Abstract
Objectives
To determine the relationship between the number of administrations of various gadolinium-based contrast agents (GBCAs) and increased T1 signal intensity in the globus pallidus (GP) and dentate nucleus (DN).
Methods
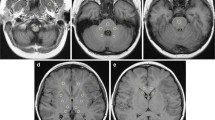
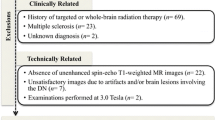
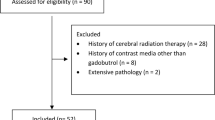
This retrospective study included 122 patients who underwent double-dose GBCA-enhanced magnetic resonance imaging. Two radiologists calculated GP-to-thalamus (TH) signal intensity ratio, DN-to-pons signal intensity ratio and relative change (Rchange) between the baseline and final examinations. Interobserver agreement was evaluated. The relationships between Rchange and several factors, including number of each GBCA administrations, were analysed using a generalized additive model.
Results
Six patients (4.9%) received linear GBCAs (mean 20.8 number of administration; range 15–30), 44 patients (36.1%) received macrocyclic GBCAs (mean 26.1; range 14–51) and 72 patients (59.0%) received both types of GBCAs (mean 31.5; range 12–65). Interobserver agreement was almost perfect (0.99; 95% CI: 0.99–0.99). Rchange (DN:pons) was associated with gadodiamide (p = 0.006) and gadopentetate dimeglumine (p < 0.001), but not with other GBCAs. Rchange (GP:TH) was not associated with GBCA administration.
Conclusions
Previous administration of linear agents gadoiamide and gadopentetate dimeglumine is associated with increased T1 signal intensity in the DN, whereas macrocyclic GBCAs do not show an association.
Key points
• Certain linear GBCAs are associated with T1 signal change in the dentate nucleus.
• The signal change is related to the administration number of certain linear GBCAs.
• Difference in signal change may reflect differences in stability of agents.




Similar content being viewed by others
Abbreviations
- BBB:
-
Blood-brain barrier
- CSF:
-
Cerebrospinal fluid
- DN:
-
Dentate nucleus
- eGFR:
-
Estimated glomerular infiltration rate
- GAM:
-
Generalized additive model
- GBCA:
-
Gadolinium-based contrast agent
- GP:
-
Globus pallidus
- MRI:
-
Magnetic resonance imaging
- NSF:
-
Nephrogenic systemic fibrosis
- Rchange :
-
Relative change
- ROI:
-
Region of interest
- TH:
-
Thalamus
References
Hao D, Ai T, Goerner F, Hu X, Runge VM, Tweedle M (2012) MRI contrast agents: basic chemistry and safety. J Magn Reson Imaging 36:1060–1071
Ersoy H, Rybicki FJ (2007) Biochemical safety profiles of gadolinium-based extracellular contrast agents and nephrogenic systemic fibrosis. J Magn Reson Imaging 26:1190–1197
Oksendal AN, Hals PA (1993) Biodistribution and toxicity of MR imaging contrast media. J Magn Reson Imaging 3:157–165
Grobner T (2006) Gadolinium--a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant 21:1104–1108
Kanal E, Tweedle MF (2015) Residual or retained gadolinium: practical implications for radiologists and our patients. Radiology 275:630–634
Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D (2014) High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 270:834–841
McDonald RJ, McDonald JS, Kallmes DF, Jentoft ME, Murray DL, Thielen KR et al (2015) Intracranial gadolinium deposition after contrast-enhanced MR imaging. Radiology 275:772–782
Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J et al (2015) Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology 276:228–232
Errante Y, Cirimele V, Mallio CA, Di Lazzaro V, Zobel BB, Quattrocchi CC (2014) Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Investig Radiol 49:685–690
Kanda T, Osawa M, Oba H, Toyoda K, Kotoku J, Haruyama T et al (2015) High signal intensity in dentate nucleus on unenhanced T1-weighted MR images: association with linear versus macrocyclic gadolinium chelate administration. Radiology 275:803–809
