Abstract
Purpose
Determining the frequency and distribution of pathogenic germline variants (PGVs) in Austrian prostate cancer (PCa) patients and to assess the accuracy of different clinical risk scores to correctly predict PGVs.
Methods
This cross-sectional study included 313 men with advanced PCa. A comprehensive personal and family history was obtained based on predefined questionnaires. Germline DNA sequencing was performed between 2019 and 2021 irrespective of family history, metastatic or castration status or age at diagnosis. Clinical risk scores for hereditary cancer syndromes were evaluated and a PCa-specific score was developed to assess the presence of PGVs.
Results
PGV presence was associated with metastasis (p = 0.047) and castration resistance (p = 0.011), but not with personal cancer history or with relatives with any type of cancer. Clinical risk scores (Manchester score, PREMM5 score, Amsterdam II criteria or Johns Hopkins criteria) showed low sensitivities (3.3–20%) for assessing the probability of PGV presence. A score specifically designed for PCa patients stratifying patients into low- or high-risk regarding PGV probability, correctly classified all PGV carriers as high-risk, whereas a third of PCa patients without PGVs was classified as low risk of the presence of PGVs.
Conclusion
Application of common clinical risk scores based on family history are not suitable to identify PCa patients with high PGV probabilities. A PCa-specific score stratified PCa patients into low- or high-risk of PGV presence with sufficient accuracy, and germline DNA sequencing may be omitted in patients with a low score. Further studies are needed to evaluate the score.
Similar content being viewed by others
Introduction
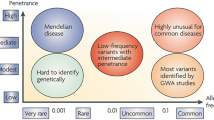
Approximately 12% of patients with metastatic prostate cancer (PCa) harbor a PGV in genes involved in homologous DNA repair or mismatch repair such as BRCA1, BRCA2, ATM, MSH2, or other DNA damage repair (DDR) genes [1]. The presence of PGVs, in particular in BRCA2, is associated with a more aggressive disease behavior as well as a poorer prognosis, which is also reflected by a higher Gleason grade, a younger age, a more advanced disease stage at diagnosis, and lower survival rates [2,3,4,5]. While molecular profiling of localized PCa tumors with pathogenic BRCA2 variants has shown an increased genomic instability and a mutational profile similar to metastatic disease [6], the impact of other PGVs on PCa is less well understood. Identification of PGV carriers with PCa is not only important for regular cancer screening or family cascade testing, but can offer the possibility for additional therapy options, such as PARP- or checkpoint inhibitors. Currently, several recommendations for germline testing in PCa patients are available, which take clinical features but also personal and family history into account [7,8,9]. For example, the European Association of Urology (EAU) PCa guideline from 2022 considers germline testing in men with metastatic PCa, men < 60 years with high-risk PCa, or family members with PCa [8]. However, this results in substantial overtesting. Currently, no available score predicts the presence of PGVs in PCa patients with positive family histories. For other tumor predisposition syndromes, such as hereditary breast and ovarian cancer (HBOC) caused by PGVs in BRCA1/2 or for Lynch syndrome (LS) caused by DNA mismatch repair alterations, criteria and risk scores based on family history determine the probability of underlying PGVs and help select patients for germline testing. Examples comprise the Manchester scoring system, identifying patients with a > 10% probability of PGVs in BRCA1/2 [10], the Amsterdam II criteria and the PREMM5 score, predicting the probability of underlying LS-associated gene alterations [11, 12], or the Johns Hopkins criteria to identify hereditary PCa families to offer early screening [13].
In summary, none of the existing scores or clinical criteria have been specifically evaluated in PCa patients. This study aimed to test the performance of these criteria and to develop a novel PCa-specific score based on personal and family cancer history to identify PCa patients with low or high probability for PGV presence.
Materials and methods
Patients
Patients with PCa treated at the Department of Urology of the Medical University of Vienna between 2019 and 2021 were offered germline genetic testing based on the National Comprehensive Cancer Network (NCCN) guidelines including high-grade localized or metastatic PCa [9]. Demographic and clinical data were collected from clinical documentation. Family history was patient-reported and obtained by questionnaires (Supplement 1 and 2). Patients were unselected regarding personal or family history and age at onset. All patients provided written informed consent and local ethics committee approved the study (EK-Nr: 1043/2020).
