Abstract
Objective
To develop and validate a deep learning (DL) model based on CT for differentiating bone islands and osteoblastic bone metastases.
Materials and methods
The patients with sclerosing bone lesions (SBLs) were retrospectively included in three hospitals. The images from site 1 were randomly assigned to the training (70%) and intrinsic verification (10%) datasets for developing the two-dimensional (2D) DL model (single-slice input) and “2.5-dimensional” (2.5D) DL model (three-slice input) and to the internal validation dataset (20%) for evaluating the performance of both models. The diagnostic performance was evaluated using the internal validation set from site 1 and additional external validation datasets from site 2 and site 3. And statistically analyze the performance of 2D and 2.5D DL models.
Results
In total, 1918 SBLs in 728 patients in site 1, 122 SBLs in 71 patients in site 2, and 71 SBLs in 47 patients in site 3 were used to develop and test the 2D and 2.5D DL models. The best performance was obtained using the 2.5D DL model, which achieved an AUC of 0.996 (95% confidence interval [CI], 0.995–0.996), 0.958 (95% CI, 0.958–0.960), and 0.952 (95% CI, 0.951–0.953) and accuracies of 0.950, 0.902, and 0.863 for the internal validation set, the external validation set from site 2 and site 3, respectively.
Conclusion
A DL model based on a three-slice CT image input (2.5D DL model) can improve the prediction of osteoblastic bone metastases, which can facilitate clinical decision-making.
Key Points
• This study investigated the value of deep learning models in identifying bone islands and osteoblastic bone metastases.
• Three-slice CT image input (2.5D DL model) outweighed the 2D model in the classification of sclerosing bone lesions.
• The 2.5D deep learning model showed excellent performance using the internal (AUC, 0.996) and two external (AUC, 0.958; AUC, 0.952) validation sets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Computed tomography (CT) is widely used for detecting, evaluating, and staging malignant tumors, and sclerosing bone lesions are frequently detected on CT images [1, 2]. Distinguishing a sclerosing bone lesion from an osteoblastic bone metastasis or bone island is essential to determine the next diagnostic steps and prepare a treatment strategy. For patients with a non-tumor history, diagnosing bone islands does not require treatment, and diagnosing osteoblastic bone metastases requires the primary lesion to be found to determine a treatment plan. For tumor patients, distinguishing bone islands from osteoblastic bone metastases can change tumor staging and alter treatment options.
To differentiate between bone islands and osteoblastic bone metastases, many methods have improved the diagnosis of sclerosing bone lesions, such as positron emission tomography (PET)/CT [3], dual-energy CT [4], identification of the salt-and-pepper noise sign in magnetic resonance (MR) images [5], CT attenuation measurements [6], and radiomics [7]. However, PET/CT, dual-energy CT, and MR examinations cannot be performed in many remote locations, and when they can be performed, they increase the financial burden of patients. In addition, radiomic methods and CT attenuation measurements rely on the precise delineation of regions of interest (ROIs), which is largely affected by human factors.
In contrast, advanced deep learning (DL) models overcome these problems by using powerful feature learning capabilities [8, 9] and have shown the potential to help humans in various medical fields [10,11,12]. In addition, unlike radiomic methods, a classification model based on DL does not require precise delineation of tumor boundaries and can automatically learn to classify features in image data and diagnose conditions accordingly. Moreover, external verification does not require accurate delineation of the lesions, increasing the possibility of using the model in various medical institutions.
In this study, we constructed a DL model to differentiate between bone islands and osteoblastic bone metastases. Our approach used an end-to-end pipeline that only required the manual selection of lesion regions in CT images and did not require precise lesion boundary segmentation or human-defined features. The proposed model needed only simple lesion delineation to diagnose sclerosing bone lesions. To evaluate the DL model’s performance, we collected two datasets from two independent hospitals and independently validated the results.
Materials and methods
Datasets
This multicenter retrospective study was conducted in three hospitals in China. The institutional review board of the principal investigator’s hospital approved the study and waived the requirement for written informed consent.
