Abstract
Purpose
To investigate whether peritoneal cavity could function as bioreactor to produce autologous tubular grafts for urethral reconstruction in male rabbits.
Methods
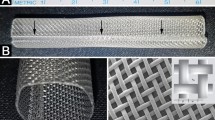
8Fr silastic tubes were implanted into peritoneal cavities of nine male rabbits. By 2 weeks, tubes were harvested and the tubular tissue covering the tubes was everted. A pendulous urethral segment of 1.5 cm long was totally excised and urethroplasty was performed with the everted tubular tissue in an end-to-end fashion. Another nine male rabbits underwent the same urethral resection and re-anastomosis as controls. Urethrography was performed at 1, 2 and 6 months postoperatively. Meanwhile, the neo-urethra were harvested and analyzed grossly and histologically.
Results
Histological analysis of the tubular tissue demonstrated transversely arranged myofibroblasts embedded in homogeneous collagen bundles and an outer layer of mesothelium. The tissue was easily everted and successfully transplanted as a urethral graft. Serial urethrography indicated no stricture or diverticula formation. While all animals of the control group developed stricture. Histological analysis of the neo-urethra demonstrated normal urethral architecture by 1 month, composed of multi-layers of urothelium surrounded by smooth muscle bundles, which became increasingly organized with time. By 6 months, the neo-urethra could be hardly distinguished from native urethra both grossly and histologically.
Conclusions
These results show that the autologous tissue grown within the recipients’ peritoneal cavity can be used successfully for tubularized urethral reconstruction in male rabbits.





Similar content being viewed by others
References
Barbagli G, Guazzoni G, Palminteri E et al (2006) Anastomotic fibrous ring as cause of stricture recurrence after bulbar onlay graft urethroplasty. J Urol 176:614–619. doi:10.1016/j.juro.2006.03.097
Barbagli G, Guazzoni G, Lazzeri M (2008) One-stage bulbar urethroplasty: retrospective analysis of the results in 375 patients. Eur Urol 53:828–833. doi:10.1016/j.eururo.2008.01.041
Ozgok Y, Ozgur Tan M, Kilciler M et al (2000) Use of bladder mucosal graft for urethral reconstruction. Int J Urol 7:355–360. doi:10.1046/j.1442-2042.2000.00210.x
Levine LA, Strom KH, Lux MM (2007) Buccal mucosa graft urethroplasty for anterior urethral stricture repair: evaluation of the impact of stricture location and lichen sclerosus on surgical outcome. J Urol 178:2011–2015. doi:10.1016/j.juro.2007.07.034
Campbell JH, Efendy JL, Campbell GR (1999) Novel vascular graft grown within recipient’s own peritoneal cavity. Circ Res 85:1173–1178
Chue WL, Campbell GR, Caplice N et al (2004) Dog peritoneal and pleural cavities as bioreactors to grow autologous vascular grafts. J Vasc Surg 39:859–867. doi:10.1016/j.jvs.2003.03.003
Campbell GR, Turnbull G, Xiang L et al (2008) The peritoneal cavity as a bioreactor for tissue engineering visceral organs: bladder, uterus and vas deferens. J Tissue Eng Regen Med 2:50–60. doi:10.1002/term.66
De Filippo RE, Yoo JJ, Atala A (2002) Urethral replacement using cell seeded tubularized collagen matrices. J Urol 168:1789–1793. doi:10.1097/01.ju.0000027662.69103.72
Fu Q, Deng CL, Liu W et al (2007) Urethral replacement using epidermal cell-seeded tubular acellular bladder collagen matrix. BJU Int 99:1162–1165. doi:10.1111/j.1464-410X.2006.06691.x
Shokeir A, Osman Y, Gabr M et al (2004) Acellular matrix tube for canine urethral replacement: is it fact or fiction? J Urol 171:453–456. doi:10.1097/01.ju.0000089776.52568.9e
Dorin RP, Pohl HG, De Filippo RE et al (2008) Tubularized urethral replacement with unseeded matrices: what is the maximum distance for normal tissue regeneration? World J Urol 26:323–326. doi:10.1007/s00345-008-0316-6
Kajbafzadeh AM, Arshadi H, Payabvash S et al (2007) Proximal hypospadias with severe chordee: single stage repair using corporeal tunica vaginalis free graft. J Urol 178:1036–1042. doi:10.1016/j.juro.2007.05.062
Zargooshi J (2004) Tube-onlay-tube tunica vaginalis flap for proximal primary and reoperative adult hypospadias. J Urol 171:224–228. doi:10.1097/01.ju.0000101881.80100.ab
Shaul DB, Xie HW, Diaz JF et al (1996) Use of tubularized peritoneal free grafts as urethral substitutes in the rabbit. J Pediatr Surg 31:225–228. doi:10.1016/S0022-3468(96)90002-0
Nanni L, Vallasciani S, Fadda G et al (2001) Free peritoneal grafts for patch urethroplasty in male rabbits. J Urol 165:578–580. doi:10.1097/00005392-200102000-00074
Reddy PP, Barrieras DJ, Wilson G (2000) Regeneration of functional bladder substitutes using large segment acellular matrix allografts in a porcine model. J Urol 164:936–941. doi:10.1016/S0022-5347(05)67221-7
Sievert KD, Tanagho EA (2000) Organ-specific acellular matrix for reconstruction of the urinary tract. World J Urol 18:19–25. doi:10.1007/s003450050004
Herrick SE, Mutsaers SE (2004) Mesothelial progenitor cells and their potential in tissue engineering. Int J Biochem Cell Biol 36:621–642. doi:10.1016/j.biocel.2003.11.002
Efendy JL, Campbell GR, Campbell JH (2000) The effect of environmental cues on the differentiation of myofibroblasts in peritoneal granulation tissue. J Pathol 192:257–262. doi:10.1002/1096-9896(2000)9999:9999<::AID-PATH681>3.0.CO;2-Y
Acknowledgments
This study is supported by grants from Shanghai Municipal Health Bureau (040303-10) and Shanghai Shen Kang Platform Grant (SHDC12007206). We also thank Dr. Yilin Cao, Dr. Wei Liu (Department of Plastic and Reconstructive Surgery, Shanghai 9th People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China) and National Tissue Engineering Center of China (Shanghai, People’s Republic of China) for technical assistance.
Conflict of interest statement
The authors declare that there is no conflict of interest involved in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
G.-L. Gu and Y.-J. Zhu contributed equally to this study.
Rights and permissions
About this article
Cite this article
Gu, GL., Zhu, YJ., Xia, SJ. et al. Peritoneal cavity as bioreactor to grow autologous tubular urethral grafts in a rabbit model. World J Urol 28, 227–232 (2010). https://doi.org/10.1007/s00345-009-0447-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-009-0447-4