Abstract
Aim of study
Duodenum-preserving resection of the pancreatic head (DPRPH) with Roux-en-Y pancreatojejunostomy is a procedure used to remove focal pathological lesions of the pancreatic head. Although predominantly used in adult patients, it is both safe and effective in children. The aim of this study was to review our experience with this procedure, with focus on its indications, complications and long-term outcomes.
Methods
A retrospective analysis of pediatric patients who underwent DPRPH between 1994 and 2015 was performed. Patient files were reviewed for demographic, diagnostic, operative and histological details, postoperative complications. Patients were contacted telephonically and sent questionnaires to determine long-term outcomes.
Results
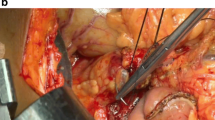
The study cohort consists of 21 patients, 14 girls and 7 boys, with an average age of 11.72 years (range 3 months to 18.6 years), who underwent DPRPH with end-to-end anastomosis of the jejunum to the pancreatic body (Roux-en-Y anastomosis). In four cases the head and also part of the body of the pancreas was resected. In the remaining 17 cases, only the head of the pancreas was resected. Indications for DPRPH were solid pseudopapillary tumor of the pancreas (n = 10), trauma (n = 8), pancreas divisum (n = 1), focal congenital hyperinsulinism (n = 1) and pancreatic cyst (n = 1). The length of follow-up ranged from 1 to 22 years (average 9.66). One patient developed a biliary fistula, which closed spontaneously within 2 weeks after stent insertion. A recurrence of abdominal pain was reported in two patients, occurring at 7 months after the operation in one patient and at 1 year in the other. Pancreatic endocrine insufficiency did not occur in any of the 21 patients. Seven patients currently require a low fat diet, five of which need pancreatic enzyme supplementation. An additional two patients need enzyme supplementation without dietary restriction.
Conclusion
DPRPH is a safe and effective procedure for the treatment of large focal pathological lesions of the pancreatic head in children. As a less invasive procedure than pancreatoduodenectomy, it is more appropriate for the developing child.


Similar content being viewed by others
References
Beger HG, Witte C, Krautzberger W, Bittner R (1980) Erfahrung mit einer das Duodenum erhaltenden Pankreaskopfresektion bei chronischer Pankreatitis. Chirurg 51:303–307
Beger HG, Rau BM, Gansauge F, Poch B (2008) Duodenum-preserving subtotal and total pancreatic head resections for inflammatory and cystic neoplastic lesions of the pancreas. J Gastrointest Surg 12:1127–1132
Beger HG, Krautzberger W, Bittner R et al (1985) Duodenum-preserving resection of the head of the pancreas in patients with severe chronic pancreatitis. Surgery 98:467–471
Beger HG, Buchler M (1990) Duodenum-preserving resection of the head of the pancreas in chronic pancreatitis with inflammatory mass in the head. World J Surg 14:83–87
Izbicki JR, Bloechle C, Knoefel CW, Kuechier T, Binmoeller KF, Broelsch CE (1995) Duodenum-preserving resection of the head of the pancreas in chronic pancreatitis a prospective, randomized trial. Ann Surg 221(4):350–358
Köninger J, Friess H, Müller M, Büchler MW (2004) Duodenum preserving pancreatic head resection in the treatment of chronic pancreatitis. Ann Acad Med Bialostoc 49:53–60
Schlosser W, Rau BM, Poch B, Beger HG (2005) Surgical treatment of pancreas divisum causing chronic pancreatitis: the outcome benefits of duodenum-preserving pancreatic head resection. J Gastrointest Surg 9:710–715
Schneider L, Miller E, Hinz U, Grenacher L, Buchler MW, Werner J (2011) Pancreas divisum: a differentiated surgical approach in symptomatic patients. World J Surg 35:1360–1366
Snajdauf J, Rygl M, Petru O, Kalousova J, Kuklova P, Mixa V, Keil R (2009) Duodenum sparing technique of head resection in solid pseudopapillary tumor of the pancreas in children. Eur J Pediatr Surg 19(6):354–357
Zampieri N, Schiavo N, Capelli P, Scarpa A, Bassi C, Camoglio FS (2011) Pseudopapillary tumor in pediatric age: clinical and surgical management. Pediatr Surg Int 27:1271–1275
