Abstract
Background
The significant technological improvement of endoscopic instrumentation has allowed, in the last 10 years, a widespread diffusion of neuroendoscopic procedures. Nevertheless, severe, sometimes life-threatening, complications may occur during neuroendoscopic surgery, and the incidence and age specificity of complications in children have been underdescribed so far.
Materials and methods
Complications recorded in a prospectively collected database of pediatric patients undergoing neuroendoscopic procedures were analysed; the medical histories of the patients and the surgical procedures were reviewed.
Results
Complications occurred in 32 out of 231 (13.8%) procedures performed for the management of obstructive hydrocephalus (137), multiloculated hydrocephalus (53), arachnoid cysts (29) and intraventricular tumors (12). Subdural hygroma occurred in 11 cases, seven requiring subdural shunting. In one of these cases, infection of the subdural space occurred and required a craniotomy. Cerebrospinal fluid (CSF) infection occurred in 11 cases. In one case, a frontal abscess developed and was managed with craniotomy. CSF leak occurred in nine cases, intraventricular haemorrhages in two, technical failures in seven, subcutaneous CSF collection (managed with lumbo-peritoneal shunt) in one, thalamic contusion and post-operative transient akinetic mutism in one. This patient suddenly died 6 months later, probably as a consequence of closure of the stoma. Two patients developed secondary compartmentalisation of the ventricles after complicated endoscopic third ventriculostomy. In nine cases, these complications were associated. Overall, no patient died after the procedure (operative mortality 0), one patient died 6 months after the procedure for unexplained events (sudden death rate 0.4%), and three patients presented permanent disability as a consequence of surgical complication (permanent morbidity 1.3%).
Conclusions
Complication rate of neuro-endoscopic procedures is not negligible even in experienced hands. The majority are minor complications which do not affect the final outcome, but sporadically major events may occur, leading to significant problems in surgical management and, occasionally, to permanent disabilities. Careful selection of patients on pre-operative imaging studies and intensive training of surgeons are mandatory to improve results.
Similar content being viewed by others
Introduction
Despite the increasing use of neuroendoscopy for the treatment of multiple intracranial pathologies in the last decade, the complications of the technique have been the object of few large clinical reports [2, 32, 33, 40]. However, many case reports warn about the occurrence of severe, life-threatening, sometimes fatal, complications of endoscopic approaches [1, 5, 18, 22, 23, 25, 27, 28, 31, 34]. In this paper, we analyse the complications encountered in our series of 231 neuroendoscopic procedures performed in the management of obstructive hydrocephalus, multiloculated hydrocephalus, arachnoid cysts and intraventricular tumours.
Materials and methods
Between September 1999 and December 2005, 231 intracranial endoscopic procedures were performed on 198 patients at Santobono Children’s Hospital in Naples, Italy in the management of different intracranial pathologies: obstructive hydrocephalus (137 procedures), multiloculated hydrocephalus (53 procedures), arachnoid cysts (29 procedures) and intraventricular tumors (12 procedures; Table 1). The clinical outcome of each procedure was classified as follows: complete success (no more operations with the same indication), partial success (success of the procedure with resolution of the primary problem but further procedures necessary during follow up; i.e. repeated septostomies in multiloculated hydrocephalus or subduro-peritoneal shunt for post-operative subdural hygroma), success but re-operation for endoscopic third ventriculostomy (ETV) obstruction (reappearance of primary pathology, managed with repeat endoscopy) and complete failure (shunt implant). The detail of the procedures is shown on Table 1. Complications recorded in a prospectively collected database were analysed; the medical histories of the patients and the surgical procedures were reviewed. The operations were performed by five neurosurgeons. With the exception of the senior author, the surgeons began their experience with endoscopic procedures during the course of this series.
Results
The age of the patients ranged between 1 day and 19 years (mean age 53 months; Fig. 1) Ninety-five procedures (40.7%) were performed in patients in the first year of life. In our series, the success rate was classified as follows: complete success in 140 procedures (60.6%), partial success in 31 procedures (13.4%), success but further surgery for ETV obstruction in 11 cases (4.7%), complete failure in 49 cases (21.2%). In 111 cases, the procedure was simple and straightforward, whereas in 77 cases, two procedures were associated [i.e. ETV + intracranial pressure (ICP) transducer implant]; in 41 cases, three procedures were associated (i.e. ETV + shunt removal + ICP transducer implant), and in two cases, four procedures were associated (i.e. ETV + shunt removal + ICP transducer implant + tumour biopsy).