Multi-gene panel sequencing and bioinformatics analysis
DNA extraction from EDTA-blood samples according to standard protocols as well as sequencing were performed at the Institute of Medical Genetics of the Medical University of Vienna. Multi-gene panel testing was enriched for genes associated with PCa by the custom designed „Prostate-Carcinoma-Panel V1 “ (PCa panel) from Illumina (San Diego, California, USA). The PCa panel included 25 genes: ATM, ATR, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, EPCAM, FAM175A (ABRAXAS1), FANCA, GEN1, MLH1, MLH3, MRE11A, MSH2, MSH6, NBN, PALB2, PMS2, PRAC2, PTEN, RAD51C, RAD51D, STK11 and TP53. This multi-gene panel was designed based on commonly used gene panels and frequently altered genes described in recent literature [1, 14,15,16,17].
Reported variants were reported as likely pathogenic and pathogenic variants or variants of uncertain significance (VUS) [18]. All reported variants were confirmed by Sanger sequencing (detailed in Supplement 3).
Statistics and score evaluation
Descriptive statistics were used to analyze patient characteristics. Associations between PGVs and clinical features were examined using Chi-square and t test. p values < 0.05 (two-tailed) were considered significant. The Manchester score was calculated and counted positive if > 14 (unadjusted for tumor biology) [10]. Johns Hopkins criteria were fulfilled if the patient met one criteria [13]. Amsterdam II criteria were considered fulfilled if the patient met all criteria [11]. The PREMM5 score was calculated using the online platform (https://premm.dfci.harvard.edu/) and considered positive, if the overall predicted probability for LS was ≥ 2.5% (Tables S1–3) [12]. The individual scores were used to calculate sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy for presence of PGVs.
For PCa-specific score development, the variables were chosen based on clinical observations relevant for interpreting patients’ family pedigrees in routine genetic counseling. These variables comprised (i) personal history of gastrointestinal or male breast cancer, (ii) first-degree relatives with a history of gastrointestinal, breast, endometrial, ovarian or PCa, (iii) < 5 first-degree relatives with cancer histories available for assessment, (iv) personal history of cancer, and (v) second-degree relatives with history of gastrointestinal, breast, endometrial, ovarian or PCa (Table S4).
The variables were tested by logistic regression analysis, and variables with p values with < 0.15 and regression coefficients > 0.5 were considered significant for inclusion for further regression analysis [corresponding to variables (i), (ii), and (iii)]. They were included in a receiver operating characteristic (ROC)-curve to calculate the score’s cut-off. A cut-off of ≥ 0.917 resulted in highest sensitivity and specificity (Table S5).
To simplify the model, points for the PCa score were assigned by rounding the value of the regression coefficients for variables (i), (ii) and (iii) from the stepwise logistic regression to 1. The pretest probability for presence of PGVs was considered high if the score was ≥ 1.
All analyses were conducted with IBM SPSS-software version 23.
Results
In this cross-sectional study, 313 men underwent germline genetic testing for 25 genes and were interviewed for personal and family history. The ethnicity was primarily Caucasian, the median age at PCa diagnosis was 64 years (42–83 years). At the time of enrollment, 78 patients had localized, non-metastatic PCa, and 235 had metastatic PCa, of whom 34.9% (n = 82) had de novo metastatic PCa. The majority of the patients were castration resistant (61.8%). In 30 patients (9.6%), an underlying PGV could be identified. Ethnicity, age, initial PSA values or ISUP grading at PCa diagnosis did not correlate with the occurrence of any PGVs, but the proportion of patients with metastasized or castration-resistant PCa was significantly higher in the group of patients with PGVs (p = 0.047, p = 0.011, respectively) (Table 1).
VUS were detected in 50 (16%) patients, and in 233 (74.4%) patients neither PGVs nor VUS were detected. The most frequent PGVs were found in BRCA2 (n = 12), CHEK2 (n = 5) and ATM (n = 4) (Fig. 1).
Regarding prior personal history, 54 patients (17.3%) had a personal history of at least one additional cancers, including basalioma, melanoma, colorectal carcinoma, urothelial carcinoma of the bladder, squamous cell carcinoma of the skin or upper tract urothelial cancer. Patients with or without PGVs did not display significant differences with regard to any personal cancer history (p = 0.708) (Table S6).
Most patients had at least one relative with any type of cancer diagnosis (74%, n = 234). In total, 68 relatives had been diagnosed with colorectal cancer, 60 with PCa, 52 with breast cancer and 20 with pancreatic cancer. There were no statistically significant differences regarding positive family history between patients with or without PGVs. Furthermore, the total number of relevant tumors (i.e., prostate, colon, upper urinary tract, pancreatic, breast, endometrial or ovarian cancer) (Table S7).
