Abstract
Purpose
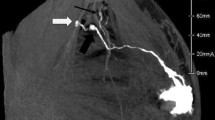
To investigate the clinical value of real-time three-dimensional contrast-enhanced ultrasound (3D-CEUS) in the detection of sentinel lymph nodes (SLNs) and drainage lymphatics in breast cancer patients.
Method
The prospective study was performed in women with pathology-confirmed T1/2 breast cancer between June 2016 and December 2017 who underwent sentinel lymph node biopsy and 3D-CEUS. The number, size, location, enhancement pattern of SLNs, and the lymphatic drainage patterns were reviewed. The routes, location of SLNs, and lymph channels (LCs) on the surface were marked. All patients underwent blue dye–guided sentinel lymph node biopsy (SLNB) finally.
Results
According to the postoperative pathology findings and the blue dye staining of the lymphatic drainage routes, there are six patterns of lymphatic drainage routes and the coincidence rate of the 3D-CEUS was 97.4%; the sensitivity, specificity, positive predictive value, negative predictive value, the LN detection rate, and the correct diagnosis rate of the 3D-CEUS were 75%, 93.0%, 81.8%, 89.9%, 95.3%, and 87.7%, respectively.
Conclusion
3D-CEUS is a new feasible and useful approach to detect the SLNs and LCs. 3D-CEUS can accurately localize the LCs and SLNs and estimate the presence of metastatic lymph nodes.
Key Points
• The three-dimensional contrast-enhanced ultrasound can detect the sentinel lymph nodes.
• The three-dimensional contrast-enhanced ultrasound can show the stereo direction of sentinel lymph nodes and lymph drainage routes.
• The three-dimensional contrast-enhanced ultrasound can accurately localize the LCs and SLNs and estimate the presence of metastatic lymph nodes.






Similar content being viewed by others
Abbreviations
- 2D-US:
-
Two-dimensional ultrasound
- 3D-CEUS:
-
Real-time three-dimensional contrast-enhanced ultrasound
- 3D-US:
-
Three-dimensional ultrasound
- ALN:
-
Axillary lymph node
- CEUS:
-
Contrast-enhanced ultrasound
- ICG:
-
Indocyanine green fluorescence
- LC:
-
Lymph channel
- LN:
-
Lymph node
- SLN:
-
Sentinel lymph node
- SLNB:
-
Sentinel lymph node biopsy
References
Morton DL, Wen DR, Wong JH et al (1992) Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 27(4):392–399
Nieweg OE, Tanis PJ, Kroon BB (2001) The definition of a sentinel node. Ann Surg Oncol 8(6):538–541
Giuliano AE, Ballman K, McCall L et al (2016) Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: long-term follow-up from the American College of Surgeons oncology group (Alliance) ACOSOG Z0011 randomized trial. Ann Surg 264(3):413–420
Giuliano AE, McCall L, Beitsch P et al (2010) Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons oncology group Z0011 randomized trial. Ann Surg 252(3):426–432 discussion 432–433
Gradishar WJ, Anderson BO, Balassanian R (2017) Breast cancer, version 1.2017 featured updates to the NCCN guidelines. J Natl Compr Cancer Netw 15(4):433–451
Veronesi U, Paganelli G, Viale G et al (2005) A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 349(6):546–553. https://doi.org/10.1056/NEJMoa012782
Canavese G, Gipponi M, Catturich A et al (2015) Sentinel lymph node mapping in early-stage breast cancer: technical issues and results with vital blue dye mapping and radioguided surgery. J Surg Oncol 74(1):61–68
Mcmasters KM, Tuttle TM, Carlson DJ et al (2000) Sentinel lymph node biopsy for breast cancer: a suitable alternative to routine axillary dissection in multi-institutional practice when optimal technique is used. J Clin Oncol 18(13):2560–2566
Motomura K, Inaji H, Komoike Y et al (2015) Combination technique is superior to dye alone in identification of the sentinel node in breast cancer patients. J Surg Oncol 76(2):95–99