Unexpected events were recorded in 32 out of 231 procedures (13.8%). Subdural hygroma occurred in 11 cases, seven requiring subdural shunting. CSF infection occurred in 11 cases. CSF leak occurred in nine cases, intraventricular haemorrhages in two, technical failures in seven, subcutaneous CSF collection (managed with lumbo-peritoneal shunt) in one and thalamic contusion and post-operative transient akinetic mutism in one. This patient suddenly died 6 months later, probably as a consequence of closure of the stoma. Two patients developed secondary compartmentalisation of the ventricles after complicated ETV: one after intraventricular haemorrhage, the other after a failed attempt of ETV and subsequent CSF infection. Both patients required further surgical procedures (multiple shunting and endoscopic septa fenestration). Both presented permanent sequelae (epilepsy and severe psychomotor delay in one case and mild psychomotor delay in the other case). In nine cases, these complications were associated. Overall, no patient died after the procedure (operative mortality 0), one patient died 6 months after the procedure for unexplained events (sudden death rate 0.4%), and three patients presented permanent disability as a consequence of surgical complication (permanent morbidity 1.3%). The detail of the complications is shown in Table 2.
Subdural hygroma
The patients who developed subdural hygromas can be divided into two different groups.
In the first group can be included eight patients in the first year of age (range 2–12, mean 4.6, median 3.5). Seven of them had neonatal hydrocephalus related in five cases to aqueductal stenosis, in one case to arachnoid cyst of the quadrigeminal cistern (case 3) and in one case to megacisterna magna (case 8). One patient had severe post-haemorrhagic multiloculated hydrocephalus with isolated fourth ventricle (case 7). Five of them underwent ETV, two ETV + ventriculo-cystostomy, one multiple septostomies and aqueductal cannulation.
In the second group are included three adolescents (13, 15 and 16 years, respectively) all presenting with significant macrocrania and affected in two cases by interhemispheric cysts and hydrocephalus, and in one case by long standing hydrocephalus related with a posterior third ventricle tumor. In the first two patients already described elsewhere [10], the subdural collection developed after neuroendoscopic fenestration of an interhemispheric cyst into the ventricle, probably due to the lack of cortical mantle at the site of introduction of the endoscope. One was managed conservatively; one required transient subduro-peritoneal shunt. The third patient, affected by a third ventricular tumor, underwent a failed attempt of third ventriculostomy (ETV); during the same anaesthesia, the tumor was biopsied and a ventriculoperitoneal (VP) shunt implanted. Thereafter, the patient developed shunt infection and subdural hygroma managed with external drainage. All the shunts were removed after extirpation of the tumour (grade 2 astrocytoma) and microsurgical creation of a third ventriculostomy during the same transcallosal approach. In this case, the cascade of events was more consequence of the decision to implant the shunt during the same procedure after the technical failure of the ETV than of the endoscopic procedure itself.
Overall, in six cases, the subdural hygromas were managed by subduro-peritonal shunts, in one case by external subdural drainage and craniotomy (Fig. 2a–d), in three cases conservatively, in one case removing the shunt and creating a third ventriculostomy in microsurgery. The subduro-peritoneal shunts were removed in all cases after radiological disappearance of the collection (4 to 12 months later; Fig. 3a–c). In this group of patients, the success rate was not different from the overall series, with complete or partial success in 9/11 cases (81%).
CSF infection
CSF infection was defined as a combination of prolonged fever, nuchal rigidity, elevation of C-reactive protein, CSF pleocytosis and positive CSF culture. Overall infection rate of our series was 5% as was observed in 11 patients: in three of them as isolated complication and in another eight patients associated with CSF leak (four), subdural hygroma (three) and after technical failure with secondary compartmentalization of the ventricles (one; Table 2). Microrganisms were isolated in CSF cultures in seven cases: Staphylococcus epidermidis (three), S. aureus (one), Serratia marcescens (one), Escherichia coli + S. epidermidis (one), Pseudomonas aeruginosa + Alcaligenes fecalis (one). The mean age of the patients who developed infection was 35.9 months (range 1 month–15 years, median 6 months). Infection complicated three out of 51 ETV in which no foreign bodies were positioned at the end of the procedure (5.8%) and three out of 94 ETV in which ICP transducer and/or external ventricular drainage were positioned (3.2%). Infection complicated three out of the 53 (5.6%) of the endoscopic procedures performed for the management of multiloculated hydrocephalus; one out of 29 (3.4%) of the procedures for arachnoid cysts and one out of 12 (8.3%) of the procedures for intraventricular tumours. There is no significant difference in the rate of infection among these groups. Nine cases of CSF infection were managed with external drainage and antibiotics, two with antibiotics alone. Permanent sequelae directly related to infection were observed in two cases. In the first (case 13), a patient already affected by multiloculated post-haemorrhagic hydrocephalus of prematurity underwent an endoscopic septostomy that was complicated by CSF infection: In the long term, the patient presented developmental delay and seizures. In the second, a 4-month-old girl affected by aqueductal stenosis (case 14) underwent an uneventful ETV. Two months later, she was readmitted with bulging fontanel and magnetic resonance imaging pattern of ETV obstruction. ETV was re-attempted, but failed because of diffuse arachnoid scarring at the level of the interpeduncular and pre-pontine cistern. In the post-operative period, she developed CSF infection with ventriculitis and secondary loculation, requiring three more procedures for endoscopic septum fenestration and implant of a complex shunt system (Fig. 4). She also needed anti-epileptic medication and presented mild psychomotor delay.