Ren Z, Zhang P, Zhang X, Liu B (2014) Solid pseudopapillary neoplasms of the pancreas: clinicopathologic features and surgical treatment of 19 cases. Int J Clin Exp Pathol 7(10):6889–6897
Snajdauf J, Rygl M, Kalousova J, Kucera A, Petru O, Pycha K, Mixa V, Keil R, Hríbal Z (2007) Surgical management of major pancreatic injury in children. Eur J Pediatr Surg 17:317–321
Bredbeck BC, Moore EE, Carlton C, Barnett CC Jr (2015) Duodenum preserving pancreatic head resection (Beger procedure) for pancreatic trauma. J Trauma Acute Care Surg 78:649–651
Beger HG, Siech M, Poch B, Mayer B, Schoenberg MH (2015) Limited Surgery for benign tumours of the pancreas: a systematic review. World J Surg 39:1557–1566
Diener MK, Rahbari NN, Fischer L et al (2008) Duodenum-preserving pancreatic head resection versus pancreatoduodenectomy for surgical treatment of chronic pancreatitis. A systematic review and meta-analysis. Ann Surg 247:950–961
Rebhandl W, Felberbauer FX, Puig S, Paya K, Hochschorner S, Bartan M, Horcher E (2001) Solid-pseudo-papillary tumor of the pancreas (Frantz tumor) in children: report of four cases and review of the literature. J Surg Oncol 76:289–296
Frantz V (1959) Papillary tumors of the pancreas: benign or malignant? In: Frantz VK (ed) Atlas of tumor pathology. US Armed Forces Institute of Pathology, Washington, pp 32–33
Morita K, Urushihara N, Fukumoto K, Miyano G, Yamoto M, Nouso H, Miyake H, Kaneshiro M (2014) Solid pseudopapillary tumor of the pancreas in children: surgical intervention strategies based on pathological findings. Pediatr Surg Int 30:253–257
Ky BA, Shilyansky J, Gerstle JJ, Taylor G, Filler RM, Grace N, Superina R (1998) Experience with papillary and solid epithelial neoplasms of the pancreas in children. J Pediatr Surg 33:42–44
Marchegiani G, Crippa S, Malleo G et al (2011) Surgical treatment of pancreatic tumors in childhood and adolescence: uncommon neoplazma with favorable outcome. Pancreatology 11:383–389
Speer AL, Erik R. Barthel ER, Patel MM, Tracy C. Grikscheit TC (2012) Solid pseudopapillary tumor of the pancreas: a single-institution 20-year series of pediatric patients. J Pediatr Surg 47:1217–1222
Laje P, Bhatti TR, Adzick NS (2013) Solid pseudopapillary neoplasm of the pancreas in children: a 15-year experience and the identification of a unique immunohistochemical marker. J Pediatr Surg 48:2054–2060
Choi SH, Kim SM, Oh JT, Park JY, Seo JM, Lee SK (2006) Solid pseudopapillary tumor of the pancreas: a multicenter study of 23 pediatric cases. J Pediatr Surg 41:1992–1995
Hwang J, Kim DY, Kim SC, Namgoong JM, Hong SM (2014) Solid-pseudopapillary neoplasm of the pancreas in children: can we predict malignancy? J Pediatr Surg 49:1730–1733
Mahida JB, Thakkar RK, Walker J, Shen R, Brian D, Kenney BD, Prasat V, Aldrink JH (2015) Solid pseudopapillary neoplasm of the pancreas in pediatric patients: a case report and institutional case series. J Pediatr Surg Case Rep 3:149–153
Resende V, Azevedo PHR, Lima L, Portela AR, Sanches MD, Pedrosa MS, Sanches MD, Pedrosa MS (2014) Duodenum-preserving pancreatic head resection in solid pseudopapillary neoplasm—report of a case. Int J Surg Case Rep 5:567–570
Snajdauf J, Pycha K, Rygl M, Kocmichova B, Kodet R, Koutecky J, Cumlivská E (1999) Papillary cystic and solid tumor of the pancreas—surgical therapy with the use of CUSA and review of the pediatric literature. Eur J Pediatr Surg 9:416–419
Lahiri R, Bhattacharya S (2013) Pancreatic trauma. Ann R Coll Surg Engl 95:241–245
Borkon MJ, Morrow SE, Koehler EA, Shyr MS, Hilmes Y, Miller MA, Neblett RS III, Lovorn HL III (2011) Operative intervention for complete pancreatic transection in children sustaining blunt abdominal trauma: revisiting an organ salvage technique. Am Surg 77:612–620
Beres AL, Wales PW, Christison-Lagay ER, McClure ME, Fallat ME, Brindle ME (2013) Non-operative management of high-grade pancreatic trauma: is it worth the wait? J Pediatr Surg 48:1060–1064
Stringer MD (2005) Pancreatic trauma in children. Br J Surg 92:467–470
Leppäniemi AK, Haapiainen RK (1994) Pancreatic trauma with proximal duct injury. Ann Chir Gynecol 83:191–195
