Abstract
Objectives
To investigate the influence of variations in resting pressure (precompression) on thyroid ultrasound supersonic shear wave elastography (SWE).
Methods
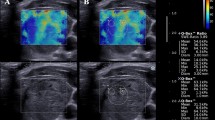
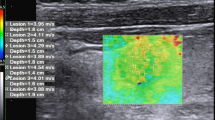
Thirty-five normal thyroid glands (Norm), 55 benign hyperplastic nodules (BHN), and 17 papillary thyroid cancers (PTC) in 96 subjects underwent thyroid SWE. Four precompression levels were applied manually by the operator, ranging from A (baseline, 0 % strain) to D (high, 22–30 % strain). SWE results at each precompression level were compared using ANOVA tests with P < 0.05 indicating significance.
Results
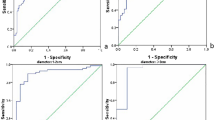
SWE indices were highest in PTC, followed by BHN and Norm at each precompression level (P < 0.05). All tissue types showed successive increases in SWE results as precompression increased, although the rate was higher for PTC than BHN and Norm (Ps < 0.05). SWE values (kPa) of Norm, BHN, and PTC at baseline precompression (A) were 10.3 ± 3.3, 17.7 ± 7.6, and 22.2 ± 11.9 compared with 21.1 ± 4.2, 42.3 ± 16.0, and 97.6 ± 46.8 at high precompression (D). SWE index differences between precompression levels A and D were 10.8 kPa for Norm, 24.6 kPa for BHN, and 75.4 kPa for PTC.
Conclusion
PTCs show greater SWE stiffening than BHN as precompression rises. Precompression effects on thyroid nodules are not negligible and may account for wide discrepancies in published SWE discriminatory performance results for thyroid malignancy.
Key Points
• Increases in resting pressure (precompression) applied by the operator increases thyroid stiffness.
• Papillary cancers show greater increases in stiffness (strain hardening) than benign nodules.
• Precompression may affect the diagnostic performance of shearwave elastography for thyroid malignancy.



Similar content being viewed by others
Abbreviations
- SWE:
-
Shear wave elastography
- US:
-
Ultrasound
- USE:
-
Ultrasound elastography
- PTC:
-
Papillary thyroid carcinoma
- BHN:
-
Benign hyperplastic nodule
- Norm:
-
Normal thyroid tissue
- kPa:
-
Kilopascals
- ROIs:
-
Regions of interest
References
Wong KT, Ahuja AT (2005) Ultrasound of thyroid cancer. Cancer Imaging 5:157–166
Cosgrove D, Piscaglia F, Bamber J et al (2013) EFSUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography. Part 2: Clinical Applications. Ultraschall Med Eur J Ultrasound 34:238–253
Bamber J, Cosgrove D, Dietrich C et al (2013) EFSUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med Eur J Ultrasound 34:169–184
DeWall RJ, Varghese T, Kliewer MA, Harter JM, Hartenbach EM (2010) Compression-dependent viscoelastic behavior of human cervix tissue. Ultrason Imaging 32:214–228
Barr RG, Zhang Z (2012) Effects of precompression on elasticity imaging of the breast: development of a clinically useful semiquantitative method of precompression assessment. J Ultrasound Med 31:895–902
Krouskop TA, Wheeler TM, Kallel F, Garra BS (1998) Elastic moduli of breast and prostate tissues under compression. Ultrason Imaging 20:260–274
Yeh WC, Li PC, Jeng YM et al (2002) Elastic modulus measurements of human liver and correlation with pathology. Ultrasound Med Biol 28:467–474
Lyshchik A, Higashi T, Asato R et al (2005) Elastic moduli of thyroid tissues under compression. Ultrason Imaging 27:101–110
Veer V, Puttagunta S (2014) The role of elastography in evaluating thyroid nodules: a literature review and meta-analysis. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-014-3155-7
Lin P, Chen M, Liu B, Wang S, Li X (2014) Diagnostic performance of shear wave elastography in the identification of malignant thyroid nodules: a meta-analysis. Eur Radiol 24:2729–2738
Bhatia KSS, Lee YYP, Yuen EHY, Ahuja AT (2013) Ultrasound elastography in the head and neck. Part II. Accuracy for malignancy. Cancer Imaging 13:260–276
Kwak JY, Kim E-K (2014) Ultrasound elastography for thyroid nodules: recent advances. Ultrasonography 33:75–82
Sebag F, Vaillant-Lombard J, Berbis J et al (2010) Shear Wave Elastography: A New Ultrasound Imaging Mode for the Differential Diagnosis of Benign and Malignant Thyroid Nodules. Journal of Clinical Endocrinology &. Metabolism 95:5281–5288
Veyrieres J-B, Albarel F, Lombard JV et al (2012) A threshold value in Shear Wave elastography to rule out malignant thyroid nodules: a reality? Eur J Radiol 81:3965–3972
Kim H, Kim J-A, Son EJ, Youk JH (2013) Quantitative assessment of shear-wave ultrasound elastography in thyroid nodules: diagnostic performance for predicting malignancy. Eur Radiol 23:2532–2537
Liu B, Liang J, Zheng Y et al (2014) Two-dimensional shear wave elastography as promising diagnostic tool for predicting malignant thyroid nodules: a prospective single-centre experience. Eur Radiol. doi:10.1007/s00330-014-3455-8
Szczepanek-Parulska E, Woliński K, Stangierski A (2013) Comparison of diagnostic value of conventional ultrasonography and shear wave elastography in the prediction of thyroid lesions malignancy. PLoS One. doi:10.1371/journal.pone
Bhatia KS, Tong CS, Cho CC, Yuen EH, Lee YY, Ahuja AT (2012) Shear wave elastography of thyroid nodules in routine clinical practice: preliminary observations and utility for detecting malignancy. Eur Radiol 22:2397–2406
Liu B-X, Xie X-Y, Liang J-Y et al (2014) Shear wave elastography versus real-time elastography on evaluation thyroid nodules: A preliminary study. Eur J Radiol 83:1135–1143
Szczepanek-Parulska E, Woliński K, Stangierski A, Gurgul E, Ruchała M (2014) Biochemical and ultrasonographic parameters influencing thyroid nodules elasticity. Endocrine. doi:10.1007/s12020-014-0197-y
Wolinski K, Stangierski A, Szczepanek-Parulska E, Gurgul E, Ruchala M (2015) Dependence of thyroid sonographic markers of malignancy and its influence on the diagnostic value of sonographic findings. Biomed Res Int 2015:693404
Syversveen T, Midtvedt K, Berstad AE, Brabrand K, Strøm EH, Abildgaard A (2012) Tissue elasticity estimated by acoustic radiation force impulse quantification depends on the applied transducer force: an experimental study in kidney transplant patients. Eur Radiol 22:2130–2137
Acknowledgments
The scientific guarantor of this publication is Kunwar Bhatia. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by Research Grants Council of the Hong Kong Special Administrative Region, China (grant Chinese University of Hong Kong; project no. 460412). No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Approval from the institutional animal care committee was not required because animal subject was not used in this research. Study subjects or cohorts have not been previously reported. Methodology: prospective, diagnostic or prognostic study, multicenter study / performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lam, A.C.L., Pang, S.W.A., Ahuja, A.T. et al. The influence of precompression on elasticity of thyroid nodules estimated by ultrasound shear wave elastography. Eur Radiol 26, 2845–2852 (2016). https://doi.org/10.1007/s00330-015-4108-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4108-2