Abstract
Purpose
The aim of this multicentre study was to analyse the effects of patent sphincter lesions and previous sphincter repair on the results of sacral neuromodulation (SNM) treatment on patients with faecal incontinence (FI).
Methods
Patients examined by endoanal ultrasound (EAUS) with FI as the indication for SNM treatment were included in the study. Data was collected from all the centres providing SNM treatment in Finland and analysed for differences in treatment outcomes.
Results
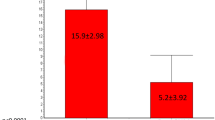
A total of 237 patients treated for incontinence with SNM had been examined by EAUS. Of these patients, 33 had a history of previous delayed sphincter repair. A patent sphincter lesion was detected by EAUS in 128 patients. The EAUS finding did not influence the SNM test phase outcome (p = 0.129) or the final treatment outcome (p = 0.233). Patient’s history of prior sphincter repair did not have a significant effect on the SNM test (p = 0.425) or final treatment outcome (p = 0.442).
Conclusions
Results of our study indicate that a sphincter lesion or previous sphincter repair has no significant effect on the outcome of SNM treatment. Our data suggests that delayed sphincter repair prior to SNM treatment initiation for FI is not necessary.

Similar content being viewed by others
References
Aitola P, Lehto K, Fonsell R, Huhtala H (2010) Prevalence of faecal incontinence in adults aged 30 years or more in general population. Color Dis 12(7):687–691. https://doi.org/10.1111/j.1463-1318.2009.01878.x
Chatoor DR, Taylor SJ, Cohen CR, Emmanuel AV (2007) Faecal incontinence. Br J Surg 94(2):134–144. https://doi.org/10.1002/bjs.5676
Sharma A, Yuan L, Marshall RJ, Merrie AE, Bissett IP (2016) Systematic review of the prevalence of faecal incontinence. Br J Surg 103(12):1589–1597. https://doi.org/10.1002/bjs.10298
Memon HU, Handa VL (2013) Vaginal childbirth and pelvic floor disorders. Womens Health (Lond) 9(3):265–277; quiz 276-267. https://doi.org/10.2217/whe.13.17
Samarasekera DN, Bekhit MT, Wright Y, Lowndes RH, Stanley KP, Preston JP, Preston P, Speakman CT (2008) Long-term anal continence and quality of life following postpartum anal sphincter injury. Color Dis 10(8):793–799. https://doi.org/10.1111/j.1463-1318.2007.01445.x
Thomas GP, Gould LE, Casunuran F, Kumar DA (2017) A retrospective review of 1495 patients with obstetric anal sphincter injuries referred for assessment of function and endoanal ultrasonography. Int J Color Dis 32(9):1321–1325. https://doi.org/10.1007/s00384-017-2851-3
Oberwalder M, Dinnewitzer A, Baig MK, Thaler K, Cotman K, Nogueras JJ, Weiss EG, Efron J, III AMV, Wexner SD (2004) The association between late-onset fecal incontinence and obstetric anal sphincter defects. Arch Surg 139(APR 2004):429–432. https://doi.org/10.1001/archsurg.139.4.429
Oude Lohuis EJ, Everhardt E (2014) Outcome of obstetric anal sphincter injuries in terms of persisting endoanal ultrasonographic defects and defecatory symptoms. Int J Gynaecol Obstet 126(1):70–73. https://doi.org/10.1016/j.ijgo.2014.01.018
Norton C, Thomas L, Hill J, Guideline Development G (2007) Management of faecal incontinence in adults: summary of NICE guidance. BMJ 334(7608):1370–1371. https://doi.org/10.1136/bmj.39231.633275.AD
Dudding TC, Vaizey CJ, Kamm MA (2008) Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg 247(2):224–237. https://doi.org/10.1097/SLA.0b013e318142cdf4
Johnson E, Carlsen E, Steen TB, Backer Hjorthaug JO, Eriksen MT, Johannessen HO (2010) Short- and long-term results of secondary anterior sphincteroplasty in 33 patients with obstetric injury. Acta Obstet Gynecol Scand 89(11):1466–1472. https://doi.org/10.3109/00016349.2010.519019
Pinta T, Kylänpää-Bäck M-L, Salmi T, Järvinen HJ, Luukkonen P (2001) Delayed sphincter repair for obstetric ruptures: analysis of failure. Color Dis 5:73–78. https://doi.org/10.1046/j.1463-1318.2003.00408.x
Thaha MA, Abukar AA, Thin NN, Ramsanahie A, Knowles CH (2015) Sacral nerve stimulation for faecal incontinence and constipation in adults. Cochrane Database Syst Rev 8:CD004464. https://doi.org/10.1002/14651858.CD004464.pub3
Evers EC, Blomquist JL, McDermott KC, Handa VL (2012) Obstetrical anal sphincter laceration and anal incontinence 5-10 years after childbirth. Am J Obstet Gynecol 207(5):425 e421–425 e426. https://doi.org/10.1016/j.ajog.2012.06.055
Kumar R, Ooi C, Nicoll A (2012) Anal incontinence and quality of life following obstetric anal sphincter injury. Arch Gynecol Obstet 285(3):591–597. https://doi.org/10.1007/s00404-011-2003-x
Shah BJ, Chokhavatia S, Rose S (2012) Fecal incontinence in the elderly: FAQ. Am J Gastroenterol 107(11):1635–1646. https://doi.org/10.1038/ajg.2012.284
Emil A, Tanagho RAS (1982) Bladder pacemaker: scientific basis and clinical future. Urology 20:614–619. https://doi.org/10.1016/0090-4295(82)90312
Hong KD, da Silva G, Wexner SD (2014) What is the best option for failed sphincter repair? Color Dis 16(4):298–303. https://doi.org/10.1111/codi.12525