For the development dataset, we evaluated chest and abdominal CT images acquired at Guangzhou Red Cross Hospital, Guangzhou, China from January 1, 2013, to March 31, 2022, that were reported to contain a bone island or osteoblastic bone metastases and for patients with a history of malignancy with high-density bone lesions. Initially, 1376 patients were recruited. Those who met the following criteria were diagnosed with a bone island: (1) no history of malignancy; (2) lesions denser than trabecular bone that were round or oblong or with speculated margin [6, 13, 14]; (3) no change in size, shape, and density on follow-up CT scans obtained at least 6 months later [7]; and (4) lesions displayed on at least three consecutive CT slices. Patients who met the following criteria were diagnosed with osteoblastic bone metastases: (1) history of malignancy; (2) no bone metastases identified during previous imaging examinations, and local high-density lesions with a maximum diameter of < 2 cm in the vertebral body or pelvic bone identified in the most recent CT image; (3) lesions displayed on at least three consecutive CT slices; (4) no history of chemotherapy, antiandrogen therapy, or bisphosphonate therapy prior to discovering high-density lesions [6]; and (5) no pathological fractures. Applying the above diagnostic criteria, two experienced radiologists (L.Z.P. and X.F., with 21 and 9 years, respectively, in musculoskeletal radiology) excluded 648 patients, leaving 728 (498 cases of bone islands and 230 cases of osteoblastic bone metastases) enrolled in this study (Fig. 1).
To verify the DL model’s utility in clinical practice, two external validation datasets containing CT images of bone islands and osteoblastic bone metastases acquired between January 1, 2019, and December 31, 2021, were also obtained from Guangzhou Cancer Hospital (GZCH), Guangzhou, China and Wuhan Third Hospital (WHTH), Wuhan, China.
Image reading and annotation
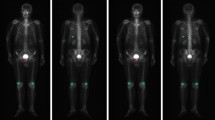
According to the diagnosis, images were labeled as bone islands or osteoblastic bone metastases. All CT images were preprocessed on a bone window (window level, 400 HU; window width, 2000 HU). The lesion ROI was manually assigned layer-by-layer with bounding boxes on the CT images from three hospitals by two experienced radiologists (L.Z.P. and X.F.) using the LabelImg software (https://pypi.org/project/labelImg/) and annotated. To apply the DL model, ROIs containing the lesion were manually selected according to the following rules: (1) the ROI of each layer should include the complete lesion area and lesion’s margin; and (2) the number of layers chosen to delineate the lesion should be a multiple of three (Fig. 2a). The rule was implemented easily in practice because it allowed some layers of the lesion to be discarded and the lesion did not need to be exactly in the center of the ROI.
Development of the DL model
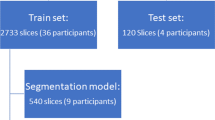
All analyses were performed using Python-based programs. Transfer learning was applied using the ResNet-18 DL model as the basic architecture of the convolutional neural network (CNN). The images from Guangzhou Red Cross Hospital were randomly assigned to the training (70%) and intrinsic verification (10%) datasets for developing the DL model and to the internal validation dataset (20%) for evaluating the DL model’s performance. The data input to the network (Supplementary Figure S1) was divided into a single-slice input (224 × 224 × 1 voxels) and a three-slice input (224 × 224 × 3 voxels) to build two-dimensional (2D) and “2.5-dimensional” (2.5D) DL models, respectively (Fig. 2b). Details of the data preprocessing and the model development are described in the Supplementary Material. The code used for training is stored in GitHub (https://github.com/Xiongyuchao/OBMORBINet).
Validation of the DL model
The trained 2D and 2.5D DL models were applied to the internal and external test sets. The overall workflow of the 2D and 2.5D DL model development is displayed in Fig. 1.
Statistical analysis
We used receiver operating characteristic (ROC) curves to demonstrate the ability of DL algorithms to classify sclerosing bone lesions. A ROC curve is generated by plotting the ratio of true positive (TP) cases (sensitivity) to false positive (FP) cases (specificity) by varying the predicted probability threshold. A larger area under the ROC curve (AUC) indicates better diagnostic performance. The code used for data analysis is stored in GitHub (https://github.com/XiongyuchaoOBMORBINet).