Next, we tested the performance of clinical criteria relying on positive family history for HBOC (Manchester score), LS-associated cancer (Amsterdam II criteria, PREMM5 score), or PCa (Johns Hopkins criteria) in indentifying PCa patients with high probabilities for underlying PGVs in BRCA1/2 (n = 14) or DNA mismatch repair genes (n = 3). In the entire cohort, three patients (1%) had a positive Manchester score, and only one out of 14 patients with a PGV in BRCA1/2 had a positive Manchester score. Ten patients (3.2%) fulfilled the Johns Hopkins criteria, and only one out of 30 patients with any PGV would have been considered at high risk of PGV presence by these criteria. 20 patients (6.4%) fulfilled the Amsterdam II criteria for LS. In our cohort, three patients had PGVs associated with LS, but Amsterdam II criteria identified none of these patients. Among the 19 patients for whom the PREMM5 score could be obtained, 6 patients (31.6%; 19% of total cohort) had a predicted probability for a PGV in LS-associated genes of ≥ 2.5%. One of the three patients with an LS-associated PGV fulfilled the PREMM5 testing criteria. In summary, all known scores had low sensitivities in detecting patients with PGVs in our PCa population (Table S8).
In genetic counselling, patients with either relevant personal or family history for specific cancer syndromes are at risk of PGV presence. Patients also should be evaluated for PGVs if their family history is too limited for assessment (i.e. less than 5 first-degree family members with cancer history available). Therefore, we defined variables relevant for PCa patients with PGVs (Table S4). Logistic regression and ROC-curve analysis were performed (Table S5). The final variables comprised personal history of gastrointestinal or male breast cancer, first-degree relatives with a history of gastrointestinal, breast, endometrial, ovarian or PCa, and < 5 first-degree relatives with cancer histories available for assessment. If any of these three variables is fulfilled, the pretest probability of PGVs is high (score ≥ 1), and the patient should undergo genetic testing (Table 2). Among all patients, 207 had a PCa risk score ≥ 1, including all 30 patients with PGVs. 106 patients had a score < 1 with low probability of PGVs, none of these patients tested positive for PGVs.
Discussion
To our knowledge, this study reports results of the largest Austrian PCa population receiving germline sequencing in recent years. The prevalence of 9.6% for PGVs in advanced PCa is consistent with previous studies [1, 14, 19,20,21]. The most common PGVs were detected in BRCA2 (3.8% of all patients; 40% of patients with PGVs), CHEK2 (1.6%; 12.7%) and ATM (1.2%, 12.3%). A significantly higher prevalence of PGVs was found in patients with metastatic and/or castration-resistant PCa, in line with previous studies [2, 3, 5].
Regarding classic components of genetic assessment criteria such as personal or family cancer history, a direct comparison between patients with or without PGVs revealed neither a difference in the total number of diagnosed tumors, relatives with cancer, nor relevant tumors associated with HBOC or LS.
Noteworthy, there was also no difference considering only relatives with breast or ovarian cancer. This is in contrast to a recent study published by Sabol et al., reporting that a positive family history for breast or ovarian cancer was predictive for PGVs in their PCa cohort [22]. This discrepancy may be explained by a different emphasis on positive family history, which served as selection criterion for germline testing. In the study by Sabol et al., a large part of patients with localized PCa underwent germline testing due to positive family history. Approximately 13% of these patients with localized PCa harbored a PGV, in contrast to only 3.8% in our patient cohort.
Clinical criteria can be applied for other cancer entities within the HBOC or LS-tumor spectrum to better identify patients with a high probability for specific PGVs. In our PCa patient population, only a few patients with PGVs fulfilled the Amsterdam II criteria, the Manchester score criteria, or had a PREMM5 score ≥ 2.5 (0, 1, and 1 patient, respectively). These criteria were primarily designed to detect high probabilities for BRCA1/2 or mismatch repair gene alterations in patients with breast, ovarian or colorectal cancer. In our patient population, these criteria had very low sensitivities to identify PCa patients with PGVs and thus seem to have no clinical value in this setting.
