Abstract
Purpose
Fundoplication is frequently used in children with neurologic impairment even in the absence of reflux due to concerns for future gastric feeding intolerance, but supporting data are lacking. We aimed to determine the incidence of secondary antireflux procedures (fundoplication or gastrojejunostomy (GJ)) post gastrostomy tube (GT) placement in children with and without neurologic impairment.
Methods
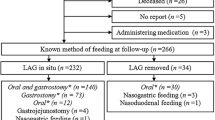
Children under 18 undergoing a GT placement without fundoplication between 2010 and 2020 were identified utilizing the PearlDiver Mariner national patient claims database. Children with a diagnosis of cerebral palsy or a degenerative neurologic disease were identified and compared to children without these diagnoses. The incidence of delayed fundoplication or conversion to GJ were compared utilizing Kaplan–Meier and Cox proportional hazards regression analyses.
Results
A total of 14,965 children underwent GT placement, of which 3712 (24.8%) had a diagnosis of neurologic impairment. The rate of concomitant fundoplication was significantly higher among children with a diagnosis of neurologic impairment as compared to those without (9.3% vs 6.4%, p < 0.001). While children with neurologic impairment had a significantly higher rate of fundoplication or GJ conversion at 5 years compared to children without (12.6% [95% confidence interval (CI): 11.4%–13.8%] vs 8.6% [95% CI 8.0%–9.2%], p < 0.001), the overall incidence remained low.
Conclusion
Although children with neurologic impairment have a higher rate of requiring an antireflux procedure or GJ conversion than other children, the overall rate remains less than 15%. Fundoplication should not be utilized in children without clinical reflux on the basis of neurologic impairment alone.


Similar content being viewed by others
References
Fox D, Campagna EJ, Friedlander J, Partrick DA, Rees DI, Kempe A (2014) National trends and outcomes of pediatric gastrostomy tube placement. J Pediatr Gastroenterol Nutr 59(5):582–588
Glasson EJ, Wong K, Leonard H, Forbes D, Ravikumara M, Mews C et al (2018) Evolving trends of gastrostomy insertion within a pediatric population. J Pediatr Gastroenterol Nutr 67(5):e89–e94
Yap BKY, Nah SA, Chen Y, Low Y (2017) Fundoplication with gastrostomy vs gastrostomy alone: a systematic review and meta-analysis of outcomes and complications. Pediatr Surg Int 33(2):217–228
Viswanath N, Wong D, Channappa D, Kukkady A, Brown S, Samarakkody U (2010) Is prophylactic fundoplication necessary in neurologically impaired children? Eur J Pediatr Surg 20(4):226–229
Jacoby P, Wong K, Srasuebkul P, Glasson EJ, Forbes D, Ravikumara M et al (2020) Risk of hospitalizations following gastrostomy in children with intellectual disability. J Pediatr 217:131–8.e10
Khalid SI, Maasarani S, Wiegmann J, Wiegmann AL, Becerra AZ, Omotosho P et al (2022) Association of bariatric surgery and risk of cancer in patients with morbid obesity. Ann Surg 275(1):1–6
Maassel NL, Shaughnessy MP, Solomon DG, Cowles RA (2021) Trends in fundoplication volume for pediatric gastroesophageal reflux disease. J Pediatr Surg 56(9):1495–1499
Romano C, van Wynckel M, Hulst J, Broekaert I, Bronsky J, Dall’Oglio L et al (2017) European society for paediatric gastroenterology, hepatology and nutrition guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with neurological impairment. J Pediatr Gastroenterol Nutr 65(2):242–264
Fukahori S, Asagiri K, Ishii S, Tanaka Y, Kojima S, Saikusa N et al (2013) Pre and post-operative evaluation of gastroesophageal reflux and esophageal motility in neurologically impaired children using combined pH-multichannel intraluminal impedance measurements. Pediatr Surg Int 29(6):545–551
Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L et al (2009) Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American society for pediatric gastroenterology, hepatology, and nutrition (NASPGHAN) and the European society for pediatric gastroenterology, hepatology, and nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr 49(4):498–547
Lasser MS, Liao JG, Burd RS (2006) National trends in the use of antireflux procedures for children. Pediatrics 118(5):1828–1835
Martin K, Deshaies C, Emil S (2014) Outcomes of pediatric laparoscopic fundoplication: a critical review of the literature. Can J Gastroenterol Hepatol 28(2):97–102
Mauritz FA, van Herwaarden-Lindeboom MY, Stomp W, Zwaveling S, Fischer K, Houwen RH et al (2011) The effects and efficacy of antireflux surgery in children with gastroesophageal reflux disease: a systematic review. J Gastrointest Surg 15(10):1872–1878
Barnhart DC (2016) Gastroesophageal reflux disease in children. Semin Pediatr Surg 25(4):212–218
Wales PW, Diamond IR, Dutta S, Muraca S, Chait P, Connolly B et al (2002) Fundoplication and gastrostomy versus image-guided gastrojejunal tube for enteral feeding in neurologically impaired children with gastroesophageal reflux. J Pediatr Surg 37(3):407–412
Wilson RE, Rao PK, Cunningham AJ, Dewey EN, Krishnaswami S, Hamilton NA (2020) A natural history of gastrojejunostomy tubes in children. J Surg Res 245:461–466
Friedman JN, Ahmed S, Connolly B, Chait P, Mahant S (2004) Complications associated with image-guided gastrostomy and gastrojejunostomy tubes in children. Pediatrics 114(2):458–461
Campwala I, Perrone E, Yanni G, Shah M, Gollin G (2015) Complications of gastrojejunal feeding tubes in children. J Surg Res 199(1):67–71
Morse J, Baird R, Muchantef K, Levesque D, Morinville V, Puligandla PS (2017) Gastrojejunostomy tube complications - a single center experience and systematic review. J Pediatr Surg 52(5):726–733
Livingston MH, Shawyer AC, Rosenbaum PL, Jones SA, Walton JM (2015) Fundoplication and gastrostomy versus percutaneous gastrojejunostomy for gastroesophageal reflux in children with neurologic impairment: a systematic review and meta-analysis. J Pediatr Surg 50(5):707–714
Nelson SP, Chen EH, Syniar GM, Christoffel KK (2000) Prevalence of symptoms of gastroesophageal reflux during childhood: a pediatric practice-based survey. Pediatric practice research group. Arch Pediatr Adolesc Med 154(2):150–154
Vandenplas Y, Salvatore S, Hauser B (2005) The diagnosis and management of gastro-oesophageal reflux in infants. Early Hum Dev 81(12):1011–1024
Funding
This work was supported by internal departmental funds.
Author information
Authors and Affiliations
Contributions
MW contributed to study design, data collection and analysis, drafted the manuscript, and critically reviewed and revised the manuscript. NS and GS contributed to study design, and critically reviewed and revised the manuscript. KH collected data and performed analysis, and critically revised the manuscript. MM, SP, and AS critically reviewed and revised the manuscript for important intellectual content. BG conceptualized and designed the study, supervised data collection, and critically reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Williams, M.D., Skertich, N., Sullivan, G.A. et al. Prophylactic antireflux procedures are not necessary in neurologically impaired children undergoing gastrostomy placement. Pediatr Surg Int 39, 122 (2023). https://doi.org/10.1007/s00383-023-05398-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05398-x