Chromik AM, Matthias H. Seeliga MH, Saewe B, Müller ChA, Weyhe D, Felderbauer P, Mittelkötter U, Tannapfel A, Schmidt-Choudhuryd A, Uhl W (2008) Tailored resective pancreatic surgery for pediatric patients with chronic pancreatitis. J Pediatr Surg 43:634–643
O’Rourke RW, Harrison MR (1998) Pancreas divisum and stenosis of the major and minor papillae in an 8-year-old girl: treatment by dual sphincteroplasty J Pediatr Surg 33:789–791
Neblett WW III, O’Neill JA Jr (2000) Surgical management of recurrent pancreatitis in children with pancreas divisum. Ann Surg 231:899–908
Rabinovich A, Rescorla FJ, Howard TI, Grosfeld J, Lillemoe KD (2006) Pancreatic disorders in children: relationship of postoperative morbidity and the indication for surgery. Am Surg 72:641–643
Schlosser W, Rau B, Poch B, Beger B (2005) Surgical treatment of pancreas divisum causing chronic pancreatitis: the outcome benefits of duodenum preserving pancreatic head resection. J Gastrointest Surg 9:710–715
Snajdauf J, Petru O, Nahlovsky J, Rygl M, Frybova B, Bronsky J, Mixa V, Keil R (2018) Pancreas divisum in children and duodenum-preserving resection of the pancreatic head. Eur J Pediatr Surg 28(03):250–254
Pierro A, Nah SA (2011) Surgical management of congenital hyperinsulinism of infancy. Semin Pediatr Surg 20:50–53
Laje P, Stanley ChA, Palladino AA, Becker SA, Adzick NS (2012) Pancreatic head resection and Roux-en-Y pancreaticojejunostomy for the treatment of the focal form of congenital hyperinsulinism. J Pediatr Surg 47:130–135
Obatake M, Mochizuki K, Taura Y, Inamura Y, Nakatomi A, Kinoshita F, Nagayasu T (2012) Pancreatic head resection preserving the main pancreatic duct for congenital hyperinsulinism of infancy. Pediatr Surg Int 28:935–937
Kazez A, Akpolat N, Kocakoç E, Parmaksız ME, Köseoğulları AA (2006) Congenital true pancreatic cyst: a rare case. Diagn Interv Radiol 12:31–33
Al-Salem AH, Matta H (2014) Congenital pancreatic cyst. J Pediatr Gastroenterol Nutr 59:e38–e40
Sukharamwala PB, Patel KD, Teta AF, Parikh S, Ross SB, Ryan CE, Rosemurgy AS (2015) Long-term outcomes favor duodenum-preserving pancreatic head resection over pylorus-preserving pancreaticoduodenectomy for chronic pancreatitis: a meta-analysis and systematic review. Am Surg 81(9):909–914
Jalleh RP, Williamson RCN (1992) Pancreatic exocrine and endocrine function after operations for chronic-pancreatitis. Ann Surg 216:656–662
Klempa I, Spatny M, Menzel J et al (1995) Pancreatic function and quality of life after resection of the head of the pancreas in chronic pancreatitis. A prospective, randomized comparative study after duodenum preserving resection of the head of the pancreas versus Whipple’s operation. Chirurg 66:350–359
Huang JJ, Yeo CJ, Sohn TA et al (2000) Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg 231:890–896
Ishikawa O, Ohigashi H, Eguchi H et al (2004) Long-term follow-up of glucose tolerance function after pancreaticoduodenectomy: comparison between pancreaticogastrostomy and pancreaticojejunostomy. Surgery 136(3):617–623
Rault A, SaCunha A, Klopfenstein D et al (2005) Pancreaticojejunal anastomosis is preferable to pancreaticogastrostomy after pancreaticoduodenectomy for longterm outcomes of pancreatic exocrine function. J Am Coll Surg 201(2):239–244
Nakamura H, Murakami Y, Uemura K et al (2009) Predictive factors for exocrine pancreatic insufficiency after pancreatoduodenectomy with pancreaticogastrostomy. J Gastrointest Surg 13(7):1321–1327
Goess R, Ceyhan G, Friess H (2016) Pancreatic exocrine insufficiency after pancreatic surgery. Panminerva Med 58(2):151–159
Maignan A, Ouaïssi M, Turrini O et al (2018) Risk factors of exocrine and endocrine pancreatic insufficiency after pancreatic resection: a multi-center prospective study. J Visc Surg 155(3):173–181. https://doi.org/10.1016/j.jviscsurg.2017.10.007
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutions involved, in accordance with national ethical standards and with the 1964 Helsinki declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Snajdauf, J., Rygl, M., Petru, O. et al. Indications and outcomes of duodenum-preserving resection of the pancreatic head in children. Pediatr Surg Int 35, 449–455 (2019). https://doi.org/10.1007/s00383-018-4410-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4410-6