Results
Clinical characteristics
Clinical characteristics of the development and external test sets are summarized in Table 1. The development set included 9066 images of 1918 sclerosing bone lesions in 498 patients with bone islands and 230 patients with osteoblastic bone metastases. The WHTH external test set included 1071 images of 122 sclerosing bone lesions in 56 patients with bone islands and 15 patients with osteoblastic bone metastases. The GZCH external test set included 525 images of 71 sclerosing bone lesions in 38 patients with bone islands and 9 patients with osteoblastic bone metastases. Detailed patient and lesion information is provided in the Supplementary Material.
Establishment of the DL model
After 19 epochs, the training procedure was ended, with no further improvement in accuracy and cross-entropy loss on training and verification for 2D and 2.5D DL models. Using the 2D DL model, an accuracy of up to 98.3% was observed for the training set and 96.1% for the intrinsic verification set. Using the 2.5D DL model, an accuracy of up to 99.7% was observed for the training set and 98.7% for the intrinsic verification set.
Performance of the 2D and 2.5D DL models
Both 2D and 2.5D DL models accurately distinguished sclerosing bone lesions in all three validation datasets. The accuracies for the internal validation dataset, external validation dataset from WHTH, and external validation dataset from GZCH were 0.854, 0.871, and 0.806, respectively, for the 2D DL model and 0.950, 0.902, and 0.863, respectively, for the 2.5D DL model (Table 2). Similarly, high AUC values were observed for all three validation datasets, and the AUC of the 2.5D DL model was higher than that of the 2D DL model (Fig. 3). The AUC values for the internal validation dataset, external validation dataset from WHTH, and external validation dataset from GZCH were 0.981(95% CI, 0.980–0.981), 0.940 (95% CI, 0.940–0.941), and 0.890 (95% CI, 0.890–0.892), respectively, for the 2D DL model and 0.996 (95% CI, 0.995–0.996), 0.958 (95% CI, 0.958–0.960), and 0.952 (95% CI, 0.951–0.953), respectively, for the 2.5D DL model. Figure 4 shows confusion matrices for the internal validation dataset, external validation dataset from WHTH, and external validation dataset from GZCH.
Using the 2.5D DL model, the positive predictive values (PPVs) for the internal validation dataset, external validation dataset from WHTH, and external validation dataset from GZCH were 0.983, 0.960, and 0.843, respectively. The proportion of false negative (FN) detections was less than 4.13% for all validation datasets, 0.83% for the internal validation dataset, 8.12% for the external validation dataset from WHTH, and 4.57% for the external validation dataset from GZCH (Table 2).
Using the 2.5D DL model (Fig. 5), FN detections were obtained for 62 three-slice data from 36 lesions, including 25 three-slice data from 14 lesions in the internal validation dataset, 29 three-slice data from 16 lesions in the external validation dataset from WHTH, and 8 three-slice data from 6 lesions in the external validation dataset from GZCH. Of the 36 lesions with FN detections, 25 contained errors in all three-slice data, 11 contained errors in some three-slice data, and 26 of these lesions (41 three-slice data) were adjacent to cortical bone (Supplementary Table S1).
Using the 2.5D DL model, FP detections were obtained for 27 three-slice data from 18 lesions, including 5 three-slice data from 3 lesions in the internal validation dataset, six three-slice data from 3 lesions in the external validation dataset from WHTH, and 16 three-slice data from 12 lesions in the external validation dataset from GZCH. Of the 18 lesions with FP detections, 8 contained errors in all three-slice data, 10 contained errors in some three-slice data, and 7 were adjacent to cortical bone (Supplementary Table S2).
Discussion
In this study, we separately developed DL models with a single-slice image input (2D DL model) and a continuous three-slice image input (2.5D DL model) to characterize sclerosing bone lesions detected by radiologists using CT. The 2.5D DL model was better able to differentiate between bone islands and osteoblastic bone metastases, with AUC values of 0.996, 0.958, and 0.952 for the internal validation dataset, external validation dataset from WHTH, and external validation dataset from GZCH, respectively; the corresponding values for the 2D DL model were 0.981, 0.940, and 0.890, respectively. The 2.5D DL model differentiated between bone islands and osteoblastic bone metastases in the internal and external validation datasets with high accuracy, sensitivity, and specificity. To the best of our knowledge, this is the first multicenter study to differentiate sclerosing bone lesions using DL.