Haemorrhages
Haemorrhagic complications occurred in two procedures (0.9%).
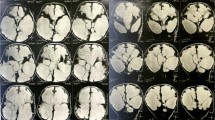
A 4-day-old baby girl (case 32) affected by obstructive tetraventricular hydrocephalus (Fig. 5a) underwent ETV that was complicated by a major bleeding from a subependymal vein near the cortical tract of the endoscope. The procedure was completed, but bleeding did not stop despite irrigation. At the end of the procedure, an external drainage was left in situ. Post-operative computed tomography (CT) scan showed intraventricular haemorrhage with subependymal haematoma at the level of the right thalamus (Fig. 5b). CSF eventually cleared, and a VP shunt was implanted 3 weeks later (Fig. 5c). The patient presents a normal psychomotor development at 12 months of follow-up.
Case 32: a Sagittal T1 MRI showing obstructive tetraventricular hydrocephalus. b Post-operative CT scan performed 2 h after ETV showing subependymal bleeding with intraventricular hematoma. c Follow-up CT scan performed at the age of 3 months. The valve is visible in the right parieto-occipital region
In the second case, a 19-day-old newborn diagnosed with congenital posterior fossa tumour and hydrocephalus underwent ETV that was complicated by a minor bleeding from the cortical tract of the endoscope, easily controlled with irrigation (case 31). The procedure was completed uneventfully, and a closed external drainage was left in the ventricular system. In the following hours, the baby became drowsy, with a bulging fontanel. A CT scan showed an intraventricular haemorrhage (Fig. 6a). He developed multiloculated hydrocephalus (Fig. 6b) which required several shunt procedures and infantile spasms, which required three-drug treatment. The patient finally underwent complete removal of a IV ventricle choroids plexus papilloma and presents significant developmental delay at 4-year follow-up.
Technical failure
Impossibility to complete the planned procedure occurred in seven cases (3.2%). In six of them, the planned ETV was not completed for anatomical reasons: In one case, the floor was too thick (case 9), in two cases at primary ETV in newborns, the subarachnoid spaces could not be identified after floor perforation (cases 22–24), in two cases of repeated ETV in newborns, subarachnoid spaces were found occupied by dense scarring (cases 14–20), in one case of shunt malfunction in a 6-year-old, myelomeningocele (case 23) dense fibrous tissue was found in the subarachnoid space after perforation of the third ventricular floor (Fig. 7). In case 21, the septostomy planned for a myelomeningocele affected by multiloculated hydrocephalus was abandoned because anatomy was not considered suitable to complete the procedure.
Case 23: 6-year-old girl affected by myelomeningocele presenting with shunt malfunction. Retrospectively, abnormal intensity tissue can be identified at the level of the interpeduncular cistern below the third ventricular floor. Clear identification of the subarachnoid spaces was impossible after floor perforation; the procedure was abandoned and the shunt revised uneventfully
In five cases, the technical failure did not bear any consequence, in two cases (cases 9–14), the failure was followed by subsequent complications as already described.
CSF leak
CSF leak from the surgical wound occurred in nine cases (3.9%). Eight were ETV procedures, and one was a septostomy. In four cases, CSF leak was associated with CSF infection: Three of them remained shunt-free after resolution of the infection; the fourth was shunted. In the remaining five cases, CSF leak was a sign of failure of the procedure, and a VP shunt was inserted uneventfully.
Subcutaneous CSF collection
Subcutaneous CSF collection developed in a baby affected by an interhemispheric cyst and who underwent endoscopic cyst-ventriculostomy and cyst-cisternostomy. The patient, already reported elsewhere [10], was managed with multiple lumbar punctures and, finally, implantation of lumbo-peritoneal shunt because of recurrence of the collection. The shunt was removed uneventfully 12 months later.