Current evidence points to personalized screening protocols and adjusted therapeutic management of PCa patients, with both germline and tumor sequencing impacting decision-making [23, 24]. However, performing genetic testing according to the current EAU guidelines would identify all metastatic patients with PGVs (n = 27), but with the disadvantage of overtesting in 88% (n = 208) of patients. We designed a PCa-specific score categorizing patients either as low or high probability for PGVs based on personal and family cancer history. Whereas all patients with PGVs had a positive score and would thus have a high probability of PGV presence, one third of the patients without PGVs had scores of < 1 with a low probability of PGV presence. Consequently, these patients may not need germline DNA sequencing.
Our study has limitations. With 313 PCa patients, sample size is modest. This study was not population-based. Furthermore, the population consists of mainly white Caucasian men, which could lead to selection bias as disparities in PGVs had been described among racial minorities [25, 26]. Evaluation of different, previously introduced scores relied on patients’ memory of personal and family history. Furthermore, each previous score was designed to detect certain PGVs in specific genes. For example, the PREMM5 model does not consider PCa as a LS-associated tumor entity and was not designed for the cases with absent LS associated cancers. Thus, this calculator was only applicable for a minority of PCa patients in this study (n = 17). Although the PCa-specific score showed promising value for giving a pretest probability for the presence of PGVs, it will need validation in a larger prospective cohort study.
Conclusion
Current clinical criteria to identify patients at risk of PGVs are insufficient and warrant further research. A PCa-specific score based on personal and family history may stratify PCa patients into low- and high-risk groups for PGV presence and help simplifying diagnostic processes by excluding PCa patients with low pretest probabilities.
Data availability
Data are available upon request from Katharina Rebhan and Melanie R. Hassler, but access may be restricted due to Austrian law.
References
Pritchard CC, Mateo J, Walsh MF, De Sarkar N, Abida W, Beltran H et al (2016) Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med 375(5):443–453. https://doi.org/10.1056/NEJMoa1603144
Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M et al (2013) Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol 31(14):1748–1757. https://doi.org/10.1200/JCO.2012.43.1882
Castro E, Goh C, Leongamornlert D, Saunders E, Tymrakiewicz M, Dadaev T et al (2015) Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur Urol 68(2):186–193. https://doi.org/10.1016/j.eururo.2014.10.022
Mitra A, Fisher C, Foster CS, Jameson C, Barbachanno Y, Bartlett J et al (2008) Prostate cancer in male BRCA1 and BRCA2 mutation carriers has a more aggressive phenotype. Br J Cancer 98(2):502–507. https://doi.org/10.1038/sj.bjc.6604132
Wu Y, Yu H, Li S, Wiley K, Zheng SL, LaDuca H et al (2020) Rare germline pathogenic mutations of DNA repair genes are most strongly associated with grade group 5 prostate cancer. Eur Urol Oncol. https://doi.org/10.1016/j.euo.2019.12.003
Taylor RA, Fraser M, Livingstone J, Espiritu SM, Thorne H, Huang V et al (2017) Germline BRCA2 mutations drive prostate cancers with distinct evolutionary trajectories. Nat Commun 8:13671. https://doi.org/10.1038/ncomms13671
Gomella LG, Knudsen KE, Giri VN (2019) Introduction to the 2019 philadelphia prostate cancer consensus program: “implementation of genetic testing for inherited prostate cancer.” Can J Urol 26(5 Suppl 2):1–4
Mottet N, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 79(2):243–262
National Comprehensive Cancer Network: Prostate Cancer, Verion 4.2019. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed 19 Aug 2019
Evans DG, Eccles DM, Rahman N, Young K, Bulman M, Amir E et al (2004) A new scoring system for the chances of identifying a BRCA1/2 mutation outperforms existing models including BRCAPRO. J Med Genet 41(6):474–480. https://doi.org/10.1136/jmg.2003.017996
Vasen HF, Watson P, Mecklin JP, Lynch HT (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology 116(6):1453–1456. https://doi.org/10.1016/s0016-5085(99)70510-x
Kastrinos F, Uno H, Ukaegbu C, Alvero C, McFarland A, Yurgelun MB et al (2017) Development and validation of the PREMM(5) model for comprehensive risk assessment of lynch syndrome. J Clin Oncol 35(19):2165–2172. https://doi.org/10.1200/JCO.2016.69.6120