Crossin JA, Johnson AC, Stewart PB, Turner WW Jr (1998) Gamma-probe-guided resection of the sentinel lymph node in breast cancer. Am Surg 64(7):666–668
Scherer K, StuderW FV, Bircher AJ (2006) Anaphylaxis to isosulfan blue and cross-reactivity to patent blue V: case report and review of the nomenclature of vital blue dyes. Ann Allergy Asthma Immunol 96(3):497–500. https://doi.org/10.1016/s1081-1206(10)60921-0
Fleissig A, Fallowfield LJ, Langridge CI et al (2005) Post-operative arm morbidity and quality of life. Results of the ALMANAC randomised trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res Treat 15(3):279–293. https://doi.org/10.1007/s10549-005-9025-7
Martin RC 2nd, Edwards MJ, Wong SL et al (2000) Practical guidelines for optimal gamma probe detection of sentinel lymph nodes in breast cancer: results of a multi-institutional study. Surgery 128(2):139–144
Hutteman M, Mieog JS, van der Vorst JR et al (2011) Randomized, double-blind comparison of indocyanine green with or without albumin premixing for near-infrared fluorescence imaging of sentinel lymph nodes in breast cancer patients. Breast Cancer Res Treat 127(1):163–170. https://doi.org/10.1007/s10549-011-1419-0
Chongwei C, Jinzuo Y, Haolong D et al (2013) Use of indocyanine green for detecting the sentinel lymph node in breast cancer patients: from preclinical evaluation to clinical validation. PLoS One 8(12):e83927. https://doi.org/10.1371/journal.pone.0083927
Murawa D, Hirche C, Dresel S, Hünerbein M (2010) Sentinel lymph node biopsy in breast cancer guided by indocyanine green fluorescence. Br J Surg 96(11):1289–1294. https://doi.org/10.1016/s1043-321x(10)79577-1
Kitai T, Inomoto T, Miwa M et al (2005) Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer 12(3):211–215. https://doi.org/10.2325/jbcs.12.211
Sever AR, Mills P, Jones SE et al (2011) Preoperative sentinel node identification with ultrasound using microbubbles in patients with breast cancer. AJR Am J Roentgenol 196(2):251. https://doi.org/10.2214/ajr.10.4865
Wang Y, ZhouW LC et al (2017) Variation of sentinel lymphatic channels (SLCs) and sentinel lymph nodes (SLNs) assessed by contrast-enhanced ultrasound (CEUS) in breast cancer patients. World J Surg Oncol 15(1):127. https://doi.org/10.1186/s12957-017-1195-3
Wang M, Zhou W, Zhao Y et al (2012) A novel finding of sentinel lymphatic channels in early stage breast cancer patients: which may influence detection rate and false-negative rate of sentinel lymph node biopsy. PLoS One 7(12):e51226
Campbell S, Lees C, Moscoso G et al (2005) Ultrasound antenatal diagnosis of cleft palate by a new technique: the 3D “reverse face” view. Ultrasound Obstet Gynecol 25(1):12–18. https://doi.org/10.1002/uog.1819
Platt LD, Devore GR, Pretorius DH (2006) Improving cleft palate/ cleft lip antenatal diagnosis by 3-dimensional sonography. J Ultrasound Med 25(11):1423–1430. https://doi.org/10.7863/jum.2006.25.11.1423
Martínez Ten P, Pérez Pedregosa J, Santacruz B, Adiego B, Barrón E, Sepúlveda W (2010) Three-dimensional ultrasound diagnosis of cleft palate: ‘reverse face’, ‘flipped face’ or ‘oblique face’–which method is best? Ultrasound Obstet Gynecol 33(4):399–406. https://doi.org/10.1002/uog.6257
Numata K, Morimoto M, Nozaki A et al (2010) Differentiation of focal liver lesions using three-dimensional ultrasonography: retrospective and prospective studies. World J Gastroenterol 16(17):2109–2119. https://doi.org/10.3748/wjg.v16.i17.2109
Wang Y, Xiang J, Ding J (2016) Clinical value of dynamic 3- dimensional contrast-enhanced ultrasound imaging for the assessment of hepatocellular carcinoma ablation. Clin Imaging 40(3):402–406
Dietrich CF (2002) 3D real time contrast enhanced ultrasonography: a new technique. Rofo 174:160–163