Although CT has greatly helped to directly distinguish between bone islands and osteoblastic bone metastases using features such as thorny radiation [15], periosteal reaction, soft tissue involvement, and bone destruction [16], only large sclerosing bone lesions can be analyzed and sclerosing bone lesions are often not accompanied by such recognizable imaging features. CT attenuation measurements [6, 13, 17] have shown promising potential to differentiate between bone islands and osteoblastic bone metastases, but their clinical applicability has been jeopardized because CT values are affected by factors such as the region selected for measurement, patient size [18], CT acquisition parameters, and image reconstruction algorithm parameters [19, 20]. CT temporal subtraction is capable of distinguishing osteoblastic bone metastases from bone islands, but its utility is significantly limited for patients with bone islands and those who have osteoblastic bone metastases but received no follow-up CT scan to minimize radiation exposure and/or cost [21, 22]. Several studies [3,4,5] have explored the potential value of further imaging for diagnosing bone islands and osteoblastic bone metastases. Spectral CT is helpful for distinguishing osteoblastic bone metastases from bone islands, particularly when using the standard deviation of CT values on high-energy virtual monochromatic spectral images [4]. The salt-and-pepper noise sign in bone islands on chemical-shift-encoded MR images can help to differentiate between bone islands and osteoblastic bone metastases [5]. PET/CT helps to differentiate sclerosing bone lesions by assessing tracer uptake [3]. Although the aforementioned studies offer many means of distinguishing between bone islands and osteoblastic bone metastases, they require human visual assessment based on expertise and experience, which is operator-dependent and imposes many demands on imaging equipment that cannot be met in remote areas.
Based on the above, there is currently no objective, simple, and low-cost method to differentiate between osteoblastic bone metastases and bone islands. In current clinical practice, images of patients with no history of tumors and sclerosing bone lesions show typical bone islands that are preferentially diagnosed, but atypical manifestations of bone islands may raise a concern about bone metastases. Patients with a history of tumors, especially those associated with prostate cancer and breast cancer, may be concerned about the possibility of osteoblastic bone metastases even when bone islands appear normal. Osteoblastic bone metastases may present with a bone island-like appearance and thus be initially misdiagnosed, which may delay the treatment of osteoblast bone metastases in tumor patients. There is an urgent need for objective, simple, and low-cost methods to differentiate between osteoblastic bone metastases and bone islands to avoid excessive medical examination of patients with bone islands and delayed treatment of patients with osteoblastic bone metastases.
DL exploits large datasets by directly learning the correlation between complex structures in raw input data and target outputs [23]. Numerous studies have reported the applicability of DL to tumor diagnosis in radiology [24]. However, many that evaluate well-functioning DL models carry a large risk of bias [25]. Using an external cohort is an important validation step to test for bias in DL systems [26]. In this study, the 2.5D DL model yielded a favorable AUC, sensitivity, and specificity for the internal and external test datasets, which indicated that the model could correctly distinguish between bone islands and osteoblastic bone metastases and showed very good generalizability. Hong et al [7] found that CT-based radiomics was helpful for distinguishing between bone islands and osteoblastic bone metastases and yielded better diagnostic performance compared with inexperienced radiologists. Radiomics is a traditional machine learning method that uses carefully chosen representations of input data to predict target outputs. Modern DL techniques are based on CNNs, which use highly flexible artificial neural networks to directly correlate input data to target outputs, and the relationships learned through this correlation are often true [23, 26, 27]. In our study, several advantages of the 2.5D DL model can be highlighted compared with radiomics for distinguishing bone islands from osteoblastic bone metastases. First, the ROI selection based on CNN-based DL only needs to include the complete lesion instead of accurately delineating the lesion edge layer by layer, as in radiomics. This advantage also makes the model more likely to be widely used in other hospitals at all levels. Second, our study recruited more patients, and a larger sample size could obviously ensure better reliability of the classification model, as confirmed by the performance of the 2.5D DL model using the internal and external test datasets. Third, CNN-based DL uses straightforward end-to-end problem-solving that removes the limitations of hand-crafted radiomics features.