Carter BS, Bova GS, Beaty TH, Steinberg GD, Childs B, Isaacs WB et al (1993) Hereditary prostate cancer: epidemiologic and clinical features. J Urol 150(3):797–802. https://doi.org/10.1016/s0022-5347(17)35617-3
Nicolosi P, Ledet E, Yang S, Michalski S, Freschi B, O’Leary E et al (2019) Prevalence of germline variants in prostate cancer and implications for current genetic testing guidelines. JAMA Oncol 5(4):523–528. https://doi.org/10.1001/jamaoncol.2018.6760
Beltran H, Eng K, Mosquera JM, Sigaras A, Romanel A, Rennert H et al (2015) Whole-exome sequencing of metastatic cancer and biomarkers of treatment response. JAMA Oncol 1(4):466–474. https://doi.org/10.1001/jamaoncol.2015.1313
You YN, Wolff BG, Boardman LA, Riegert-Johnson DL, Qin R (2010) Peutz-Jeghers syndrome: a study of long-term surgical morbidity and causes of mortality. Fam Cancer 9(4):609–616. https://doi.org/10.1007/s10689-010-9358-1
Graziano F, Humar B, Guilford P (2003) The role of the E-cadherin gene (CDH1) in diffuse gastric cancer susceptibility: from the laboratory to clinical practice. Ann Oncol 14(12):1705–1713. https://doi.org/10.1093/annonc/mdg486
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American college of medical genetics and genomics and the Association for molecular pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Giri VN, Obeid E, Gross L, Bealin L, Hyatt C, Hegarty SE et al (2017) Inherited mutations in men undergoing multigene panel testing for prostate cancer: emerging implications for personalized prostate cancer genetic evaluation. JCO Precis Oncol. https://doi.org/10.1200/PO.16.00039
Annala M, Struss WJ, Warner EW, Beja K, Vandekerkhove G, Wong A et al (2017) Treatment outcomes and tumor loss of heterozygosity in germline DNA repair-deficient prostate cancer. Eur Urol 72(1):34–42. https://doi.org/10.1016/j.eururo.2017.02.023
Pritzlaff M, Tian Y, Reineke P, Stuenkel AJ, Allen K, Gutierrez S et al (2020) Diagnosing hereditary cancer predisposition in men with prostate cancer. Genet Med 22(9):1517–1523. https://doi.org/10.1038/s41436-020-0830-5
Sabol RA, Ledet EM, Jaeger E, Hatton W, Moses M, Lankford A et al (2021) Family history and pathogenic/likely pathogenic germline variants in prostate cancer patients. Prostate 81(7):427–432. https://doi.org/10.1002/pros.24120
Marino F, Totaro A, Gandi C, Bientinesi R, Moretto S, Gavi F et al (2022) Germline mutations in prostate cancer: a systematic review of the evidence for personalized medicine. Prostate Cancer Prostatic Dis. https://doi.org/10.1038/s41391-022-00609-3
Wang Z, Yan X, Tang P, Tang T, Wang Y, Peng S et al (2023) Genetic profiling of hormone-sensitive and castration-resistant prostate cancers and identification of genetic mutations prone to castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 26(1):180–187. https://doi.org/10.1038/s41391-022-00618-2
Pan E, Shaya J, Madlensky L, Randall JM, Javier-Desloges J, Millard FE et al (2022) Germline alterations among Hispanic men with prostate cancer. Prostate Cancer Prostatic Dis 25(3):561–567. https://doi.org/10.1038/s41391-022-00517-6
Weise N, Shaya J, Javier-Desloges J, Cheng HH, Madlensky L, McKay RR (2022) Disparities in germline testing among racial minorities with prostate cancer. Prostate Cancer Prostatic Dis 25(3):403–410. https://doi.org/10.1038/s41391-021-00469-3
Funding
Open access funding provided by Medical University of Vienna. MRH was supported by a grant of the Austrian society for Urology and Andrology (FA743A0601).
Author information
Authors and Affiliations
Contributions
KR and MRH: developed study conception and design. Material preparation, data collection and analysis were performed by KR, PDS, BP, PR, GK, BH, IR, FAL, MGB, and MS. The first draft of the manuscript was written by KR and MRH. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Informed consent was obtained from all individual participants included in the study.
Ethics approval
The study was approved by the local ethics committee (EK-Nr: 1043/2020, Ethics committee of the Medical University of Vienna).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rebhan, K., Stelzer, P.D., Pradere, B. et al. Performance of clinical risk scores and prediction models to identify pathogenic germline variants in patients with advanced prostate cancer. World J Urol 41, 2091–2097 (2023). https://doi.org/10.1007/s00345-023-04535-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04535-4