Abstract
The popularity of esthetic medicine is growing every year, also among patients with autoimmune inflammatory rheumatic diseases (AIRD). The objective of this study was to evaluate the safety of esthetic medicine (AM) procedures in patients with AIRD. A semi-structured, anonymous questionnaire regarding rheumatic and concomitant diseases and AM procedures was distributed among adult patients hospitalized in the rheumatology department or attending outpatient clinic in the National Institute of Geriatrics, Rheumatology, and Rehabilitation, Warsaw. The main outcome was the occurrence of an adverse event. A number of 512 patients took part in the survey and 15 were excluded (AM procedure preceded the diagnosis of AIRD). The study group consisted of 497 patients, of whom 47 had undergone AM procedures. The procedures performed included: tattooing (22 patients), piercing (16 patients), hyaluronic acid (7 patients), botulinum toxin (5 patients) injections, laser procedures (6 patients), plastic surgery (4 patients), mesotherapy (3 patients) and others. The vast majority of patients had these performed during remission or low disease activity. 70.2% of patients received treatment with disease-modifying antirheumatic drugs (DMARDs) during the AM procedure, with TNF-alfa inhibitors being the most common (63.6%). Adverse events occurred in 15% of patients. All were mild and transient site reactions. Most patients would like to repeat the AM procedure in the future. The use of esthetic medicine procedures in patients with AIRD, including those treated with biologic DMARDs, was associated with a risk of mild site reactions. Most of the patients expressed satisfaction with the results of the AM procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of new treatment paradigms for rheumatic diseases in recent years resulted in improvements in patients’ quality of life. Rheumatologists are increasingly dealing with questions about the possibility of using esthetic medicine (AM), plastic surgery, or tattooing. Both men and women go for, more or less, invasive methods to alter their appearance, resulting in the growing popularity of esthetic medicine every year. Unfortunately, these interventions can cause adverse events, even in the hands of experienced professionals. Appropriate selection of patients for the procedure and considering their medical history are extremely important. Some data indicate that the risk of adverse events increases in patients with inflammatory conditions of the skin (psoriasis, rosacea, and skin infections), active connective tissue diseases with skin involvement, or immunosuppressive treatment [1], but data on the safety of patients with autoimmune inflammatory rheumatic diseases (AIRD) are limited and contradictory.
The purpose of this study was to gather information on the performance of esthetic medicine, plastic surgery, and tattooing procedures in patients with AIRD and to assess the incidence of complications following these procedures.
Materials and methods
This unvalidated survey was drafted by two clinician rheumatologists and revised by a third clinician rheumatologist who decided in any disagreement. The study received ethical approval from the National Institute of Geriatrics, Rheumatology, and Rehabilitation Ethics Committee (KBT-5/10/2022, 08.11.2022). All study procedures were conducted in accordance with the Declaration of Helsinki.
A semi-structured, anonymous questionnaire consisted of 19 closed and open questions regarding demographics, rheumatic and concomitant diseases, and AM procedure (Appendix 1). The main outcome was the occurrence of an adverse event.
We distributed paper booklets among adult patients hospitalized in the Department of Connective Tissue Diseases or attending outpatient clinic—Biological Therapy Center in the National Institute of Geriatrics, Rheumatology, and Rehabilitation, Warsaw, between April 2018 and December 2019. Participation in the survey was voluntary, followed by written consent. Patients completed it personally during the visit. Handwritten answers were collected and entered into database by the authors between April and August 2020.
The inclusion criterium was a diagnosis of AIRD and the exclusion criterium was a history of AM procedure before the diagnosis of AIRD.
GraphPad Prism 8.4.1 has been used to conduct statistical analysis. Numerical data distribution was analyzed using the Shapiro–Wilk test. The Mann–Whitney test, Kruskal–Wallis test, or one-way ANOVA were used for inter-group comparisons. The frequency of categorical data was analyzed using Fisher’s exact test. Statistical significance was set at p < 0.05.