Secondary compartmentalisation
Secondary compartmentalisation occurred in two patients described above (cases 14–31) and was consecutive to significant intraventricular haematoma in one case and to ventriculitis after CSF infection in the other. This complication should be considered as the most dangerous for the final outcome and the most difficult to treat because of the need for multiple procedures to treat the asynchrone development of the cavities. Case 31 was the patient who suffered the most serious clinical consequences of a complicated neuroendoscopic procedure in our series.
Sudden death
Patient 19, affected by aqueductal stenosis and shunted at birth, was admitted at the age of 8 years for shunt malfunction with mild ventricular dilatation. During ETV, the right lateral ventricle was cannulated at the third attempt, and blood-stained CSF was rapidly cleared by warm Ringer lactate irrigation. ETV was performed, the shunt was removed and EVD with ICP monitoring was implanted. Post-operative CT scan revealed right thalamic contusion, and the patient presented CSF infection that was managed by EVD opening and antibiotics. He also presented akinetic mutism that completely resolved after 2 weeks. On resolution of CSF infection, the EVD was removed, and the patient was discharged with a normal neurological exam and normal size ventricles. The family of the patient did not attend the proposed outpatient follow-up, and 6 months later, the patient was found dead in his bed one morning by the parents. He had not complained of headache nor had he presented signs or symptoms related with intracranial hypertension in the previous days. Autopsy was not performed.
Discussion
The reported complication rate of endoscopic procedures ranges between 0 and 20% [11, 32], but it is felt among the neurosurgical community that the real complication rate may be higher than that published [32, 40, 42]. In the 19 endoscopic series reviewed by Schroeder et al. [32], only in five did the complication rate exceed 10%, and only in one 15%. We did not encounter disastrous intraoperative complications such as lesions of the basilar artery or its branches, but a high rate of post-operative complications that include post-operative subdural effusions (5%), CSF infections (5%) and CSF leaks (3,9%). We have also considered, as complication of endoscopy, the technical failures.
Mortality
The mortality rate of endoscopic procedures is under 1% in most series [17, 32, 41]. This incidence is comparable to the very low one observed for extrathecal shunts (0.1%) [12]. Death usually occurs after catastrophic bleedings from large vessels or, less frequently, because of severe secondary complications (infections) in patients with poor clinical conditions [32, 36].
In our series, a patient suddenly died 6 months after a complicated endoscopic procedure. Considering the circumstances of this event, with lack of any warning signs in the hours preceding the adverse event, the lack of paraclinical or radiological examination and the absence of autopsy findings, the pathophysiology of this event will remain speculative. Although acute hydrocephalus due to ETV obstruction remains the most likely explanation, the report of this case will hardly be contributive to the understanding of the phenomenon of sudden death as late complication of ETV.
Deaths after late closure of the fenestrated floor of the third ventricle have been reported by an increasing number of authors even 7 years after the operation; however, such risk appears to be low [1, 16, 18, 19]. Neuropathological examinations in the cases reported by Hader et al. [16] showed the presence of arachnoid and glial scarring in the floor of the third ventricle, confirming that the ETV obstruction should be considered responsible for acute increase of intracranial pressure and death. The reasons for the rapid progression of the symptoms (<24 h) and subsequent deaths in some cases are unclear; however, the complete blockage of flow at the orifice and the presence of non-compliant brain (especially in previously shunted patients) may play an important role [16]. Moreover, symptoms of increased ICP can be often underappreciated due to a false feeling of security on the part of family and caregivers because the absence of a shunt and the false belief that the hydrocephalus has been definitively cured contributes to this fatal complications [16]. Predicting which patients may be at risk for later failure after successful third ventriculostomy is difficult. However, routine imaging may be important to identify patients with asymptomatic increases in ventricular size and those with an absent flow void (on T2-weighted MR imaging or cine phase-contrast imaging) who may be at risk for delayed failure [7, 16]. To reduce mortality associated with late failure of ETV, Mobbs et al. [26] suggested to leave a ventricular catheter and a subcutaneous reservoir at the end of the procedure to allow urgent access to the ventricular system, in selected cases, when patients do not have ready access to a neurosurgical department. Anyway, the association between ETV failure and sudden death is probably not related to the technique itself but to the kind of patients (obstructive triventricular hydrocephalus) that are most frequently treated by ETV. These patients are, in fact, prone to sudden deterioration, and similar episodes have been described when these patients were only treated by VP shunt during shunt malfunction [20, 24, 30, 39].
