Abstract
Objectives
Opsoclonus myoclonus ataxia (OMA) syndrome, also known as “Kinsbourne syndrome” or “dancing eye syndrome,” is a rare, paraneoplastic entity which may be associated with pediatric neuroblastic tumors and carry a grave prognosis. We aimed to evaluate the role of 68Ga DOTANOC PET/CT for detecting neuroblastic tumors in patients with OMA syndrome.
Methods
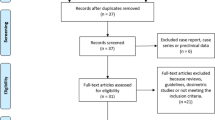
We retrospectively evaluated the 68Ga-DOTANOC PET/CT data of pediatric patients presenting with OMA syndrome from March 2012 to November 2018. A somatostatin receptor (SSTR)-expressing lesion with corresponding morphological change on CT image was considered PET-positive, while no abnormal SSTR expression or lesion was noticed in PET-negative patients. Histopathology and/or clinical/imaging follow-up (minimum one year) was considered a reference standard for comparing the PET/CT findings. The results of 68Ga-DOTANOC PET/CT were also compared with 131I MIBG whole-body scintigraphy, which was available in five patients.
Results
Of 38 patients (13 males, 25 females, aged 3–96 months), 18 (47.3%) had SSTR-expressing lesions (PET-positive), and histopathology revealed neuroblastic tumors in 17/18 lesions (neuroblastoma 14, ganglioneuroblastoma 2, and ganglioneuroma 1) and reactive hyperplasia in 1/18. The remaining 20/38 (52.6%) patients did not demonstrate SSTR-expressing lesions (PET-negative) and had an uneventful follow-up. The average SUVmax of the PET-positive lesions was 10.3 (range 2.8–34.5). The PET/CT results revealed 17 true-positive, one false-positive, 20 true-negative, and zero false-negative. The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 100%, 95.2%, 94.4%, 100%, and 97.3% respectively.
Conclusions
68Ga-DOTANOC PET/CT identified neuroblastic tumors with a high diagnostic accuracy in our cohort compared to histology and follow-up.
Key Points
• Opsoclonus myoclonus ataxia (OMA) syndrome or “dancing eye syndrome” is a rare paraneoplastic entity which may be associated with pediatric neuroblastic tumors with a grave prognosis.
• 123I/131I MIBG imaging has a proven role for functional imaging in neuroblastoma or patients with OMA, but the role of 68Ga-DOTANOC PET/CT is not yet studied.
• 68Ga-labelled DOTANOC PET/CT (SSTR) imaging, in our cohort, was able to positively identify neuroblastic tumors with high diagnostic accuracy when compared with histology.




Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- KeV:
-
Kilo electron volt
- mA:
-
Milli ampere
- MBq:
-
Megabecquerel
- mCi:
-
Millicurie
- MIBG:
-
Metaiodobenzyl guanidine
- MRI:
-
Magnetic resonance imaging
- OMA syndrome:
-
Opsoclonus myoclonus ataxia syndrome
- OSEM:
-
Ordered subset expectation maximization
- PET/CT:
-
Positron emission tomography computed tomography
- SPECT/CT:
-
Single-photon emission tomography/computed tomography
- SSTR:
-
Somatostatin receptor
- SUVmax:
-
Standardized uptake value
- USG:
-
Ultrasonography
References
Pike M (2013) Opsoclonus-myoclonus syndrome. Handb Clin Neurol 112:1209–1211
Kinsbourne M (1962) Myoclonic encephalopathy of infants. J Neurol Neurosurg Psychiatry 25:271–276
Hasegawa S, Matsushige T, Kajimoto M et al (2015) A nationwide survey of opsoclonus-myoclonus syndrome in Japanese children. Brain Dev 37:656–660
Solomon GE, Chutorian AM (1968) Opsoclonus and occult neuroblastoma. N Engl J Med 279:475–477
Sahu JK, Prasad K (2011) The opsoclonus–myoclonus syndrome. Pract Neurol 11:160–166
Russo C, Cohn SL, Petruzzi MJ, de Alarcon PA (1997) Long-term neurologic outcome in children with opsoclonus-myoclonus associated with neuroblastoma: A report from the Pediatric Oncology Group. Med Pediatr Oncol 28:284–288
Blaes F, Dharmalingam B (2016) Childhood opsoclonus-myoclonus syndrome: diagnosis and treatment. Expert Rev Neurother 16:641–648