Quattrocchi CC, Mallio CA, Errante Y, Cirimele V, Carideo L, Ax A et al (2015) Gadodiamide and dentate nucleus T1 hyperintensity in patients with meningioma evaluated by multiple follow-up contrast-enhanced magnetic resonance examinations with no systemic interval therapy. Investig Radiol 50:470–472
Radbruch A, Weberling LD, Kieslich PJ, Eidel O, Burth S, Kickingereder P et al (2015) Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 275:783–791
Cao Y, Huang DQ, Shih G, Prince MR (2016) Signal change in the dentate nucleus on T1-weighted MR images after multiple administrations of gadopentetate dimeglumine versus gadobutrol. AJR Am J Roentgenol 206:414–419
Radbruch A, Weberling LD, Kieslich PJ, Hepp J, Kickingereder P, Wick W et al (2015) High-signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted images: evaluation of the macrocyclic gadolinium-based contrast agent gadobutrol. Investig Radiol 50:805–810
Adin ME, Kleinberg L, Vaidya D, Zan E, Mirbagheri S, Yousem DM (2015) Hyperintense dentate nuclei on T1-weighted MRI: relation to repeat gadolinium administration. AJNR Am J Neuroradiol 36:1859–1865
Roberts DR, Holden KR (2016) Progressive increase of T1 signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images in the pediatric brain exposed to multiple doses of gadolinium contrast. Brain Dev 38:331–336
Weberling LD, Kieslich PJ, Kickingereder P, Wick W, Bendszus M, Schlemmer HP et al (2015) Increased signal intensity in the dentate nucleus on unenhanced T1-weighted images after gadobenate dimeglumine administration. Investig Radiol 50:743–748
Stojanov DA, Aracki-Trenkic A, Vojinovic S, Benedeto-Stojanov D, Ljubisavljevic S (2016) Increasing signal intensity within the dentate nucleus and globus pallidus on unenhanced T1W magnetic resonance images in patients with relapsing-remitting multiple sclerosis: correlation with cumulative dose of a macrocyclic gadolinium-based contrast agent, gadobutrol. Eur Radiol 26:807–815
Murata N, Gonzalez-Cuyar LF, Murata K, Fligner C, Dills R, Hippe D et al (2016) Macrocyclic and other non–group 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue: preliminary results from 9 patients with normal renal function. Investig Radiol 51:447–453
Ramalho J, Castillo M, AlObaidy M, Nunes RH, Ramalho M, Dale BM et al (2015) High signal intensity in globus pallidus and dentate nucleus on unenhanced T1-weighted MR images: evaluation of two linear gadolinium-based contrast agents. Radiology 276:836–844
Jost G, Lenhard DC, Sieber MA, Lohrke J, Frenzel T, Pietsch H (2016) Signal increase on unenhanced T1-weighted images in the rat brain after repeated, extended doses of gadolinium-based contrast agents: comparison of linear and macrocyclic agents. Investig Radiol 51:83–89
Subedi KS, Takahashi T, Yamano T, Saitoh J, Nishimura K, Suzuki Y et al (2013) Usefulness of double dose contrast-enhanced magnetic resonance imaging for clear delineation of gross tumor volume in stereotactic radiotherapy treatment planning of metastatic brain tumors: a dose comparison study. J Radiat Res 54:135–139
Kim ES, Chang JH, Choi HS, Kim J, Lee SK (2010) Diagnostic yield of double-dose gadobutrol in the detection of brain metastasis: intraindividual comparison with double-dose gadopentetate dimeglumine. AJNR Am J Neuroradiol 31:1055–1058
Ahn SJ, Chung T-S, Chang J-H, Lee S-K (2014) The added value of double dose gadolinium enhanced 3D T2 fluid-attenuated inversion recovery for evaluating small brain metastases. Yonsei Med J 55:1231–1237
Lin LI (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45:255–268
Hastie T, Tibshirani R (1995) Generalized additive models for medical research. Stat Methods Med Res 4:187–196
Schmitt-Willich H (2007) Stability of linear and macrocyclic gadolinium based contrast agents. Br J Radiol 80:581–582, author reply 584-585