Ohto M, Kato H, Tsujii H et al (2005) Vascular flow patterns of hepatic tumors in contrast-enhanced 3-dimensional fusion ultrasonography using plane shift and opacity control modes. J Ultrasound Med 24:49–57
Yukisawa S, Ohto M, Masuya Y et al (2007) Contrast enhanced three-dimensional fusion sonography of small liver metastases with pathologic correlation. J Clin Ultrasound 35:1–8
Dong FJ, Xu JF, Dong D et al (2016) 3D analysis is superior to 2D analysis for contrast-enhanced ultrasound in revealing vascularity in focal liver lesions —a retrospective analysis of 83 cases. Ultrasonics 70:221–226. https://doi.org/10.1016/j.ultras.2016.05.007
Kupesic S, Plavsic BM (2007) 2D and 3D hysterosalpingocontrast- sonography in the assessment of uterine cavity and tubal patency. Eur J Obstet Gynecol Reprod Biol 133(1):64–69. https://doi.org/10.1016/j.ejogrb.2006.10.010
Xie F, ZhangD CL et al (2015) Intradermalmicrobubbles and contrast-enhanced ultrasound (CEUS) is a feasible approach for sentinel lymph node identification in early-stage breast cancer. World J Surg Oncol 13(1):319–326
Zhao J, Zhang J, Zhu QL et al (2018) The value of contrastenhanced ultrasound for sentinel lymph node identification and characterisation in pre-operative breast cancer patients: a prospective study. Eur Radiol 28(4):1654–1661. https://doi.org/10.1007/s00330-017-5089-0
Yang WT, Goldberg BB (2011) Microbubble contrast-enhanced ultrasound for sentinel lymph node detection: ready for prime time? AJR Am J Roentgenol 196(2):249–250. https://doi.org/10.2214/ajr.10.5707
Bude RO (2004) Does contrast-enhanced US have potential for sentinel lymph node detection? Radiology 230(3):603–604. https://doi.org/10.1148/radiol.2303031683
YuM LQ, Song HP et al (2010) Clinical application of contrastenhanced ultrasonography in diagnosis of superficial lymphadenopathy. J Ultrasound Med 29(5):735. https://doi.org/10.7863/jum.2010.29.5.735
Cui XW, Ignee A, Nielsen MB et al (2013) Contrast enhanced ultrasound of sentinel lymph nodes. J Ultrason 13(52):73–81. https://doi.org/10.15557/jou.2013.0006
Serra C, Pallotti F, Bortolotti M et al (2016) A new reliable method for evaluating gallbladder dynamics: the 3-dimensional sonographic examination. J Ultrasound Med 35(2):297
Luo W, Numata K, Morimoto M et al (2009) Three-dimensional contrast-enhanced sonography of vascular patterns of focal liver tumors: pilot study of visualization methods. AJR Am J Roentgenol 192:165–173
Xu HX, Lu MD, Xie XH et al (2009) Three-dimensional contrastenhanced ultrasound of the liver: experience of 92 cases. Ultrasonics 49:377–385
Luo W, Numata K, Morimoto M et al (2010) Differentiation of focal liver lesions using three-dimensional ultrasonography: retrospective and prospective studies. World J Gastroenterol 16:2109–1942
Cox K, Sever A, Jones S et al (2013) Validation of a technique using microbubbles and contrast enhanced ultrasound (CEUS) to biopsy sentinel lymph nodes (SLN) in pre-operative breast cancer patients with a normal grey-scale axillary ultrasound. Eur J Surg Oncol 39(7):760–765. https://doi.org/10.1016/j.ejso.2013.03.026
Funding
This study has received funding by the Department of Science and Technology of Sichuan Provincial.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Man Lu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ziyue Hu and Man Lu contributed to the work equally and should be regarded as co-first authors.
Rights and permissions
About this article
Cite this article
Hu, Z., Cheng, X., Li, J. et al. Preliminary study of real-time three-dimensional contrast-enhanced ultrasound of sentinel lymph nodes in breast cancer. Eur Radiol 30, 1426–1435 (2020). https://doi.org/10.1007/s00330-019-06494-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06494-0