Intraoperative complications
Haemorrhages are the most worrisome complications in neuroendoscopy because of the difficulty in obtaining haemostasis with the endoscopic instrumentation: As suggested by Walker [42], irrigation and patience are the most important methods for achieving hemostasis in endoscopic neurosurgery.
Teo et al. [41] reported “clinically insignificant” haemorrhage in six out of 55 endoscopic ventriculostomies. Of 98 cases, Hopf et al. [17] reported venous bleeding in three cases, arterial bleeding in one case and bleeding from a bridging vein during the opening in another case. In our series, significant intraoperative haemorrhages occurred in two procedures (0.9%), with significant clinical sequelae for one of them.
Intraventricular bleeding from the small subependymal vessels, due to traumatic injuries caused by the impact with the endoscopic instrumentation, is the most frequent reported haemorrhagic complication [2, 6, 7, 14, 15]. Usually, it is a non-significant complication that can be easily managed by irrigation or through a prudent coagulation of the bleeding vessel. On the contrary, haemorrhages from larger veins, such as hypothalamic, thalamostriate or septal veins, sometimes make the irrigation ineffective, so affecting the operative visibility and the possibility to perform a safe electrocoagulation. In these cases, the procedure should be abandoned and an extracranial CSF drainage placed [7, 11, 42]. In some instances, the venous bleeding results in a subependymal clot that may clear up spontaneously without the need to abort the surgical procedure [31].
The damage of large vascular structures is rare, occurring in about 1% of ETVs [1, 23, 25, 32, 34]. This is, in fact, the endoscopic procedure more at risk to compromise the important vessels of the interpeduncolar cistern: the basilar, posterior cerebral or posterior communicating arteries. After arterial injury, fatal major haemorrhage, vasospasm, pseudoaneurysm and delayed subarachnoid haemorrhage have been reported, with significant morbidity and mortality [42]. An unfavourable anatomy (small or too thick or excessively elastic floor of the third ventricle) and a poor intraoperative visibility are important risk factors [11, 40, 42]. Basilar artery perforation appears as a brisk intraventricular bloody flooding that suddenly obscures the operating field. The management consists of quick removal of the endoscope and placement of an external ventricular drain through which a copious irrigation must be performed until the bleeding is arrested. A cerebral angiogram should be obtained within 1 to 3 days of any significant haemorrhage to rule out the presence of a pseudoaneurysm [42]. This can be successfully managed with craniotomy and surgical exclusion [1, 25] or endovascular techniques [23].
Proper placement of the fenestration halfway between the infundibular recess and the mammillary bodies in the midline; close inspection of a sagittal MR image to determine the relationship between the basilar artery and the floor of the third ventricle; avoidance of laser, cautery and other forms of energy in fenestrating the floor; use of a rigid, pointed (but not sharp) instrument to achieve the initial perforation (to avoid the instrument to slip on one side) and abandoning the procedure if intraoperative conditions, such as bleeding, unfavourable anatomy, make the fenestration too risky are simple recommendations to avoid injuries of arterial vessels [34, 40, 42].
The rate of abandoning procedures has been reported to range from 0 to 26% [11]. The reasons for abandoning have mainly been haemorrhages, anatomical variations and inability to perform the fenestration of the floor [4, 7, 17, 41]. Most failures occur in patients with myelomeningocele and Chiari malformation, in which a large massa intermedia may hide the floor of the third ventricle and in patients who suffered ventriculitis, because the surgical landmarks may become unrecognizable. In our series, seven procedures (ETV) were aborted: To avoid more severe intraoperative complications, our policy is not to hesitate converting the endoscopic procedure into a shunt procedure.
Other intraoperative complications such as hypothalamic injury, oculomotor palsy and severe bradycardia during floor perforation are uniquely dependent upon the technique used for floor perforation and only reported by authors who use the whole endoscope to perforate the floor, thus, performing significant tractions on the hypothalamus [13]. Contusion of the fornix and mammillary bodies with subsequent memory disturbances; brain herniation syndrome (resulting from intraventricular over-irrigation or sudden resolution of the hydrocephalus in patients with posterior fossa tumours with subsequent upward herniation [4, 32] did not occur in our series.
Post-operative complications: subdural hygroma
The appearance of subdural collections in the post-operative period has been the most frequent complication in our series, occurring in 5% of the cases. The procedures with the higher risk to develop such complications have been ETV and fenestration of arachnoid cysts in newborns. Most of the patients who developed subdural hygromas were younger than 1 year (Table 2). The two children who developed subdural effusions after arachnoid cyst fenestration (without ETV) were adolescents with significant macrocrania. This complication has not been frequently reported in the literature in which its incidence did not exceed 2% [2, 21, 32, 33].
