rectus sheath block: successful use in the chronic pain management of pediatric abdominal wall pain. Paediatr Anaesth 17:1203–1211
Uchinami Y, Sakuraya F, Tanaka N, Hoshino K, Mikami E, Ishikawa T et al (2017) Comparison of the analgesic efficacy of ultrasound-guided rectus sheath block and local anesthetic infiltration for laparoscopic percutaneous extraperitoneal closure in children. Paediatr Anaesth 27:516–523
Lancaster P, Chadwick M (2010) Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth 104:509–510
Gupta M, Naithani U, Singariya G, Gupta S (2016) Comparison of 0.25% ropivacaine for intraperitoneal instillation v/s rectus sheath block for postoperative pain relief following laparoscopic cholecystectomy: a prospective study. J Clin Diagn Res 10:UC10–UC15
Hansen TG (2004) Ropivacaine: a pharmacological review. Expert Rev Neurother 4:781–791
Das NT, Deshpande C (2017) Effects of intraperitoneal local anaesthetics bupivacaine and ropivacaine versus placebo on postoperative pain after laparoscopic cholecystectomy: a randomised double blind study. J Clin Diagn Res 11:UC08–UC12
Acknowledgements
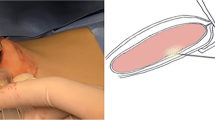
We would like to express our gratitude to Dr. Haifa Alotaibi for her assistance in illustrating the rectus sheath block technique.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board of the College of Medicine, The Catholic University of Korea (KC21RISI0763).
Consent to participate
Not applicable
Consent for publication
Not applicable
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Al-Sawat, A., Lee, C.S., Hong, S.H. et al. Clinical effect of rectus sheath block compared to intrathecal morphine injection for minimally invasive colorectal cancer surgery: a propensity score–matched study. Int J Colorectal Dis 37, 665–672 (2022). https://doi.org/10.1007/s00384-022-04094-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04094-x