Abstract
Objectives
The study of postoperative liver decompensation after microwave ablation (MWA) for hepatocellular carcinoma (HCC) in patients with clinically significant portal hypertension (CSPH) is still lacking. The purpose of the present study was to compare the postoperative liver decompensation after MWA and laparoscopic resection (LR) for HCC in patients with CSPH.
Methods
The present retrospective study enrolled 222 HCC patients with CSPH who underwent MWA (n = 67) or LR (n = 155). Postoperative liver decompensation, complications, postoperative hospital stays, and overall survival were analyzed. Factors associated with postoperative liver decompensation were identified.
Results
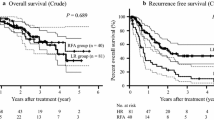
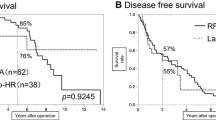
After propensity score matching, the postoperative liver decompensation rate was significantly lower in the MWA group than that in the LR group (15.5% versus 32.8%, p = 0.030). The multivariable regression analysis identified that type of treatment (MWA vs. LR, odds ratio [OR] 0.44; 95% confidence interval [CI], 0.21–0.91; p = 0.026) and Child–Pugh B (OR, 2.86; 95% CI, 1.24–6.61; p = 0.014) were independent predictors for postoperative liver decompensation. The rate of complications for patients in the MWA group was significantly lower than that in the LR group (p < 0.001). And MWA showed shorter postoperative hospital stays than LR (3 days vs. 6 days, p < 0.001). Overall survival rate between the two groups was not significantly different (p = 0.163).
Conclusion
Compared with laparoscopic resection, microwave ablation has a lower rate of postoperative liver decompensation and might be a better option for HCC patients with CSPH.
Clinical relevance statement
Microwave ablation exhibited a lower incidence of postoperative liver decompensation in comparison to laparoscopic resection, thereby conferring greater advantages to hepatocellular carcinoma patients with clinically significant portal hypertension.
Key Points
•Postoperative liver decompensation rate after microwave ablation was lower than that of laparoscopic resection for hepatocellular carcinoma in patients with clinically significant portal hypertension.
•Microwave ablation showed shorter postoperative hospital stays than laparoscopic resection.
•Microwave ablation had fewer complications than laparoscopic resection.




Similar content being viewed by others
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- CSPH:
-
Clinically significant portal hypertension
- HCC:
-
Hepatocellular carcinoma
- IQR:
-
Interquartile ranges
- LR:
-
Laparoscopic resection
- LTP:
-
Local tumor progression
- MELD:
-
Model for end-stage liver disease
- MWA:
-
Microwave ablation
- OS:
-
Overall survival
- PHLF:
-
Post-hepatectomy liver failure
- PLT:
-
Platelet counts
- PSM:
-
Propensity score matching
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Craig AJ, von Felden J, Garcia-Lezana T, Sarcognato S, Villanueva A (2020) Tumour evolution in hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol 17:139–152
European Association for the Study of the Liver (2018) EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 69:182–236
Citterio D, Facciorusso A, Sposito C, Rota R, Bhoori S, Mazzaferro V (2016) Hierarchic interaction of factors associated with liver decompensation after resection for hepatocellular carcinoma. JAMA Surg 151:846–853
Berzigotti A, Reig M, Abraldes JG, Bosch J, Bruix J (2015) Portal hypertension and the outcome of surgery for hepatocellular carcinoma in compensated cirrhosis: a systematic review and meta-analysis. Hepatology 61:526–536
Berardi G, Morise Z, Sposito C et al (2020) Development of a nomogram to predict outcome after liver resection for hepatocellular carcinoma in Child-Pugh B cirrhosis. J Hepatol 72:75–84
Gustot T, Stadlbauer V, Laleman W, Alessandria C, Thursz M (2021) Transition to decompensation and acute-on-chronic liver failure: role of predisposing factors and precipitating events. J Hepatol 75(Suppl 1):S36-s48
Kokudo T, Hasegawa K, Shirata C et al (2019) Assessment of preoperative liver function for surgical decision making in patients with hepatocellular carcinoma. Liver Cancer 8:447–456
Zheng J, Feng X, Liang Y et al (2021) Safety and feasibility of laparoscopic liver resection for hepatocellular carcinoma with clinically significant portal hypertension: a propensity score-matched study. Surg Endosc 35:3267–3278
Heimbach JK, Kulik LM, Finn RS et al (2018) AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67:358–380
