Abstract
Purpose
Although the principles of the Ladd’s procedure for intestinal malrotation in children have remained unchanged since its first description, in the era of minimally invasive surgery it is controversial whether laparoscopy is advantageous over open surgery. The aim of our study was to determine whether the surgical approach for the treatment of malrotation had an impact on patient outcome.
Methods
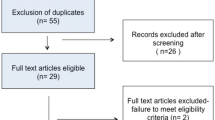
Using a defined strategy (PubMed, Cochrane, Embase and Web of Science MeSH headings), two investigators independently searched for studies comparing open versus laparoscopic Ladd’s procedure in children. Case reports and opinion articles were excluded. Outcome measures included age at operation, time to full enteral feeding, length of hospital stay, and post-operative complications. Maneuvers were compared using Fisher’s exact test and meta-analysis was conducted using RevMan 5.3. Data are expressed as mean ± SD.
Results
Of 308 abstracts screened, 49 full-text articles were analyzed and nine (all retrospective) met our search criteria. Selected articles included 1003 patients, of whom 744 (74 %) underwent open surgery and 259 (26 %) laparoscopy. Patients who had open surgery were younger (0.9 ± 1.2 years) than those who underwent laparoscopy (2.6 ± 3 years; p < 0.0001). Laparoscopy was converted to open Ladd’s in 25.3 % patients. Laparoscopy was associated with faster full enteral feeding (1.5 ± 0.3 days) in comparison to open surgery (4.6 ± 0.1 days, p < 0.0001). Length of hospital stay was shorter in the laparoscopic group (5.9 ± 4.3 days) than in the open group (11.2 ± 6.7 days; p < 0.0001). Open surgery was associated with higher overall post-operative complication rate (21 %) than laparoscopy (8 %; p < 0.0001). Although there was no difference in the prevalence of post-operative bowel obstruction (open, n = 10 %; laparoscopy, n = 0 % p = 0.07), post-operative volvulus was more frequent in the laparoscopy group (3.5 %) than in the open group (1.4 %, p = 0.04).
Conclusion
Comparative but non-randomized studies indicate that laparoscopic Ladd’s procedure is not commonly performed in young children. Although one third of laparoscopic procedures is converted to open surgery, laparoscopy is associated with shorter time to full enteral feeds and length of hospital stay. However, laparoscopic Ladd’s procedure seems to have higher incidence of post-operative volvulus. Prospective randomized studies with long follow-up are needed to confirm present outcome data and determine the safety and effectiveness of the laparoscopic approach.


Similar content being viewed by others
References
Zani A, Pierro A (2017) Intestinal malrotation. In: Puri P (ed) Newborn surgery, 4th edn. CRC Press, Boca Raton, FL (in press)
Zellos A, Zarganis D, Ypsiladis S et al (2012) Malrotation of the intestine and chronic volvulus as a cause of protein-losing enteropathy in infancy. Pediatrics 129(2):e515–e518
Millar AJ, Rode H, Cywes S (2003) Malrotation and volvulus in infancy and childhood. Semin Pediatr Surg 12(4):229–236
Yousefzadeh DK (2009) The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol 39(Suppl 2):S172–S177
Warner B (1997) Malrotation. In: Oldham KT, Colombani PM, Foglia RP (eds) Surgery of infants and children: scientific principles and practice. Lippincott Williams & Wilkins, Philadelphia, pp 12–29
Torres AM, Ziegler MM (1993) Malrotation of the intestine. World J Surg 17(3):326–331
McVay MR, Kokoska ER, Jackson RJ et al (2007) Jack Barney Award. The changing spectrum of intestinal malrotation: diagnosis and management. Am J Surg 194(6):712–717 (discussion 718–719)
Lin JN, Lou CC, Wang KL (1995) Intestinal malrotation and midgut volvulus: a 15-year review. J Formos Med Assoc Taiwan yi zhi 94(4):178–181
Lampl B, Levin TL, Berdon WE et al (2009) Malrotation and midgut volvulus: a historical review and current controversies in diagnosis and management. Pediatr Radiol 39(4):359–366
Ford EG, Senac MO Jr, Srikanth MS et al (1992) Malrotation of the intestine in children. Ann Surg 215(2):172–178