The accurate classification of bone islands and osteoblastic bone metastases is of great significance for China, which has a large population, huge differences among the levels of medical resources, and extremely minimal medical insurance funds. Accurate diagnosis of sclerosing bone lesions as bone islands could reduce patient anxiety and the burden on the medical system by avoiding biopsies of benign lesions and unnecessary further imaging studies. The diagnosis of sclerosing bone lesions as osteoblastic bone metastases could allow patients to receive appropriate treatment earlier. However, in current clinical practice, radiologists with different subspecialties have different subjective interpretations of sclerosing bone lesions. Our 2.5D DL model can accurately classify bone islands and osteoblastic bone metastases by simply delineating lesions, which further emphasizes its great clinical value and social benefits. Noguchi et al developed a DL model to identify bone metastases on CT images and this model achieved excellent performance [28]. However, its sensitivity and PPV for osteoblastic bone metastases were significantly lower than those achieved using our 2.5D DL model. Nevertheless, our model can be well combined with that of Noguchi et al to improve the accuracy of osteoblastic bone metastases, which further highlights the clinical value of our study.
In clinical practice, we are more concerned with FN detections produced by the 2.5D DL model. These may result from an ROI that includes adjacent cortical bone. Therefore, we suggest that when radiologists use the 2.5D DL model for osteoblastic bone lesion identification, they should be cautious when lesions are adjacent to cortical bone. Given the urgency of treating osteoblastic bone metastases, the necessary follow-up can be considered cost-effective.
Despite the remarkable results, our study also has some potential limitations. First, the features used by the DL model for classification are difficult to interpret. Therefore, when the doctor’s judgment differs from that of the trained model, the difference cannot be resolved by discussion. Second, this study was retrospective and may suffer from selection bias. Bone islands may be underreported, and many radiologists may not comment on this type of lesion in their reports. Third, only lesions displayed in consecutive slices of three-slice CT images were included in this study. Fourth, this study ignored bone metastases in several locations other than the vertebral body or pelvic bone, the inclusion of which is the goal of our future research.
In conclusion, we developed a classification model of bone islands and osteoblastic bone metastases that achieved high diagnostic accuracy across different hospitals. The 2.5D DL model demonstrated high accuracy, sensitivity, and specificity in differentiating between bone islands and osteoblastic bone metastases in the internal and external validation datasets. Our proposed DL model is simpler and more accurate than other radiomic models and can be generalized.
Abbreviations
- AUC:
-
Area under the ROC curve
- CI:
-
Confidence interval
- CNN:
-
Convolutional neural network
- CT:
-
Computed tomography
- DL:
-
Deep learning
- MRI:
-
Magnetic resonance imaging
- PACS:
-
Picture archiving and communication systems
- PET:
-
Positron emission tomography
- ROC:
-
Receiver operating characteristic
- ROIs:
-
Lesion regions of interest
References
Woo S, Ghafoor S, Vargas HA (2019) Contribution of radiology to staging of prostate cancer. Semin Nucl Med 49:294–301
Bychkovsky BL, Lin NU (2017) Imaging in the evaluation and follow-up of early and advanced breast cancer: when, why, and how often? Breast 31:318–324
Wu J, Wang Y, Liao T et al (2021) Comparison of the relative diagnostic performance of [(68)Ga]Ga-DOTA-FAPI-04 and [(18)F]FDG PET/CT for the detection of bone metastasis in patients with different cancers. Front Oncol 11:737827
Dong Y, Zheng S, Machida H et al (2015) Differential diagnosis of osteoblastic metastases from bone islands in patients with lung cancer by single-source dual-energy CT: advantages of spectral CT imaging. Eur J Radiol 84:901–907
Jeon SW, Kwack KS, Yun JS, Gho SM, Park S (2020) Salt-and-pepper noise sign on fat-fraction maps by chemical-shift-encoded mri: a useful sign to differentiate bone islands from osteoblastic metastases-a preliminary study. AJR Am J Roentgenol 214:1139–1145