Zheng H, Xu C, Wang X et al (2020) Microwave ablation shows similar survival outcomes compared with surgical resection for hepatocellular carcinoma between 3 and 5 cm. Int J Hyperthermia 37:1345–1353
Wang Z, Liu M, Zhang DZ et al (2022) Microwave ablation versus laparoscopic resection as first-line therapy for solitary 3-5-cm HCC. Hepatology 76:66–77
Liu K, Zheng H, Sui X et al (2022) Microwave ablation versus surgical resection for subcapsular hepatocellular carcinoma: a propensity score-matched study of long-term therapeutic outcomes. Eur Radiol. https://doi.org/10.1007/s00330-022-09135-1
Takayama T, Hasegawa K, Izumi N et al (2022) Surgery versus radiofrequency ablation for small hepatocellular carcinoma: a randomized controlled trial (SURF trial). Liver Cancer 11:209–218
Marrero JA, Kulik LM, Sirlin CB et al (2018) Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 68:723–750
Tajiri T, Yoshida H, Obara K et al (2010) General rules for recording endoscopic findings of esophagogastric varices (2nd edition). Dig Endosc 22:1–9
Kim SH, Kim YJ, Lee JM et al (2007) Esophageal varices in patients with cirrhosis: multidetector CT esophagography–comparison with endoscopy. Radiology 242:759–768
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Faitot F, Allard MA, Pittau G et al (2015) Impact of clinically evident portal hypertension on the course of hepatocellular carcinoma in patients listed for liver transplantation. Hepatology 62:179–187
Mathew G, Agha R (2021) STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 96:106165
An C, Cheng Z, Yu X et al (2020) Ultrasound-guided percutaneous microwave ablation of hepatocellular carcinoma in challenging locations: oncologic outcomes and advanced assistive technology. Int J Hyperthermia 37:89–100
Urrunaga NH, Singal AG, Cuthbert JA, Rockey DC (2013) Hemorrhagic ascites. Clinical presentation and outcomes in patients with cirrhosis. J Hepatol 58:1113–1118
Liu CH, Arellano RS, Uppot RN, Samir AE, Gervais DA, Mueller PR (2010) Radiofrequency ablation of hepatic tumours: effect of post-ablation margin on local tumour progression. Eur Radiol 20:877–885
D’Amico G, Bernardi M, Angeli P (2022) Towards a new definition of decompensated cirrhosis. J Hepatol 76:202–207
Rahbari NN, Garden OJ, Padbury R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Ahmed M, Solbiati L, Brace CL et al (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. Radiology 273:241–260
Vitale A, Peck-Radosavljevic M, Giannini EG et al (2017) Personalized treatment of patients with very early hepatocellular carcinoma. J Hepatol 66:412–423
Azoulay D, Ramos E, Casellas-Robert M et al (2021) Liver resection for hepatocellular carcinoma in patients with clinically significant portal hypertension. JHEP Rep 3:100190
Feng H, Yang C, Xu F et al (2022) Therapeutic efficacy of microwave coagulation versus liver resection for hepatocellular carcinoma within the Milan criteria: a propensity score matching analysis. Eur J Surg Oncol 48:418–424
Qiu J, Zheng Y, Shen J et al (2015) Resection versus ablation in hepatitis B virus-related hepatocellular carcinoma patients with portal hypertension: a propensity score matching study. Surgery 158:1235–1243
Harada N, Maeda T, Yoshizumi T et al (2016) Laparoscopic liver resection is a feasible treatment for patients with hepatocellular carcinoma and portal hypertension. Anticancer Res 36:3489–3497
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 82160124; 82203658; 82100641) and the Study program of Corps science and technology (No. 2022AB024), Project of Science and Technology of Xinjiang Autonomous Region (2022E02044).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xinya Zhao.
Conflict of interest
The authors declare no competing interests.
Statistics and biometry
Yes, we enlisted a statistical expert, Xiaoxiao Men, to carefully review the statistical methods utilized throughout this study.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
The study was approved by the ethical committee of Shandong Provincial Hospital.
Study subjects or cohorts overlap
None.
Methodology
• retrospective
• prognostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, H., Zhao, F., Men, X. et al. Microwave ablation versus laparoscopic resection for hepatocellular carcinoma in patients with clinically significant portal hypertension: a propensity score–matched study of postoperative liver decompensation. Eur Radiol (2023). https://doi.org/10.1007/s00330-023-10268-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-023-10268-0