The pathophysiological mechanism of formation probably includes two main factors: sudden decrease of ventricular volume induced by abrupt drainage of CSF during ETV [3, 35] and the creation of a large parenchymal tract into the frontal lobe in children who often present a thin cortical mantle. The progressive decrease of the ventricular volume due to the functioning ETV and the constant filling of the subdural space through the cortical tract are two additional factors that contribute to the persistence and progression of the subdural collection. Moreover, it has been demonstrated that the absorptive mechanisms need a few days to be able to absorb the whole amount of CSF entering the subarachnoid spaces through the ETV [10, 29] so that CSF tries to escape through the pathway of least resistance [40]. If the absorptive mechanisms fail, the patients will require extracranial CSF diversion. However, in our series, we did not observe a higher rate of failure in patients who developed subdural hygromas even if the collections were progressive and needed shunting. In fact, most subduro-peritoneal shunts had been uneventfully removed after radiographic disappearance of the collections.
Alternative pathogenetic hypothesis is that acute and chronic subdural haematomas, after injury of bridging veins secondary to abrupt drainage of CSF, have been reported [3, 27, 35]. Significant ventricular dilatation with a thin cortical mantle, especially in children, is a risk factor for subdural effusions and hemorrhage [42].
Teo [40] proposed a protocol to reduce this complication: expansion of the ventricles before removing the sheath from the lateral ventricle, plugging the cortical hole with a piece of gelfoam, avoiding lumbar and ventricular drainage in the post-operative period. With this protocol, he did not observe subdural collections in more than 350 procedures [40]. In case of arachnoid cysts, Schroeder et al. [33] recommend not to detach the outer wall of the cyst from the dura mater, which may result in collapse of the cyst and subdural/subcutaneous collections.
CSF infection
The infection rate of our series (4.7%), although high, remains within the limits of what is reported in the literature (1 to 5%) [2, 33, 41]. CSF infection was the most significant complications in our series: in the group of 11 patients who experienced infection, there was one death (sudden death 6 months after the procedure), two secondary compartmentalisation of the ventricular system with further surgery and permanent sequelae (seizures and neurodevelopmental delay) in both.
The risk of arachnoiditis and consequent obliteration of the CSF pathways after CSF infection is high [38]. In our series, nine procedures completely failed, one had to be repeated twice, and one was initially successful, but the patient died 6 months later. Actually, post-operative meningitis resulted as an independent risk factor of failure of ETV from the multivariate analysis of Fukuhara et al. [14].
On the contrary, we did not observe an increase in infection rate when an EVD or an ICP transducer was positioned at the end of ETV. Infection rate of endoscopic procedures remain lower than that of extrathecal shunts that range from 1 to 40% (mean 8.5%) in the literature [11, 43].
CSF leak
CSF leak and subgaleal CSF collection over the burr hole are well-described complications of ETV [11, 15, 32, 41], especially in infants (thin skin, immature subarachnoid spaces) [40]. Although in many cases they can be successfully managed by intermittent tapping from lumbar or ventricular drainage [8, 9, 37], revealing the possibility of a gradual adaptation of the CSF hydrodynamics to the ETV [29], this type of complication represents a risk factor for infections and, in particular, it may be the early sign of failure of the procedure and need of shunt placement. In our series, four developed CSF infection and five did not. The patient who presented subcutaneous CSF collection was unsuccessfully managed with repeated lumbar punctures followed by lumbo-peritoneal shunt. This was uneventfully removed 1 year later.
The possibility of a CSF leak may be minimised using the smallest appropriate endoscope (especially in patients with large ventricles) and by minimising the dural opening [42]. Teo [40] recommends plugging the cortical tract at the end of the procedure with Gelfoam (UpJohn, Kalamazoo) and closing the wound in a water-tight fashion. Moreover, in the post-operative period, the patient should be kept as upright as possible to reduce the CSF pressure on the wound and decrease the sagittal sinus pressure, encouraging the absorption of CSF across the villi into the sagittal sinus [40]. In newborns, we propose to perform a linear incision of the dura to allow watertight closure of the dura itself at the end of the procedure, careful subcutaneous layer and watertight mattress suture of the skin [8].
Conclusion
Even if the complication rate of endoscopic procedures has been reported to be low, it should not be considered negligible, at least in children. In fact, in children, an increased number of post-operative complications, such as subdural collections, CSF leaks and CSF infections, have to be expected. Some of these, especially CSF infection, significantly affect the outcome. Careful selection of patients on pre-operative imaging studies and intensive training of surgeons are mandatory to improve results.