Quezada Y, Whiteside JL, Rice T, Karram M, Rafferty JF, Paquette IM (2015) Does preoperative anal physiology testing or ultrasonography predict clinical outcome with sacral neuromodulation for fecal incontinence? Int Urogynecol J 26(11):1613–1617. https://doi.org/10.1007/s00192-015-2746-1
Rodrigues FG, Chadi SA, Cracco AJ, Sands DR, Zutshi M, Gurland B, Da Silva G, Wexner SD (2017) Faecal incontinence in patients with a sphincter defect: comparison of sphincteroplasty and sacral nerve stimulation. Color Dis 19(5):456–461. https://doi.org/10.1111/codi.13510
Rydningen MB, Dehli T, Wilsgaard T, Lindsetmo RO, Kumle M, Stedenfeldt M, Norderval S (2017) Sacral neuromodulation for faecal incontinence following obstetric sphincter injury - outcome of percutaneous nerve evaluation. Color Dis 19(3):274–282. https://doi.org/10.1111/codi.13472
Roy AL, Gourcerol G, Menard JF, Michot F, Leroi AM, Bridoux V (2014) Predictive factors for successful sacral nerve stimulation in the treatment of fecal incontinence: lessons from a comprehensive treatment assessment. Dis Colon Rectum 57(6):772–780. https://doi.org/10.1097/DCR.0000000000000115
Dudding TC, Pares D, Vaizey CJ, Kamm MA (2008) Predictive factors for successful sacral nerve stimulation in the treatment of faecal incontinence: a 10-year cohort analysis. Color Dis 10(3):249–256. https://doi.org/10.1111/j.1463-1318.2007.01319.x
Govaert B, Melenhorst J, Nieman FH, Bols EM, van Gemert WG, Baeten CG (2009) Factors associated with percutaneous nerve evaluation and permanent sacral nerve modulation outcome in patients with fecal incontinence. Dis Colon Rectum 52(10):1688–1694. https://doi.org/10.1007/DCR.0b013e3181b55595
Melenhorst J, Koch SM, Uludag O, van Gemert WG, Baeten CG (2007) Sacral neuromodulation in patients with faecal incontinence: results of the first 100 permanent implantations. Color Dis 9(8):725–730. https://doi.org/10.1111/j.1463-1318.2007.01241.x
Boyle DJ, Knowles CH, Lunniss PJ, Scott SM, Williams NS, Gill KA (2009) Efficacy of sacral nerve stimulation for fecal incontinence in patients with anal sphincter defects. Dis Colon Rectum 52(7):1234–1239. https://doi.org/10.1007/DCR.0b013e31819f7400
Ramage L, Yen C, Qiu S, Simillis C, Kontovounisios C, Tekkis P, Tan E (2017) Functional and quality of life outcomes following obstetric anal sphincter injury (OASI): does the grade of injury affect outcomes? Int Urogynecol J 28(11):1709–1717. https://doi.org/10.1007/s00192-017-3334-3
Chan MK, Tjandra JJ (2008) Sacral nerve stimulation for fecal incontinence: external anal sphincter defect vs. intact anal sphincter. Dis Colon Rectum 51(7):1015–1024; discussion 1024-1015. https://doi.org/10.1007/s10350-008-9326-0
Melenhorst J, Koch SM, Uludag O, van Gemert WG, Baeten CG (2008) Is a morphologically intact anal sphincter necessary for success with sacral nerve modulation in patients with faecal incontinence? Color Dis 10(3):257–262. https://doi.org/10.1111/j.1463-1318.2007.01375.x
Kairaluoma MV, Raivio P, Aarnio MT, Kellokumpu IH (2004) Immediate repair of obstetric anal sphincter rupture: medium-term outcome of the overlap technique. Dis Colon Rectum 47(8):1358–1363. https://doi.org/10.1007/s10350-004-0596-x
Acknowledgments
We would like to thank Ms. Elizabeth Prouty, for her revision of the English language.
Author information
Authors and Affiliations
Ethics declarations
This study was conducted in accordance with Finnish Medical Research Act 488/199, 295/2004 and approved by the Ethics Committee of the Hospital District of Southwest Finland (ETMK: 163/1801/2015).
Appendices
Appendix 1
The EAUS imaging devices were all supplied by BK Medical. The models varied over the period of 1999–2017, with models Cheetah and Leopard being in use from 1999 to 2002, Falcon from 1999 to 2009, Hawk from 2000 to 2009, Pro Focus Yellow and Green from 2005 to 2010, Pro Focus Blue from 2005 to 2012, Pro Focus Ultraview and Flex Focus 400 from 2009 to 2017, Flex Focus 500 from 2011 to 2017, Flex Focus 800 from 2012 to 2017 and bk3000 and bk5000 from 2014 to 2017. Transducers used with these scanners have varied over the period from 1999 to 2017, with model 1850 being in use from 1999 to 2012, model 2050 from 1999 to 2012, model 2052 from 2005 to 2017 and model 20R3 from 2015 to 2017
Appendix 2
All of the implanted devices were supplied by Medtronic® Inc. (Minneapolis, Minnesota, USA). Until 2002, a non-tined lead was used. Model 3057 PNE (Medtronic® Inc. Minneapolis, USA) was used for temporary evaluation of therapeutic success. A Quadripolar lead model 3093 tined lead was used from 2003 and changed to model 3889 in 2014
Rights and permissions
About this article
Cite this article
Kirss, J., Pinta, T., Rautio, T. et al. Impact of sphincter lesions and delayed sphincter repair on sacral neuromodulation treatment outcomes for faecal incontinence: results from a Finnish national cohort study. Int J Colorectal Dis 33, 1709–1714 (2018). https://doi.org/10.1007/s00384-018-3161-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3161-0