Ulano A, Bredella MA, Burke P et al (2016) Distinguishing untreated osteoblastic metastases from enostoses using CT attenuation measurements. AJR Am J Roentgenol 207:362–368
Hong JH, Jung JY, Jo A et al (2021) Development and validation of a radiomics model for differentiating bone islands and osteoblastic bone metastases at abdominal CT. Radiology 299:626–632
Heaven D (2019) Why deep-learning AIs are so easy to fool. Nature 574:163–166
Landhuis E (2020) Deep learning takes on tumours. Nature 580:551–553
Mu W, Jiang L, Shi Y et al (2021) Non-invasive measurement of PD-L1 status and prediction of immunotherapy response using deep learning of PET/CT images. J Immunother Cancer 9:e002118
Xu Y, Hosny A, Zeleznik R et al (2019) Deep learning predicts lung cancer treatment response from serial medical imaging. Clin Cancer Res 25:3266–3275
Capobianco N, Meignan M, Cottereau AS et al (2021) Deep-learning (18)F-FDG uptake classification enables total metabolic tumor volume estimation in diffuse large B-cell lymphoma. J Nucl Med 62:30–36
Elangovan SM, Sebro R (2018) Accuracy of CT attenuation measurement for differentiating treated osteoblastic metastases from enostoses. AJR Am J Roentgenol 210:615–620
Bedard T, Mohammed M, Serinelli S, Damron TA (2020) Atypical enostoses-series of ten cases and literature review. Medicina (Kaunas) 56(10):534
Greenspan A (1995) Bone island (enostosis): current concept–a review. Skeletal Radiol 24:111–115
Nguyen M, Beaulieu C, Weinstein S, Shin LK (2017) The incidental bone lesion on computed tomography: management tips for abdominal radiologists. Abdom Radiol (NY) 42:1586–1605
Sala F, Dapoto A, Morzenti C et al (2019) Bone islands incidentally detected on computed tomography: frequency of enostosis and differentiation from untreated osteoblastic metastases based on CT attenuation value. Br J Radiol 92:20190249
Ai HA, Meier JG, Wendt RE 3rd (2018) HU deviation in lung and bone tissues: characterization and a corrective strategy. Med Phys 45:2108–2118
Lamba R, McGahan JP, Corwin MT et al (2014) CT Hounsfield numbers of soft tissues on unenhanced abdominal CT scans: variability between two different manufacturers’ MDCT scanners. AJR Am J Roentgenol 203:1013–1020
Zurl B, Tiefling R, Winkler P, Kindl P, Kapp KS (2014) Hounsfield units variations: impact on CT-density based conversion tables and their effects on dose distribution. Strahlenther Onkol 190:88–93
Onoue K, Nishio M, Yakami M et al (2019) CT temporal subtraction improves early detection of bone metastases compared to SPECT. Eur Radiol 29:5673–5681
Hoshiai S, Hanaoka S, Masumoto T et al (2022) Effectiveness of temporal subtraction computed tomography images using deep learning in detecting vertebral bone metastases. Eur J Radiol 154:110445
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts H (2018) Artificial intelligence in radiology. Nat Rev Cancer 18:500–510
Nagendran M, Chen Y, Lovejoy CA et al (2020) Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies. BMJ 368:m689
Kleppe A, Skrede OJ, De Raedt S, Liestol K, Kerr DJ, Danielsen HE (2021) Designing deep learning studies in cancer diagnostics. Nat Rev Cancer 21:199–211
Schmidhuber J (2015) Deep learning in neural networks: an overview. Neural Netw 61:85–117
Noguchi S, Nishio M, Sakamoto R et al (2022) Deep learning-based algorithm improved radiologists’ performance in bone metastases detection on CT. Eur Radiol 32(11):7976–7987
Acknowledgements
We thank Liwen Bianji (Edanz) (www.liwenbianji.cn/ac) for editing the language of a draft of this manuscript.
Funding
The authors state that this study has received funding from the Guangzhou Planned Project of Science and Technology, China [grant numbers: 202102010102] (XWZ). Guangzhou Science and Technology Project of Health, China [grant numbers: 20211A010019] (FX), Guangzhou Planned Project of Science and Technology [grant numbers: 202102010031] (YYL). Guangdong Basic and Applied Basic Research Foundation [grant numbers: 2021A1515110703] (YYL).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Fan Xu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board for the retrospective cases.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• multicenter study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiong, Y., Guo, W., Liang, Z. et al. Deep learning–based diagnosis of osteoblastic bone metastases and bone islands in computed tomograph images: a multicenter diagnostic study. Eur Radiol 33, 6359–6368 (2023). https://doi.org/10.1007/s00330-023-09573-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09573-5