Abstract
Purpose
To compare the effectiveness, safety, and cost between ultrasound-guided shock wave lithotripsy (SWL) with an early second session protocol and ureteroscopy (URS) in patients with proximal ureteral stones using the propensity score matching (PSM) method based on a large prospective study.
Methods
This prospective study was conducted in a tertiary hospital from June 2020 to April 2022. Patients who underwent lithotripsy (SWL or URS) for proximal ureteral stones were enrolled. The stone-free rate (SFR), complications, and cost were recorded. PSM analysis was performed.
Results
A total of 1230 patients were included, of whom 81.1% (998) were treated with SWL and 18.9% (232) were treated with URS. After PSM, the SWL group had an equivalent SFR at one month (88.7 vs. 83.6%, P = 0.114) compared with the URS group. Complications were rare and comparable between the two groups, while the incidence of ureteral injuries was higher in the URS group compared with the SWL group (1.4 vs. 0%, P = 0.011). The hospital stay was significantly shorter (1 day vs. 2 days, P < 0.001), and the cost was considerably less (2000 vs. 25,053, P < 0.001) in the SWL group compared with the URS group.
Conclusion
This prospective PSM cohort demonstrated that ultrasound-guided SWL with an early second session protocol had equivalent effectiveness but better safety and lower cost compared with URS in the treatment of patients with proximal ureteral stones, whether the stones were radiopaque or radiolucent. These results will facilitate treatment decisions for proximal ureteral stones.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of urinary stones ranges from 1 to 20% [1]. Approximately 50% of patients have at least one lifetime recurrence [2, 3]. Urinary stones are commonly accompanied by several complications, including colic episodes, urinary tract infections, and even hydronephrosis, particularly in ureteral stones [4, 5]. Shock wave lithotripsy (SWL) and ureteroscopy (URS) are currently recommended as primary treatment modalities for ureteral stones [6]. The advantages of URS include direct visualization of fragmentation and a greater stone-free rate (SFR) but a higher complication rate [4]. SWL has the advantages of a low complication rate, no anesthesia requirement, and a high level of patient acceptance [7], but it may be associated with a lower SFR and higher retreatment rate [8]. Compared with distal ureteral stones, proximal ureteral stones are associated with lower success rates, which are ascribed to more difficult access, as well as proximal migration of the stone fragments during URS [9].
The COVID-19 pandemic had a significant impact on determining the intervention for ureteral stones. Procedures including general anesthesia and endotracheal intubation for URS pose a considerable risk of COVID-19 transmission [10, 11]. However, SWL is performed without general anesthesia and thereby may limit the risk [12]. The pandemic has also postponed large volumes of scheduled treatments to allow beds and staff to be available for patients seriously ill with COVID-19 [13].
There are only three prospective studies with small sample sizes that address this issue. Salem et al. [11] reported that the SFR was comparable between SWL and semirigid URS, while the mean costs were significantly higher in the SWL group; however, critical confounding factors, such as BMI, Hounsfield units of the stone, and hydronephrosis, were not adjusted in the study; Zhang et al. [14] found that the SFR following SWL was equivalent to semirigid ureteroscopy based on subgroup analysis, while SWL had a significant advantage with respect to the complication rate, charges, and period of hospitalization compared with the URS group. In another RCT, Ahmed et al. [15] reported that SWL is safe and effective compared to flexible URS; however, compared with the electrohydraulic lithotripter they used, the best results in stone fragmentation and fewer analgesia requirements occurred with the electromagnetic lithotripter [16]. The previous studies concerning this issue were limited and had a small number of participants. Furthermore, the conclusions were only suitable for radiopaque stones in the process of SWL.
The localization of stones can be guided by either ultrasound or fluoroscopy during SWL. Ultrasound localization not only provides real-time monitoring without X-ray exposure but is also suitable for both radiopaque and radiolucent stones. In addition, adding an early second SWL session significantly improved stone fragmentation, facilitated stone passage, and lower complication rate and cost [15, 17]. Therefore, based on a large prospective cohort using a propensity score matching (PSM) method, we compared the effectiveness, safety, and cost between electromagnetic SWL guided by ultrasound with the early second session protocol and URS in patients with proximal ureteral stones.