Matthay KK, Blaes F, Hero B et al (2015) Opsoclonus myoclonus syndrome in neuroblastoma a report from a workshop on the dancing eyes syndrome at the advances in neuroblastoma meeting in Genoa, Italy, 2004. Cancer Lett 228(1–2):275–282
Swart JF, de Kraker J, van der Lely N (2002) Metaiodobenzylguanidine total-body scintigraphy required for revealing occult neuroblastoma in opsoclonus-myoclonus syndrome. Eur J Pediatr 161:255–258
Parisi MT, Hattner RS, Matthay KK, Berg BO, Sandler ED (1993) Optimized diagnostic strategy for neuroblastoma in opsoclonus-myoclonus. J Nucl Med 34:1922–1926
Kroiss A, Putzer D, Uprimny C et al (2011) Functional imaging in phaeochromocytoma and neuroblastoma with 68Ga-DOTA-Tyr3-octreotide positron emission tomography and 123I-metaiodobenzylguanidine. Eur J Nucl Med Mol Imaging 38:865–873
Liu B, Zhuang H, Servaes S (2013) Comparison of [123I] MIBG and [131I] MIBG for imaging of neuroblastoma and other neural crest tumors. Q J Nucl Med Mol Imaging 57:21–28
Pettinato C, Sarnelli A, Di Donna M et al (2008) 68Ga-DOTANOC: biodistribution and dosimetry in patients affected by neuroendocrine tumors. Eur J Nucl Med Mol Imaging 35:72–79
Anderson DJ, Carnahan JF, Michelsohn A, Patterson PH (1991) Antibody markers identify a common progenitor to sympathetic neurons and chromaffin cells in vivo and reveal the timing of commitment to neuronal differentiation in the sympathoadrenal lineage. J Neurosci 11:3507–3519
Parsons XH, Teng YD, Parsons JF, Snyder EY, Smotrich DB, Moore DA (2011) Efficient derivation of human neuronal progenitors and neurons from pluripotent human embryonic stem cells with small molecule induction. J Vis Exp 28:e3273
Hoehner JC, Hedborg F, Eriksson L et al (1998) Developmental gene expression of sympathetic nervous system tumors reflects their histogenesis. Lab Invest 78:29–45
Irtan S, Brisse HJ, Minard-Colin V, Schleiermacher G, Canale S, Sarnacki S (2015) Minimally invasive surgery of neuroblastic tumors in children: indications depend on anatomical location and image-defined risk factors. Pediatr Blood Cancer 62:257–261
Lonergan GJ, Schwab CM, Suarez ES, Carlson CL (2002) Neuroblastoma, ganglioneuroblastoma and ganglioneuroma: radiologic-pathologic correlation. Radiographics 22:911–934
Rudnick E, Khakoo Y, Antunes NL et al (2001) Opsoclonus-myoclonus-ataxia syndrome in neuroblastoma: Clinical outcome and antineuronal antibodies - a report from the Children’s Cancer Group Study. Med Pediatr Oncol 36:612–622
Altman AJ, Baehner RL (1976) Favorable prognosis for survival in children with coincident opso-myoclonus and neuroblastoma. Cancer 37:846–852
Tate ED, Allison TJ, Pranzatelli MR, Verhulst SJ (2005) Neuroepidemiologic trends in 105 US cases of pediatric opsoclonus-myoclonus syndrome. J Pediatr Oncol Nurs 22:8–19
Melzer HI, Coppenrath E, Schmid I et al (2011) 123I-MIBG scintigraphy/SPECT versus 18F-FDG PET in paediatric neuroblastoma. Eur J Nucl Med Mol Imaging 38(9):1648–1658
Joshi P, Lele V (2013) Somatostatin receptor positron emission tomography/computed tomography (PET/CT) in the evaluation of opsoclonus-myoclonus ataxia syndrome. Indian J Nucl Med 28:108–111
Mayerhoefer ME, Ba-Ssalamah A, Weber M et al (2013) Gadoxetate-enhanced versus diffusion-weighted MRI for fused Ga-68-DOTANOC PET/MRI in patients with neuroendocrine tumours of the upper abdomen. Eur Radiol 23:1978–1985
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Bhagwant Rai Mittal
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institute ethics committee due to retrospective and observational nature of the study.
Ethical approval
Institute ethics committee approved the study.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, R., Vankadari, K., Mittal, B.R. et al. Diagnostic values of 68Ga-labelled DOTANOC PET/CT imaging in pediatric patients presenting with paraneoplastic opsoclonus myoclonus ataxia syndrome. Eur Radiol 31, 4587–4594 (2021). https://doi.org/10.1007/s00330-020-07587-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07587-x