References
Abtin K, Thompson BG, Walker ML (1998) Basilar artery perforation as a complication of endoscopic third ventriculostomy. Pediatr Neurosurg 28:35–41
Beems T, Grotenhuis JA (2004) Long term complications and definition of failures of neuroendoscopic procedures. Childs Nerv Syst 20:868–877
Beni-Adani L, Siomin V, Segev Y, Beni S, Constantini S (2000) Increasing chronic subdural haematoma after endoscopic III ventriculostomy. Childs Nerv Syst 16:402–405
Brockmeyer D, Abtin K, Carey L, Walker M (1998) Endoscopic third ventriculostomy: an outcome analysis. Pediatr Neurosurg 28:236–240
Buxton N, Punt J (2000) Cerebral infarction after neuroendoscopic third ventriculostomy: case report. Neurosurgery 46:999–1002
Choi JU, Kim DS, Kim SH (1999) Endoscopic surgery for obstructive hydrocephalus. Yonsei Med J 40:600–607
Cinalli G, Sainte-Rose C, Chumas P, Zerah M, Brunelle F, Lot G, Pierre-Kahn A, Renier D (1999) Failure of third ventriculostomy in the treatment of aqueductal stenosis in children. J Neurosurg 90:448–454
Cinalli G (2004) Endoscopic third ventriculostomy. In: Cinalli G, Maixner WJ, Sainte-Rose C (eds) Pediatric hydrocephalus. Springer, Milan, Italy
Cinalli G, Spennato P, Ruggiero C, Aliberti F, Zerah M, Trischitta V, Cianciulli E (2006) Intracranial pressure monitoring and lumbar puncture following endoscopic third ventriculostomy in children. Neurosurgery 58:126–136
Cinalli G, Peretta P, Spennato P, Savarese L, Varone A, Vedova P, Grimaldi G, Ragazzi P, Ruggiero C, Cianciulli C, Maggi G (2006) Neuroendoscopic management of interhemispheric cysts in children. J Neurosurg 105:194–202
Di Rocco C, Cinalli G, Massimi L, Spennato P, Cianciulli E, Tamburrini G (2006) Endoscopic third ventriculostomy in the treatment of hydrocephalus in pediatric patients. In: ickard JD (ed) Advances and technical standards in neurosurgery, vol 31. Springer, Wien, pp 119–219
Di Rocco C, Marchese E, Velardi F (1994) A survey of the first complication of newly implanted CSF shunt devices for the treatment of nontumoral hydrocephalus. Cooperative survey of the 1991–1992 Education Committee of the ISPN. Childs Nerv Syst 10:312–327
El-Dawlatly AA, Murshid WR, Elshimy A, Magboul MA, Samarkandi A, Takrouri MS (2000) The incidence of bradycardia during endoscopic third ventriculostomy. Anesth Analg 91:1142–1144
Fukuhara T, Vorster SJ, Luciano MG (2000) Risk factors for failure of endoscopic third ventriculostomy for obstructive hydrocephalus. Neurosurgery 46:1100–1111
Gangemi M, Donati P, Maiuri F, Longatti P, Godano U, Mascari C (1999) Endoscopic third ventriculostomy for hydrocephalus. Minim Invasive Neurosurg 42:128–132
Hader WJ, Drake J, Cochrane D, Sparrow O, Johnson ES, Kestle J (2002) Death after late failure of third ventriculostomy in children. J Neurosurg 97:211–215
Hopf NJ, Grunert P, Fries G, Resch KDM, Perneczky A (1999) Endoscopic third ventriculostomy: outcome analysis of 100 consecutive procedures. Neurosurgery 44:795–806
Javadpour M, May P, Mallucci C (2003) Sudden death secondary to delayed closure of endoscopic third ventriculostomy. Br J Neurosurg 17:266–269
Jones RFC, Kwok BCT, Stening WA (1996) Endoscopic III ventriculostomy. How long does it last? Childs Nerv Syst 12:364–365
Johnson DL, Fitz C, McCullough DC, Schwarz S (1986) Perimesencephalic cistern obliteration: a CT sign of life-threatening shunt failure. J Neurosurg 64:386–389
Kamel MH, Murphy M, Aquilina K, Marks C (2006) Subdural hemorrhage following endoscopic third ventriculostomy. A rare complication. Acta Neurochir (Wien) 148:591–593
Kumar R, Behari S, Wahi J et al (1999) Peduncular hallucinosis: an unusual sequel to surgical intervention in the suprasellar region. Br J Neurosurg 13:500–503