Methods
Study design
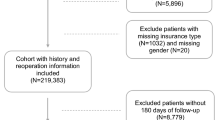
This prospective study was conducted on 1,230 patients of Shengjing Hospital from June 2010 to April 2022. Nine hundred and ninety-eight patients were treated with SWL, and 232 patients with URS, respectively (Figure S1). Ethical approval (No. 2020PS521K) was provided by the Ethics Committee of the Shengjing Hospital Affiliated China Medical University. Informed consent from all eligible subjects was obtained.
Inclusion and exclusion criteria
Inclusion criteria were: proximal ureteral stone with a size ≥ 6 mm, age ≥ 18 years, body mass index (BMI) < 30 kg/m2, ureter stone density < 1000 Hounsfield units (HU), and skin to stone distance (SSD) less than 11 cm, persistent obstruction, stone growth, infection.
Exclusion criteria were: pregnancy, coagulopathy, multiple or bilateral ureteral stones, anatomical obstruction distal to the stone or congenital genitourinary anomaly, transplanted kidney, solitary kidney, renal insufficiency.
Decision-making process: Patients were given the choice to undergo either URS or SWL after counseling them about the advantages and drawbacks of both procedures. After receiving the explanation, the patients selected the method they preferred.
The surgical technique of SWL
Extracorporeal shock wave lithotripsy was performed using a third-generation electromagnetic lithotripter (XYS.SUI-6B, Shenzhen, China). The focal depth was more than 110 mm; the focal area was ± 7 mm (radial) and ± 45–50 mm (axial). The procedure was performed in a supine or prone position without anesthesia or sedation requirements. The shock frequency used was 60–90 (shock waves/min). Stone localization and simultaneous real-time monitoring were performed by ultrasound (DC40, Shenzhen, China). All procedures in SWL group were outpatient procedures.
Follow-up KUB X-rays and urinary ultrasounds were taken one week after the first session, and patients underwent a second SWL session if there was stone fragmentation (≥ 4 mm) occurred. The preplanned SWL modality included two sessions of SWL within one week, as a package of intervention.
The surgical technique of URS
All procedures were performed under general or spinal anesthesia. An 8Fr/9.5Fr rigid ureteroscopy (Richard Wolf, Knittlingen, Germany) was employed. The fragmentation source was pneumatic and ultrasonic lithoclast systems (Electro Medical Systems, Nyon, Switzerland). Fragments were extracted by forceps or nitinol baskets (Ngage, Cook Incorporated, USA). Special anti-migration tools (stone cone, Boston Scientific, USA) were applied to prevent stone migration into the kidney. A 6 Fr JJ stent was placed after URS.
Propensity score matching
We used the PSM method to adjust baseline confounding variables between the URS and SWL group in an effort to derive more accurate conclusions. Multivariate logistic regression analysis was used to determine propensity scores for each patient based on age, gender, BMI, smoking status, comorbidities, previous history of ureteral stone, and stone data (all baseline variables in Table 1). The URS and SWL groups were matched 1:4 using a caliper width 0.2 of the standard deviation of the logit of the propensity score through the nearest neighbor matching (Figure S2).
Statistical analysis
Data were analyzed by SPSS 22.0 software. Continuous variables were presented as the median (interquartile range). Categorical variables were reported as the number (percentage). Before PSM, independent samples Student’s t test was used to compare the mean of two continuous normally distributed variables and the Mann–Whitney U test was used to compare the mean of two continuous non-normally distributed variables, The χ2 test or Fisher’s exact test was used for categorical variables. After PSM, the categorical variables were compared by binary conditional logistic regression. Paired samples Student’s t test was used to compare the mean of two continuous normally distributed variables, and the Wilcoxon test was used to compare the mean of two continuous non-normally distributed variables in univariate analysis. A p value of less than 0.05 was considered statistically significant.
Results
A total of 1230 patients were included in the final analysis and divided into two groups. We achieved a balance of baseline variables between the two groups after PSM; 998 patients treated with SWL and 232 patients treated with URS were balanced into 774 patients treated with SWL and 220 patients treated with URS. In the matched group, the median age of the patients in the SWL and URS groups was 55 and 54 years, respectively (P = 0.265). Most patients were males (64.7 vs. 61.4%). The BMI was 25.22 and 25.39 kg/m2 (P = 0.594); see details in Table 1.