Results
A number of 512 patients took part in the survey and 15 were excluded (AM procedure preceded the diagnosis of AIRD). The study group consisted of 497 patients, of whom 47 had undergone AM procedures (group 2). In group 2, women (n = 39; 83%) outnumbered men (n = 8; 17%) and the average age of the patient was 36.8 ± 9 years (min. 20, max. 56 years). Among the 450 patients who had never had AM procedures (group 1), there were 254 women (56%) and 196 men (44%) and patients were older (the average age was 48 ± 14 years, min. 18, max. 82 years).
Demographic data and the distribution of diagnoses are shown in Table 1. There were no statistically significant differences regarding place of residence and education between the groups.
AM procedures and treatment reported within group 2 are shown in Tables 2 and 3. Only 4 patients had their disease-modifying antirheumatic drug (DMARD) discontinued temporarily due to a planned AM procedure.
A number of 21 subjects (44.7%) consulted a physician before the procedure, including 14 patients consulting a rheumatologist. Recommendations against the AM procedure were reported by 4 patients (9%) The risk associated with AM procedure was discussed with 27 patients (63%).
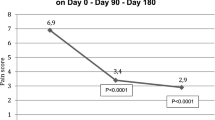
Since disease-specific activity scores at the time of the AM procedure were not available, patients were asked to rate disease activity subjectively on a five-point scale. The largest group of subjects underwent AM procedure while remission or mild disease activity (n = 39; 66%). Moderate activity was indicated by 12 patients (25.5%) and high activity by 4 patients (8.5%).
Side effects after a procedure affected 7 patients (15%) and included swelling, pain, redness, and bruising. All events were mild and transient and dissipated within 2 weeks; only in 3 cases they required medical consultation.
In group 2, most patients (57.4%, n = 27) would like to repeat the AM procedure in the future. In comparison, in group 1, only 37 patients (8%) expressed a desire to undergo such a procedure.
Discussion
There is a paucity of literature on the safety of AM procedures in patients with rheumatic conditions. However, several aspects concerning this group of patients should be considered.
Wound healing and blood coagulability
According to the Kluger guidelines (2018), rheumatic diseases such as systemic lupus erythematosus or scleroderma are not a contraindication for tattooing. However, the procedure should not be performed when a disease is active/unstable or in an acute stage of flaring, because skin healing may be delayed, resulting in poor esthetic effect [2]. Chin et al. in their case series reported two of the main complications that can occur in patients with severe connective tissue diseases: delayed donor site wound healing, and delayed hematoma formation [3].
Alternatively, some authors suggested that dermal fillers are not contraindicated in patients in whom wound healing is normal, even though they may have an underlying systemic disease [4, 5]. In addition, Lemperle et al. have not found immunosuppression to delay wound healing, because fibroblasts need an approximately tenfold higher concentration of immunosuppressive drugs to be affected than do immunocytes [4].
Infections
Immunosuppressive treatment may involve a higher risk of complications such as increased fatigue/diminished stamina during the tattoo session, and increased risk of local or systemic infection [2].
There have been few studies evaluating perioperative clinical features and complications after elective orthopedic surgery in these patients, including the risk of surgical site infection. These studies demonstrated a significant association between early infectious complications and impaired wound healing following orthopedic surgery and treatment with TNF-alfa inhibitors in patients with rheumatoid arthritis [6,7,8]. It is known that patients with AIRD have been shown to be at higher risk for the development of surgical complications. The highest risk is in those with multiple organ dysfunction or using long-term steroids and immunosuppressive drugs [9]. In plastic surgery, the recommended time of biologic therapy cessation varies between 3 and 5 half-lives of the drug in the patients of low risk, but recent orthopedic recommendations allow to plan surgery after the end of the dose interval (1 to 5 half-lives, respectively) [8, 10].