Lenthall LK, Cinalli G, Rodesch G, Lasjaunias PL (1999) Endovascular management of a traumatic basilar tip aneurism following endoscopic ventriculostomy in a child. Interv Neuroradiol 5:57–60
Mc Donnell GV, Mc Cann JP (2000) Why do adults with spina bifida and hydrocephalus die? A clinic base study. Eur J Pediatr Surg 10(Suppl)1:31–32
McLaughlin M, Wahlig J, Kaufman A, Albright A (1997) Traumatic basilar aneurysm after endoscopic third ventriculostomy: case report. Neurosurgery 41:1400–1403
Mobbs RJ, Vonau M, Davies MA (2003) Death after late failure of endoscopic third ventriculostomy: a potential solution. Neurosurgery 53:384–386
Mohanty A, Anandh B, Reddy MS et al (1997) Contralateral massive acute subdural collection after endoscopic third ventriculostomy—a case report. Minim Invasive Neurosurg 40:59–61
Navarro R, Gil-Parra R, Reitman AJ, Olavarria G, Grant JA, Tomita T (2006) Endoscopic third ventriculostomy in children: early and late complications and their avoidance. Childs Nerv Syst 22:506–513
Nishiyama K, Mori H, Tanaka R (2003) Changes in cerebrospinal fluid hydrodynamics following endoscopic third ventriculostomy for shunt-dependent noncommunicating hydrocephalus. J Neurosurg 98:1027–1031
Peretta P, Cinalli G, Spennato P, Ragazzi P, Ruggiero C, Aliberti F, Carlino C, Cianciulli E, Maggi G (2007) Long term results of secondary ETV in children. Retrospective analysis of 40 cases. J Neurosurg (in press)
Schönauer C, Bellotti A, Tessitore E, Parlato C, Moraci A (2000) Traumatic subependymal hematoma during endoscopic third ventriculostomy in a patient with a third ventricle tumor: case report. Minim Invasive Neurosurg 43:135–137
Schroeder HWS, Niendorf W-R, Gaab MR (2002) Complications of endoscopic third ventriculostomy. J Neurosurg 96:1032–1040
Schroeder HWS, Oertel J, Gaab MR (2004) Incidence of complications in neuroendoscopic surgery. Childs Nerv Syst 20:878–883
Schroeder HWS, Warzok RW, Assaf JA, Gaab MR (1999) Fatal subarachnoid hemorrhage after endoscopic third ventriculostomy. Case report. J Neurosurg 90:153–155
Sgaramella E, Castelli G, Sotgiu S (2004) Chronic subdural collection after endoscopic third ventriculostomy. Acta Neurochir (Wien) 146:529–530
Singh D, Gupta V, Goyal A, Singh H, Sinha S, Singh AK, Kumar S (2003) Endoscopic third ventriculostomy in obstructed hydrocephalus. Neurol India 51:39–42
Siomin V, Cinalli G, Grotenhuis A, Golash A, Oi S, Kothbauer K, Weiner H, Roth J, Beni-Adani L, Pierre-Kahn A, Takahashi M, Mallucci C, Abbott R, Wisoff J, Constantini S (2002) Endoscopic third ventriculostomy for patients with cerebrospinal fluid infections and/or hemorrhage. J Neurosurg 97:519–524
Spennato P, Cinalli G, Carannante G, Ruggiero C, Del Basso De Caro ML (2004) Multiloculate hydrocephalus. In: Cinalli G, Maixner J, Saint-Rose C (eds) Pediatric hydrocephalus. Springer, Milan, pp 219–244
Staal MJ, Meihuizen-de Regt MJ, Hess J (1987) Sudden death in hydrocephalic spina bifida aperta patients. Pediatr Neurosci 13(1):13–18
Teo C (2004) Complications of endoscopic third ventriculostomy. In: Cinalli G, Maixner J, Saint-Rose C (eds) Pediatric hydrocephalus, Springer, Milan, pp 411–420
Teo C, Rahman S, Boop FA, Cherny B (1996) Complications of endoscopic neurosurgery. Childs Nerv Syst 12:248–253
Walker ML (2004) Complications of third ventriculostomy. Neurosurg Clin N Am 15:61–66
Whitehead WE, Kestle JRW (2001) The treatment of cerebrospinal fluid shunt infections. Pediatr Neurosurg 35:205–210
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cinalli, G., Spennato, P., Ruggiero, C. et al. Complications following endoscopic intracranial procedures in children. Childs Nerv Syst 23, 633–644 (2007). https://doi.org/10.1007/s00381-007-0333-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-007-0333-6