The procedural duration was comparable between SWL and URS (39 vs. 41 min, P = 0.145). The rate of stone migration into the kidney in the URS group was 16.40%. The SFR at one month (87.7% vs. 83.6%, P = 0.114) and three months (96.8% vs. 98.2%, P = 0.272) was equivalent between the two groups. Of the postoperative data, there were a little lower secondary treatment rates in the SWL group than that in the URS group (10.10% vs. 12.70%, P = 0.261). The incidence of minor complications (Clavien 1–2), major complications (Clavien 3–4), SIRS, and sepsis was comparable between the two groups. The mortality (Clavien 5) of both groups was 0%. The rate of steinstrasse in the SWL group was 1.7%, which was a little higher than that in the URS group (0.00%, P = 0.084). One percent of patients in the SWL group developed renal colic (analgesic requirement), and no patients suffered from renal hematoma in both groups. No patient in the SWL group had a ureteral injury (stenosis or perforation), but the ureteral injury rate in the URS group was higher (1.4%, P = 0.011). The length of hospital stay (one day vs. two days, P < 0.001) and cost (2,000 RMB vs. 25,053 RMB, P < 0.001) in the SWL group were significantly lower than that in the URS group (Table 2).
Discussion
SWL and URS are the most commonly used treatment modalities for proximal ureteral stones; however, previous studies with a prospective study design comparing these two techniques were limited with a small sample size, and the conclusions were only suitable for radiopaque stones. The present study aimed to compare the effectiveness, safety, and cost between ultrasound-guided SWL with the early second session protocol and URS in patients with proximal ureteral stones. Furthermore, this prospective PSM cohort provided a fair comparison. SWL had equivalent effectiveness and increased safety and less cost compared with URS, whether the stones were radiopaque or radiolucent.
In this study, we found that the SFR was equivalent between the SWL and URS groups at one (88.7% vs. 83.6%, P = 0.114) and three months (96.8% vs. 98.2%, P = 0.272). In agreement with this finding, in a RCT that enrolled 108 patients with radiopaque proximal ureteral stones (< 1.5 cm in size and ≤ 1,000 Hounsfield units), Ahmed et al. [12] found that there were no statistical differences between the early second session SWL (within 48–72 h of the first session) and flexible-URS SFR (92.6% vs. 96.2%, P = 0.418) and an auxiliary procedure (5.6% vs. 3.7%, P = 0.640). Therefore, they concluded that SWL is safe and effective compared to flexible URS. In another RCT that enrolled 200 patients with radiopaque proximal ureteral stones ≤ 20 mm in size, Salem et al. [11] demonstrated that the SFR was comparable between SWL and semirigid URS for stone size ≥ 1 cm (60% vs. 88%, P > 0.05) or < 1 cm in size (80% vs. 100%, P > 0.05). They suggested SWL should be the first-line therapy for proximal ureteral stones < 1 cm in size because SWL is less invasive, while URS is an acceptable treatment modality for proximal ureteral stones, especially in stones ≥ 1 cm in size.
In a retrospective study including 400 patients with proximal ureteral stones < 20 mm in size, Iqbal et al. [18] found that the SFR for SWL was inferior to rigid URS with pneumatic lithotripsy after the first (62.5% vs. 84%, P = 0.001) and second session (86% vs. 94%, P = 0.01). The main reasons that accounted for these discrepancies were that the patients were treated with an early second session SWL protocol under real-time ultrasound localization. This protocol significantly improved the effectiveness of fragmentation and subsequently enhanced the SFR [17]. In addition, the retrospective design and small sample size also limited validation of the results.
In the present study, the secondary treatment morbidity was comparable between the SWL and URS groups (10.10% vs. 12.70%, P = 0.261). In a meta-analysis that included 11 studies focusing on secondary procedures, 880 patients with proximal ureteral stones were treated primarily with SWL and 787 were treated primarily with URS. The secondary treatment rate varied greatly between studies, ranging from 2.6 to 45% in the primary SWL group and 4%-50% in the primary URS group [7]. The relatively low rate in the present study may be attributed to the early second session SWL protocol, which had advantages in achieving SFR and reducing complications.