Malek MM, Burd RS (2006) The optimal management of malrotation diagnosed after infancy: a decision analysis. Am J Surg 191(1):45–51
Graziano K, Islam S, Dasgupta R et al (2015) Asymptomatic malrotation: diagnosis and surgical management: an American Pediatric Surgical Association outcomes and evidence based practice committee systematic review. J Pediatr Surg 50(10):1783–1790
Ladd WE (1936) Surgical diseases of the alimentary tract in infants. N Engl J Med 215:705–708
van der Zee DC, Bax NM (1995) Laparoscopic repair of acute volvulus in a neonate with malrotation. Surg Endosc 9(10):1123–1124
Hsiao M, Langer JC (2011) Value of laparoscopy in children with a suspected rotation abnormality on imaging. J Pediatr Surg 46(7):1347–1352
Hagendoorn J, Vieira-Travassos D, van der Zee D (2011) Laparoscopic treatment of intestinal malrotation in neonates and infants: retrospective study. Surg Endosc 25(1):217–220
Bass KD, Rothenberg SS, Chang JH (1998) Laparoscopic Ladd’s procedure in infants with malrotation. J Pediatr Surg 33(2):279–281
Bax NM, van der Zee DC (1998) Laparoscopic treatment of intestinal malrotation in children. Surg Endosc 12(11):1314–1316
Fraser JD, Aguayo P, Sharp SW et al (2009) The role of laparoscopy in the management of malrotation. J Surg Res 156(1):80–82
Palanivelu C, Rangarajan M, Shetty AR et al (2007) Intestinal malrotation with midgut volvulus presenting as acute abdomen in children: value of diagnostic and therapeutic laparoscopy. J Laparoendosc Adv Surg Tech Part A 17(4):490–492
Hsiao M, Langer JC (2012) Surgery for suspected rotation abnormality: selection of open vs laparoscopic surgery using a rational approach. J Pediatr Surg 47(5):904–910
Kozlov YA, Novozhilov VA, Rasputin AA et al (2016) Endoscopic treatment of intestinal malrotation in newborns and infants. Khirurgiia 4:34–39
Miyano G, Fukuzawa H, Morita K et al (2015) Laparoscopic repair of malrotation: what are the indications in neonates and children? J Laparoendosc Adv Surg Tech Part A 25(2):155–158
Ooms N, Matthyssens LE, Draaisma JM et al (2016) Laparoscopic treatment of intestinal malrotation in children. Eur J Pediatr Surg 26(4):376–381
Pearson EG FS, Blinman TA (2013) Laparoscopic Ladd’s procedure is a safe and effective treatment for intestinal malrotation in children with and without volvulus. Paper presented at the American Academy of Pediatrics National Conference, Orlando FL
Stanfill AB, Pearl RH, Kalvakuri K et al (2010) Laparoscopic Ladd’s procedure: treatment of choice for midgut malrotation in infants and children. J Laparoendosc Adv Surg Techn Part A 20(4):369–372
Chen LE, Minkes RK, Langer JC (2003) Laparoscopic versus open surgery for malrotation without volvulus. Pediatr Endosurg Innov Techniques 7(4):433–438
Prasil P, Flageole H, Shaw KS et al (2000) Should malrotation in children be treated differently according to age? J Pediatr Surg 35(5):756–758
Lee HC, Pickard SS, Sridhar S et al (2012) Intestinal malrotation and catastrophic volvulus in infancy. J Emerg Med 43(1):e49–e51
Draus JM Jr, Foley DS, Bond SJ (2007) Laparoscopic Ladd procedure: a minimally invasive approach to malrotation without midgut volvulus. Am Surg 73(7):693–696
Kalfa N, Zamfir C, Lopez M et al (2004) Conditions required for laparoscopic repair of subacute volvulus of the midgut in neonates with intestinal malrotation: 5 cases. Surg Endosc 18(12):1815–1817
Durkin ET, Shaaban AF (2008) Recent advances and controversies in pediatric laparoscopic surgery. Surg Clin N Am 88 (5):1101–1119, viii
Hall NJ, Pacilli M, Eaton S et al (2009) Recovery after open versus laparoscopic pyloromyotomy for pyloric stenosis: a double-blind multicentre randomised controlled trial. Lancet 373(9661):390–398
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Catania, V.D., Lauriti, G., Pierro, A. et al. Open versus laparoscopic approach for intestinal malrotation in infants and children: a systematic review and meta-analysis. Pediatr Surg Int 32, 1157–1164 (2016). https://doi.org/10.1007/s00383-016-3974-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3974-2