Abstract
Objectives
To evaluate the associations of the radiological features of subcutaneous adipose tissue (SAT) and visceral adipose tissue (VAT) with the postoperative complications and overall survival (OS) of patients undergoing laparoscopic radical gastrectomy for gastric cancer.
Methods
One hundred forty-two patients underwent laparoscopic radical gastrectomy for gastric cancer from February 2013 to May 2016. The radiological features of SAT and VAT were studied by preoperative computed tomography, and the relationships between the parameters of adipose tissues and the intraoperative and postoperative conditions and OS rate of patients were evaluated.
Results
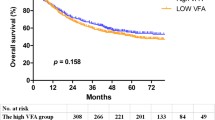
A positive linear correlation was found between VAT area and operation duration, and a negative linear correlation was found between VAT density and intraoperative blood loss (p < 0.05 in both). VAT area was an independent risk factor for postoperative complications. VAT area and VAT density were independent risk factors for OS in gastric cancer.
Conclusions
A high VAT area was an independent risk factor for postoperative complications of gastric cancer, whereas a low VAT area and high VAT density were independent risk factors for poor prognosis in terms of OS in gastric cancer.
Key Points
• A large visceral adipose tissue (VAT) area is an unfavourable factor affecting the outcomes of radical gastrectomy for gastric cancer.
• Low VAT density may be more likely to cause intraoperative bleeding.
• VAT area and VAT density were independent risk factors for the OS of patients with gastric cancer.



Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- HU:
-
Hounsfield unit
- OS:
-
Overall survival
- RFS:
-
Relapse-free survival
- SAT:
-
Subcutaneous adipose tissue
- VAT:
-
Visceral adipose tissue
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394-424
Baiocchi GL, Giacopuzzi S, Reim D et al (2020) Incidence and grading of complications after gastrectomy for cancer using the GASTRODATA Registry: a European Retrospective Observational Study. Ann Surg 272:807–813
Nelen SD, Bosscha K, Lemmens VEPP et al (2018) Morbidity and mortality according to age following gastrectomy for gastric cancer. Br J Surg 105:1163–1170
Toriumi T, Makuuchi R, Satosh K et al (2020) Obesity is a risk factor for internal hernia after laparoscopic or robot-assisted gastrectomy with mesenteric defect closure for gastric cancer. Surg Endosc 34:436–442
Chen XD, Mao CC, Zhang WT et al (2017) A quantified risk-scoring system and rating model for postsurgical gastroparesis syndrome in gastric cancer patients. J Surg Oncol 116:533–544
Steffen A, Huerta JM, Weiderpass E et al (2015) General and abdominal obesity and risk of esophageal and gastric adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 137:646–657
Kapoor ND, Twining PK, Groot OQ et al (2020) Adipose tissue density on CT as a prognostic factor in patients with cancer: a systematic review. Acta Oncol 59:1488–1495
Lee JW, Son MW, Chung IK, Cho YS, Lee MS, Lee SM (2020) Significance of CT attenuation and F-18 fluorodeoxyglucose uptake of visceral adipose tissue for predicting survival in gastric cancer patients after curative surgical resection. Gastric Cancer 23:273–284
Taniguchi Y, Kurokawa Y, Takahashi T et al (2021) Impacts of preoperative psoas muscle mass and visceral fat area on postoperative short- and long-term outcomes in patients with gastric cancer. World J Surg 45:815–821
Peng YC, Wu CH, Tien YW et al (2021) Preoperative sarcopenia is associated with poor overall survival in pancreatic cancer patients following pancreaticoduodenectomy. Eur Radiol 31:2472–2481
Heus C, Smorenburg A, Stoker J et al (2021) Visceral obesity and muscle mass determined by CT scan and surgical outcome in patients with advanced ovarian cancer. A retrospective cohort study. Gynecol Oncol 160:187–192
Wang SL, Ma LL, Chen XY et al (2018) Impact of visceral fat on surgical complications and long-term survival of patients with gastric cancer after radical gastrectomy. Eur J Clin Nutr 72:436–445
Murphy RA, Register TC, Shively CA et al (2014) Adipose tissue density, a novel biomarker predicting mortality risk in older adults. J Gerontol A Biol Sci Med Sci 69:109–117
Rosenquist KJ, Massaro JM, Pedley A et al (2015) Fat quality and incident cardiovascular disease, all-cause mortality, and cancer mortality. J Clin Endocrinol Metab 100:227–234
Lee JJ, Pedley A, Hoffmann U et al (2016) Cross-sectional associations of computed tomography (CT)-derived adipose tissue density and adipokines: The Framingham Heart Study. J Am Heart Assoc 5:e002545
McDonald AM, Fiveash JB, Kirkland RS et al (2017) Subcutaneous adipose tissue characteristics and the risk of biochemical recurrence in men with high-risk prostate cancer. Urol Oncol 35:663.e15–663.e21