The assessment of complications is essential for further comparisons of both interventions. In this study, morbidity was low and comparable between the SWL and URS groups, except for ureteric injuries. There was no ureteric injury observed in the SWL group, whereas 3 of 220 patients treated with URS had ureteric injuries (0.0 vs. 1.4%, P = 0.011), which is reported to be the most severe complication during the URS process. In agreement with this finding, Castro et al. [19] reported a 1.1% ureteral perforation rate in the treatment of proximal ureteral stones based on a prospective study enrolled in > 9600 patients from multicenters. The mechanism may be that the proximal ureter had lower levels of tensile strength, which were more likely to cause ureteral perforations [20]. In addition, the invasiveness of ureteroscopy may lead to mucosal edema or injury. The patients with ureteric injuries were treated successfully with the placement of a stent. Although the incidence of steinstrasse and renal colic was a little higher in the SWL group than in the URS group, the incidence was low and there was no statistical difference between the two groups. In addition, these complications were immediately and successfully treated by the early second session SWL protocol.
This study demonstrated that SWL was less cost than URS, with a significantly shorter length of hospital stay and a lower mean cost. Similar results have been described by Zhang [14], who reported that the SWL requires lower costs (USD 445 vs. 1327, P < 0.001) and a shorter period of hospitalization (5.4 vs. 6.6 days, P < 0.001) compared with the URL in an RCT that recruited 155 patients with proximal ureteral stones. The addition of special instruments developed for URS, such as tipless nitinol baskets, also increases the cost. In addition, the requirement for expensive repairs, especially with respect to the learning curve of the URS, should also be kept in mind in the management of these patients. SWL has the benefit of avoiding double “J” stent fixation and removal, general anesthesia, and the associated complications and cost. Therefore, the medical costs were also dramatically reduced. In addition, all patients in the SWL group were treated as day surgery patients in this study and could resume normal activities as soon as possible.
There were several limitations in the present study. First, this was a non-randomized study from a single situation with inherent selection bias; however, the known confounders were controlled by PSM in this study. Second, no available data were found about stone composition; however, we adjusted the computed tomography (CT) value to obtain reliable results. Third, the stone-free status was evaluated by a combination KUB X-ray and ultrasound instead of CT, which might result in an overestimation of the SFR. Fourth, we were not able to report long-term complications, such as the incidence of ureteral stenosis. Nevertheless, this is the first large-scale PSM cohort study to explore the effectiveness, safety, and cost between URS and short-interval SWL for proximal ureteral stones. In addition, SWL is preferred for treating proximal ureteral stones during the COVID-19 pandemic because SWL is performed by an outpatient procedure with fewer medical resources consumed. Further multicenter RCTs are needed to accurately compare these two treatment modalities.
Conclusion
This prospective PSM cohort demonstrated that ultrasound-guided SWL with an early second session protocol had equivalent effectiveness but better safety and lower cost compared with URS in the treatment of patients with proximal ureteral stones, whether the stones were radiopaque or radiolucent. These results will facilitate treatment decisions for proximal ureteral stones.
Availability of data and materials
Not applicable.
