Abstract
Objectives
To develop a mediastinal shift angle (MSA) measurement method applicable to right-sided congenital diaphragmatic hernia (RCDH) in fetal MRI and to validate the predictive value of MSA in RCDH.
Methods
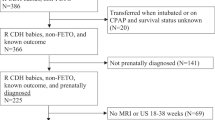
Twenty-seven fetuses with isolated RCDH and 53 controls were included in our study. MSA was measured on MRI axial image at the level of four-chamber view of the fetal heart. The angle between the sagittal midline landmark line and the left boundary landmark line touching tangentially the lateral wall of the left ventricle was used to quantify MSA for RCDH. Appropriate statistical analyses were performed to determine whether MSA can be regarded as a valid predictive tool for postnatal outcomes. Furthermore, predictive performance of MSA was compared with that of lung area to head circumference ratio (LHR), observed/expected LHR (O/E LHR), total fetal lung volume (TFLV), and observed/expected TFLV (O/E TFLV).
Results
MSA was significantly higher in the RCDH group than in the control group. MSA, LHR, O/E LHR, TFLV, and O/E TFLV were all correlated with postnatal survival, pulmonary hypertension (PH), and extracorporeal membrane oxygenation (ECMO) therapy (p < 0.05). Value of the AUC demonstrated good predictive performance of MSA for postnatal survival (0.901, 95%CI: (0.781–1.000)), PH (0.828, 95%CI: (0.661–0.994)), and ECMO therapy (0.813, 95%CI: (0.645–0.980)), which was similar to O/E TFLV but slightly better than TFLV, O/E LHR, and LHR.
Conclusions
We developed a measurement method of MSA for RCDH for the first time and demonstrated that MSA could be used to predict postnatal survival, PH, and ECMO therapy in RCDH.
Clinical relevance statement
Newly developed MRI assessment method of fetal MSA in RCDH offers a simple and effective risk stratification tool for patients with RCDH.
Key Points
• We developed a measurement method of mediastinal shift angle for right-sided congenital diaphragmatic hernia for the first time and demonstrated its feasibility and reproducibility.
• Mediastinal shift angle can predict more prognostic information other than survival in right-sided congenital diaphragmatic hernia with good performance.
• Mediastinal shift angle can be used as a simple and effective risk stratification tool in right-sided congenital diaphragmatic hernia to improve planning of postnatal management.




Similar content being viewed by others
Abbreviations
- CDH:
-
Congenital diaphragmatic hernia
- CDHSG:
-
Congenital Diaphragmatic Hernia Study Group
- ECLS:
-
Extracorporeal life support
- ECMO:
-
Extracorporeal membrane oxygenation
- FETO:
-
Fetal endoluminal tracheal occlusion
- LCDH:
-
Left-sided diaphragmatic hernia
- LHR:
-
Lung area to head circumference ratio
- MSA:
-
Mediastinal shift angle
- O/E LHR:
-
Observed/expected lung area to head circumference ratio
- O/E TFLV:
-
Observed/expected total fetal lung volume
- PH:
-
Pulmonary hypertension
- PPLV:
-
Percent predicted lung volume
- RCDH:
-
Right-sided diaphragmatic hernia
- TFLV:
-
Total fetal lung volume
References
Politis MD, Bermejo-Sánchez E, Canfield MA et al (2021) Prevalence and mortality in children with congenital diaphragmatic hernia: a multicountry study. Ann Epidemiol 56:61-69.e3
Montalva L, Antounians L, Zani A (2019) Pulmonary hypertension secondary to congenital diaphragmatic hernia: factors and pathways involved in pulmonary vascular remodeling. Pediatr Res 85:754–768
Badillo A, Gingalewski C (2014) Congenital diaphragmatic hernia: treatment and outcomes. Semin Perinatol 38:92–96
Clark RH, Hardin WD Jr, Hirschl RB et al (1998) Current surgical management of congenital diaphragmatic hernia: a report from the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg 33:1004–1009
Partridge EA, Peranteau WH, Herkert L et al (2016) Right- versus left-sided congenital diaphragmatic hernia: a comparative outcomes analysis. J Pediatr Surg 51:900–902
Burgos CM, Frenckner B, Luco M et al (2018) Right versus left congenital diaphragmatic hernia - what’s the difference. J Pediatr Surg 53:113–117
Duess JW, Zani-Ruttenstock EM, Garriboli M, Puri P, Pierro A, Hoellwarth ME (2015) Outcome of right-sided diaphragmatic hernia repair: a multicentre study. Pediatr Surg Int 31:465–471