Idee JM, Port M, Raynal I, Schaefer M, Le Greneur S, Corot C (2006) Clinical and biological consequences of transmetallation induced by contrast agents for magnetic resonance imaging: a review. Fundam Clin Pharmacol 20:563–576
Fretellier N, Idee JM, Dencausse A, Karroum O, Guerret S, Poveda N et al (2011) Comparative in vivo dissociation of gadolinium chelates in renally impaired rats: a relaxometry study. Investig Radiol 46:292–300
Edwards BJ, Laumann AE, Nardone B, Miller FH, Restaino J, Raisch DW et al (2014) Advancing pharmacovigilance through academic-legal collaboration: the case of gadolinium-based contrast agents and nephrogenic systemic fibrosis-a Research on Adverse Drug Events and Reports (RADAR) report. Br J Radiol 87:20140307
Frenzel T, Lengsfeld P, Schirmer H, Hutter J, Weinmann HJ (2008) Stability of gadolinium-based magnetic resonance imaging contrast agents in human serum at 37 degrees C. Investig Radiol 43:817–828
Cacheris WP, Quay SC, Rocklage SM (1990) The relationship between thermodynamics and the toxicity of gadolinium complexes. Magn Reson Imaging 8:467–481
Chang CA (1993) Magnetic resonance imaging contrast agents. Design and physicochemical properties of gadodiamide. Investig Radiol 28:S21–S27
Robert P, Lehericy S, Grand S, Violas X, Fretellier N, Idee JM et al (2015) T1-weighted hypersignal in the deep cerebellar nuclei after repeated administrations of gadolinium-based contrast agents in healthy rats: difference between linear and macrocyclic agents. Investig Radiol 50:473–480
Qin DX, Zheng R, Tang J, Li JX, Hu YH (1990) Influence of radiation on the blood-brain barrier and optimum time of chemotherapy. Int J Radiat Oncol Biol Phys 19:1507–1510
van Vulpen M, Kal HB, Taphoorn MJ, El-Sharouni SY (2002) Changes in blood-brain barrier permeability induced by radiotherapy: implications for timing of chemotherapy? (Review). Oncol Rep 9:683–688
Yuan H, Gaber MW, Boyd K, Wilson CM, Kiani MF, Merchant TE (2006) Effects of fractionated radiation on the brain vasculature in a murine model: blood-brain barrier permeability, astrocyte proliferation, and ultrastructural changes. Int J Radiat Oncol Biol Phys 66:860–866
Mattos DM, Gomes ML, Freitas RS, Boasquevisque EM, Cardoso VN, Paula EF et al (2000) The effect of vincristine on the biodistribution of technetium-99m DTPA, GHA, and DMSA in Balb/c female mice. J Nucl Med Technol 28:271–274
Frey KW, Hoer G (1965) Effect of thyreovalun, an antithyroid drug of plant origin, on the thyroid radioiodine (I-131) incorporation test. Arztl Forsch 19:155–157
Kennedy JM, Van Riji AM (1998) Effects of surgery on the pharmacokinetic parameters of drugs. Clin Pharmacokinet 35:293–312
Ramalho J, Semelka RC, AlObaidy M, Ramalho M, Nunes RH, Castillo M (2016) Signal intensity change on unenhanced T1-weighted images in dentate nucleus following gadobenate dimeglumine in patients with and without previous multiple administrations of gadodiamide. Eur Radiol 26:4080–4088
Magnotta VA, Friedman L, First B (2006) Measurement of signal-to-noise and contrast-to-noise in the fBIRN multicenter imaging study. J Digit Imaging 19:140–147
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Seung-Koo Lee.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
One of the authors has significant statistical expertise.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Methodology
Retrospective, diagnostic or prognostic study, performed at one institution.
Rights and permissions
About this article
Cite this article
Bae, S., Lee, HJ., Han, K. et al. Gadolinium deposition in the brain: association with various GBCAs using a generalized additive model. Eur Radiol 27, 3353–3361 (2017). https://doi.org/10.1007/s00330-016-4724-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4724-5