References
Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y (2017) Epidemiology of stone disease across the world. World J Urol 35(9):1301–1320
Hesse A, Brandle E, Wilbert D, Kohrmann KU, Alken P (2003) Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol 44(6):709–713
Strohmaier WL (2000) Course of calcium stone disease without treatment. What can we expect? Eur Urol 37(3):339–344
McClinton S, Cameron S, Starr K, Thomas R, MacLennan G, McDonald A et al (2018) TISU: Extracorporeal shockwave lithotripsy, as first treatment option, compared with direct progression to ureteroscopic treatment, for ureteric stones: study protocol for a randomised controlled trial. Trials 19(1):286
Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP et al (2016) Surgical Management of Stones: American Urological Association/Endourological Society Guideline. PART I J Urol 196(4):1153–1160
Turk C, Petrik A, Sarica K, Seitz C, Skolarikos A, Straub M et al (2016) EAU guidelines on interventional treatment for urolithiasis. Eur Urol 69(3):475–482
Drake T, Grivas N, Dabestani S, Knoll T, Lam T, Maclennan S et al (2017) What are the benefits and harms of ureteroscopy compared with shock-wave lithotripsy in the treatment of upper ureteral stones? A Systematic Review Eur Urol 72(5):772–786
Mi Y, Ren K, Pan H, Zhu L, Wu S, You X et al (2016) Flexible ureterorenoscopy (F-URS) with holmium laser versus extracorporeal shock wave lithotripsy (ESWL) for treatment of renal stone <2 cm: a meta-analysis. Urolithiasis 44(4):353–365
Shaikh AH, Khalid SE, Zaidi SZ (2008) Ureteroscopy under spinal versus general anaesthesia: morbidity and stone clearance. J Coll Physicians Surg Pak 18(3):168–171
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395(10223):497–506
Salem HK (2009) A prospective randomized study comparing shock wave lithotripsy and semirigid ureteroscopy for the management of proximal ureteral calculi. Urology 74(6):1216–1221
Lee SM, Collin N, Wiseman H, Philip J (2019) Optimisation of shock wave lithotripsy: a systematic review of technical aspects to improve outcomes. Transl Androl Urol 8(Suppl 4):S389–S397
Shivakumar N, Nantha Kumar D, Joshi H (2022) The impact of early COVID-19 pandemic on the presentation and management of urinary calculi across the globe: a systematic review. J Endourol. https://doi.org/10.1089/end.2022.0167
Zhang J, Shi Q, Wang GZ, Wang F, Jiang N (2011) Cost-effectiveness analysis of ureteroscopic laser lithotripsy and shock wave lithotripsy in the management of ureteral calculi in eastern China. Urol Int 86(4):470–475
Abdelbary AM, Al-Dessoukey AA, Moussa AS, Elmarakbi AA, Ragheb AM, Sayed O et al (2021) Value of early second session shock wave lithotripsy in treatment of upper ureteric stones compared to laser ureteroscopy. World J Urol 39(8):3089–3093
Bianchi G, Marega D, Knez R, Bucci S, Trombetta C (2018) Comparison of an electromagnetic and an electrohydraulic lithotripter: efficacy, pain and complications. Arch Ital Urol Androl 90(3):169–171
Turan T, Efioglu O, Danacioglu YO, Sendogan F, Culpan M, Gunaydin B et al (2018) Can intervals in extracorporeal shock wave lithotripsy sessions affect success in the treatment of upper ureteral stones? Wideochir Inne Tech Maloinwazyjne 13(4):507–511
Iqbal N, Malik Y, Nadeem U, Khalid M, Pirzada A, Majeed M et al (2018) Comparison of ureteroscopic pneumatic lithotripsy and extracorporeal shock wave lithotripsy for the management of proximal ureteral stones: a single center experience. Turk J Urol 44(3):221–227
Perez Castro E, Osther PJ, Jinga V, Razvi H, Stravodimos KG, Parikh K et al (2014) Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol 66(1):102–109
Shilo Y, Pichamuthu JE, Averch TD, Vorp DA (2014) Evaluation of the tensile strength of the human ureter–preliminary results. J Endourol 28(12):1470–1473
Acknowledgements
We give special thanks to all the colleagues at the Department of Urology of Shengjing Hospital for their help and support. We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript. The authors would like to thank all of the study participants.
Funding
This study was financially supported by The 345 Talent Project of Shengjing Hospital, Natural Science Foundation of Liaoning Science and Technology Department (grant number 2020-BS-093), and Natural Science Foundation of Liaoning Education Department (grant number QN2019013). These sponsors had no role in the study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SB and ZL: had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SB and ZL: contributed to protocol/project development. PW, YZ, JL, GL, ZL, and SB: were involved in data collection or management. PW, YZ, JL, GL, ZL, and SB: contributed to data analysis. PW and SB: were involved in manuscript writing/editing.
Corresponding authors
Ethics declarations
Conflict of interest
There is no conflict of interest.
Ethical approval
Ethical approval (No. 2020PS521K) was provided by Ethics Committee of the Shengjing Hospital Affiliated China Medical University. Informed consent from all eligible subjects was obtained. The clinical research registry UIN is ChiCTR2000033790. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Consent for publication
Informed consent from all eligible patients was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, P., Zhan, Y., Li, J. et al. Comparison of shock wave lithotripsy and ureteroscopy in patients with proximal ureteral stones under the COVID-19 pandemic. World J Urol 41, 797–803 (2023). https://doi.org/10.1007/s00345-023-04307-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04307-0