Bryner BS, Kim AC, Khouri JS et al (2009) Right-sided congenital diaphragmatic hernia: high utilization of extracorporeal membrane oxygenation and high survival. J Pediatr Surg 44:883–887
DeKoninck P, Gomez O, Sandaite I et al (2015) Right-sided congenital diaphragmatic hernia in a decade of fetal surgery. BJOG 122:940–946
Graham G, Devine PC (2005) Antenatal diagnosis of congenital diaphragmatic hernia. Semin Perinatol 29:69–76
Sepulveda W, Wong AE, Casasbuenas A, Solari A, Alcalde JL (2008) Congenital diaphragmatic hernia in a first-trimester ultrasound aneuploidy screening program. Prenat Diagn 28:531–534
Metkus AP, Filly RA, Stringer MD, Harrison MR, Adzick NS (1996) Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg 31:148–152 (discussion 151-152)
Basta AM, Lusk LA, Keller RL, Filly RA (2016) Fetal stomach position predicts neonatal outcomes in isolated left-sided congenital diaphragmatic hernia. Fetal Diagn Ther 39:248–255
Gentili A, Pasini L, Iannella E et al (2015) Predictive outcome indexes in neonatal congenital diaphragmatic hernia. J Matern Fetal Neonatal Med 28:1602–1607
Jani JC, Peralta CF, Nicolaides KH (2012) Lung-to-head ratio: a need to unify the technique. Ultrasound Obstet Gynecol 39:2–6
Mullassery D, Ba’ath ME, Jesudason EC, Losty PD (2010) Value of liver herniation in prediction of outcome in fetal congenital diaphragmatic hernia: a systematic review and meta-analysis. Ultrasound Obstet Gynecol 35:609–614
Victoria T, Danzer E, Oliver ER et al (2018) Right congenital diaphragmatic hernias: is there a correlation between prenatal lung volume and postnatal survival, as in isolated left diaphragmatic hernias. Fetal Diagn Ther 43:12–18
Pinton A, Boubnova J, Becmeur F et al (2020) Is laterality of congenital diaphragmatic hernia a reliable prognostic factor? French national cohort study. Prenat Diagn 40:949–957
Danzer E, Chock VY, Chung S et al (2022) Image-based prenatal predictors of postnatal survival, extracorporeal life support, and defect size in right congenital diaphragmatic hernia. J Perinatol 42:1202–1209
Romiti A, Viggiano M, Conforti A et al (2020) Ultrasonographic assessment of mediastinal shift angle (MSA) in isolated left congenital diaphragmatic hernia for the prediction of postnatal survival. J Matern Fetal Neonatal Med 33:1330–1335
Romiti A, Viggiano M, Savelli S et al (2022) Comparison of mediastinal shift angles obtained with ultrasound and magnetic resonance imaging in fetuses with isolated left sided congenital diaphragmatic hernia. J Matern Fetal Neonatal Med 35:269–274
Amodeo I, Borzani I, Corsani G et al (2022) Fetal MRI mediastinal shift angle and respiratory and cardiovascular pharmacological support in newborns with congenital diaphragmatic hernia. Eur J Pediatr 181:323–334
Savelli S, Bascetta S, Carducci C et al (2020) Fetal MRI assessment of mediastinal shift angle in isolated left congenital diaphragmatic hernia: a new postnatal survival predictive tool. Prenat Diagn 40:136–141
Ba’ath ME, Jesudason EC, Losty PD (2007) How useful is the lung-to-head ratio in predicting outcome in the fetus with congenital diaphragmatic hernia? A systematic review and meta-analysis. Ultrasound Obstet Gynecol 30:897–906
Knox E, Lissauer D, Khan K, Kilby M (2010) Prenatal detection of pulmonary hypoplasia in fetuses with congenital diaphragmatic hernia: a systematic review and meta-analysis of diagnostic studies. J Matern Fetal Neonatal Med 23:579–588
Jani J, Nicolaides KH, Keller RL et al (2007) Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol 30:67–71
Zamora IJ, Olutoye OO, Cass DL et al (2014) Prenatal MRI fetal lung volumes and percent liver herniation predict pulmonary morbidity in congenital diaphragmatic hernia (CDH). J Pediatr Surg 49:688–693
Rypens F, Metens T, Rocourt N et al (2001) Fetal lung volume: estimation at MR imaging-initial results. Radiology 219:236–241
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5:1315–1316
Ding W, Gu Y, Wu H et al (2023) Mediastinal shift angle (MSA) measurement with MRI: a simple and effective tool for prenatal risk stratification in fetuses with congenital diaphragmatic hernia. Eur Radiol 33:1668–1676