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Shen W, Punyanitya M, Wang ZM et al (1985) (2004) Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol (1985) 97:2333–2338
Veld J, Vossen JA, De ABK et al (2016) Adipose tissue and muscle attenuation as novel biomarkers predicting mortality in patients with extremity sarcomas. Eur Radiol 26:4649–4655
Examination Committee of Criteria for “Obesity Disease” in Japan, Japan Society for the Study of Obesity (2002) New criteria for “obesity disease” in Japan. Circulation Journal 66:987–992
Huang ZN, Ma YB, Chen QY et al (2022) Potential survival benefits of open over laparoscopic radical gastrectomy for gastric cancer patients beyond three years after surgery: result from multicenter in-depth analysis based on propensity matching. Surg Endosc 36:1456–1465
Mu L, Liu J, Zhou GH et al (2021) Obesity prevalence and risks among Chinese adults: findings from the China PEACE Million Persons Project, 2014-2018. Circ Cardiovasc Qual Outcomes 14:e007292
Lee JH, Park DJ, Kim HH et al (2012) Comparison of complications after laparoscopy-assisted distal gastrectomy and open distal gastrectomy for gastric cancer using the Clavien-Dindo classification. Surg Endosc 26:1287–1295
Kunisaki C (2010) Reply to 090220: re: ‘predictive factors for surgical complications of laparoscopy-assisted distal gastrectomy for gastric cancer’ (Epub 31 Dec 08). Surg Endosc 24:247
Schwarz RE (2012) Obesity and postgastrectomy outcomes: large risks, fat chances, or no big deal? Gastric Cancer 15:121–123
Katai H, Mizusawa J, Katayama H et al (2019) Single-arm confirmatory trial of laparoscopy-assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group study JCOG1401. Gastric Cancer 22:999–1008
Muto M, Ezoe Y, Yano T et al (2012) Usefulness of endoscopic radial incision and cutting method for refractory esophagogastric anastomotic stricture (with video). Gastrointestinal Endoscopy 75(5):965–972
Miki Y, Tokunaga M, Bando E et al (2011) Evaluation of postoperative pancreatic fistula after total gastrectomy with D2 lymphadenectomy by ISGPF classification. J Gastrointest Surg 15:1969–1976
Parikh NI, Keyes MJ, Larson MG et al (2009) Visceral and subcutaneous adiposity and brachial artery vasodilator function. Obesity (Silver Spring) 17:2054–2059
Lind L, Strand R, Kullberg J et al (2021) Cardiovascular-related proteins and the abdominal visceral to subcutaneous adipose tissue ratio. Nutr Metab Cardiovasc Dis 31:532–539
Farro G, Stakenborg M, Gomez-Pinilla PJ et al (2017) CCR2-dependent monocyte-derived macrophages resolve inflammation and restore gut motility in postoperative ileus. Gut 68(9):1726
Kim JM, Chung E, Cho ES et al (2021) Impact of subcutaneous and visceral fat adiposity in patients with colorectal cancer. Clin Nutr 40:5631–5638
Matsui R, Inaki N, Tsuji T (2021) Impact of visceral adipose tissue on compliance of adjuvant chemotherapy and relapse-free survival after gastrectomy for gastric cancer: a propensity score matching analysis. Clin Nutr 40:2745–2753
Garcia JM, Shamliyan TA (2017) Omega-3 fatty acids in patients with anorexia-cachexia syndrome associated with malignancy and its treatments. Am J Med 130:1151–1155
Agustsson T, Rydén M, Hoffstedt J et al (2007) Mechanism of increased lipolysis in cancer cachexia. Cancer Res 67:5531–5537
De LM, Mandala M, Rose G (2021) Towards an understanding of the mechanoreciprocity process in adipocytes and its perturbation with aging. Mech Ageing Dev 197:111522
Debari MK, Abbott RD (2020) Adipose tissue fibrosis: mechanisms, models, and importance. Int J Mol Sci 21(17):6030
Ruiz-Ojeda FJ, Méndez-Gutiérrez A, Aguilera CM, Plaza-Díaz J (2019) Extracellular matrix remodeling of adipose tissue in obesity and metabolic diseases. Int J Mol Sci 20(19):4888
Gealekman O, Guseva N, Hartigan C et al (2011) Depot-specific differences and insufficient subcutaneous adipose tissue angiogenesis in human obesity. Circulation 123(2):186–194
Marcelin G, Silveira ALM, Martins LB et al (2019) Deciphering the cellular interplays underlying obesity-induced adipose tissue fibrosis. J Clin Invest 129:4032–4040
Acknowledgements
The authors are grateful for the support from the Wuxi Health Committee and Wuxi translational medicine center.
Funding
This study has received funding from the Top Talent Support Program for young and middle-aged people of the Wuxi Health Committee (No. BJ2020032), major scientific research projects of the Wuxi Health Committee (No. Z201901), and project supported by the Wuxi translational medicine center (No. 2020ZHYB10).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yigang Chen.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Bian, L., Wu, D., Chen, Y. et al. Associations of radiological features of adipose tissues with postoperative complications and overall survival of gastric cancer patients. Eur Radiol 32, 8569–8578 (2022). https://doi.org/10.1007/s00330-022-08918-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08918-w