Butler N, Claireaux AE (1962) Congenital diaphragmatic hernia as a cause of perinatal mortality. Lancet 1:659–663
Russo FM, Eastwood MP, Keijzer R et al (2017) Lung size and liver herniation predict need for extracorporeal membrane oxygenation but not pulmonary hypertension in isolated congenital diaphragmatic hernia: systematic review and meta-analysis. Ultrasound Obstet Gynecol 49:704–713
Recio Rodríguez M, Martínez de Vega V, Cano Alonso R, Carrascoso Arranz J, Ten Martínez P, Pérez Pedregosa J (2012) MR imaging of thoracic abnormalities in the fetus. Radiographics 32:E305-321
Skari H, Bjornland K, Haugen G, Egeland T, Emblem R (2000) Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg 35:1187–1197
Midrio P, Gobbi D, Baldo V, Gamba P (2007) Right congenital diaphragmatic hernia: an 18-year experience. J Pediatr Surg 42:517–521
Fisher JC, Jefferson RA, Arkovitz MS, Stolar CJ (2008) Redefining outcomes in right congenital diaphragmatic hernia. J Pediatr Surg 43:373–379
Skari H, Bjornland K, Frenckner B et al (2002) Congenital diaphragmatic hernia in Scandinavia from 1995 to 1998: predictors of mortality. J Pediatr Surg 37:1269–1275
Slavotinek AM, Warmerdam B, Lin AE, Shaw GM (2007) Population-based analysis of left- and right-sided diaphragmatic hernias demonstrates different frequencies of selected additional anomalies. Am J Med Genet A 143A:3127–3136
Schaible T, Kohl T, Reinshagen K et al (2012) Right- versus left-sided congenital diaphragmatic hernia: postnatal outcome at a specialized tertiary care center. Pediatr Crit Care Med 13:66–71
Colvin J, Bower C, Dickinson JE, Sokol J (2005) Outcomes of congenital diaphragmatic hernia: a population-based study in Western Australia. Pediatrics 116:e356-363
Wilson JM, Lund DP, Lillehei CW, Vacanti JP (1997) Congenital diaphragmatic hernia–a tale of two cities: the Boston experience. J Pediatr Surg 32:401–405
Abramov A, Fan W, Hernan R et al (2020) Comparative outcomes of right versus left congenital diaphragmatic hernia: a multicenter analysis. J Pediatr Surg 55:33–38
Beaumier CK, Beres AL, Puligandla PS, Skarsgard ED, Network CPS (2015) Clinical characteristics and outcomes of patients with right congenital diaphragmatic hernia: a population-based study. J Pediatr Surg 50:731–733
Hedrick HL, Danzer E, Merchant AM et al (2007) Liver position and lung-to-head ratio for prediction of extracorporeal membrane oxygenation and survival in isolated left congenital diaphragmatic hernia. Am J Obstet Gynecol 197:422.e1–4
Weis M, Hoffmann S, Henzler C et al (2018) Isolated impact of liver herniation on outcome in fetuses with congenital diaphragmatic hernia - a matched-pair analysis based on fetal MRI relative lung volume. Eur J Radiol 105:148–152
Hedrick HL, Crombleholme TM, Flake AW et al (2004) Right congenital diaphragmatic hernia: prenatal assessment and outcome. J Pediatr Surg 39:319–323 (discussion 319-323)
Acknowledgements
We thank Guangdong Science and Technology Department, Guangzhou Science and Technology Program and Fetal Medicine Foundation of Guangzhou Women and Children’s Medical Center for supporting research on congenital diaphragmatic hernia.
Funding
This study has received funding from the Major Projects of Guangdong Science and Technology Department, China (Grant No. 2019B020227001, No. 2019B030301004), the key projects of Guangzhou Science and Technology Program, China (Grant No. 202102010016), and Fetal Medicine Foundation of Guangzhou Women and Children’s Medical Center (Grant No.4001027).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yuanyuan Gu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because of the retrospective nature of the study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Study subjects or cohorts have never been previously reported.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ding, W., Gu, Y., Wang, H. et al. Prenatal MRI assessment of mediastinal shift angle as a feasible and effective risk stratification tool in isolated right-sided congenital diaphragmatic hernia. Eur Radiol 34, 1524–1533 (2024). https://doi.org/10.1007/s00330-023-10178-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10178-1