Site reactions
Patients with a history of AIRD or receiving immunosuppression should avoid fillers containing copolymers of hydroxy-ethyl-methacrylate (HEMA) and ethyl-methacrylate (EMA), which are non-biodegradable and may cause severe granulomatous reactions [11]. It seems that the most appropriate dermal fillers for such patients are quickly biodegradable or re-absorbable agents [12]. The safety of fillers not approved by medicine agencies has been undermined [12]. A recent study by Koren et al. points to the high level of safety of esthetic treatment with non-permanent fillers in patients with inflammatory rheumatic diseases [13]. Furthermore, two reviews state that patients with autoimmune conditions may be safely treated with a variety of fillers [14, 15]. Cutaneous complications after tattooing occurred in 8.7% patients with psoriasis, with Koebner sign being the most common. No adverse events were observed in patients receiving biologic therapy [16].
New autoimmune entity development
While some studies have indicated a potential link between esthetic procedures and autoimmune diseases involving the injection of fillers, breast implants, or tattoo ink [4, 5, 17,18,19,20,21,22,23], others showed that there was no evidence of an association between AM procedures and AIRD [24]. Controlled epidemiological studies have not shown an actual link between silicone and systemic autoimmune diseases [25,26,27,28].
Hence, some authors permit the use of fillers in patients with systemic lupus erythematosus, rheumatoid arthritis, dermatomyositis/polymyositis, scleroderma, Sjögren syndrome, and Raynaud syndrome [4, 5, 10].
Adverse events may be delayed and may occur years after AM procedure [12].
Exacerbation of rheumatic disease
According to the American Society for Dermatologic Surgery recommendations, dermal fillers are not recommended for patients with lupus or other connective tissue disorders. Data indicate the risk of cross-reactivity of anti-dsDNA antibodies with collagen; hence, collagen-based fillers should not be used in patients with systemic lupus erythematosus [29]. No evidence was found of sclerosis reactivation preceded by hyaluronic acid filling in cases of stable localized scleroderma [30]. Tattooing in psoriasis resulted in exacerbation in 1.3% of patients [16]
It is worth mentioning that withholding drugs before AM procedure has the potential to produce a risk of exacerbation.
Drug interactions
Special care should be taken when using botulinum toxin (BTX) in patients taking immunosuppressive drugs [31, 32]. It should be avoided in patients treated with chloroquine, hydroxychloroquine, and cyclosporine [33].
Summary
To date, the risk of adverse events associated with AM procedures in patients with AIRD was not estimated. There are studies regarding specific procedures in specific diseases (like tattooing in psoriasis or dermal fillers in scleroderma) [16, 30]. Systematic reviews are focused on procedures (like breast implants or dermal fillers) [34, 35]. A systematic review investigating adverse events of injectable fillers showed that events with poor prognosis are very rare, and the evidence certainty on the topic is low [34]. Further investigations in the field of AM and AIRD are needed. Thus, we recommend individual consulting before AM procedure with the rheumatologist to discuss the topics mentioned in Table 4.
Limitations
The number of patients in group 2 is relatively small, making it difficult to draw definite conclusions. Another important limitation lies in the fact that the information is based on patients’ reporting, not medical history. Rare and remote time adverse events may require that large cohort studies would be able to show potential correlation.
The strength of this survey is that it is the first such paper (after the PubMed literature review) that has attempted to evaluate the safety of AM procedures in patients treated with biologics.
Conclusion
In our study, the use of esthetic medicine procedures in patients with AIRD, including those treated with bDMARDs, was associated with a risk of mild site reactions. Most of the patients expressed satisfaction with the results of the AM procedure and they would like to repeat the procedure in the future. AM procedure timing should be planned during remission or low disease activity. Patients undergoing immunosuppressive treatment need special attention to avoid wound infections.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
De Boulle K, Heydenrych I (2015) Patient factors influencing dermal filler complications: prevention, assessment, and treatment. Clin Cosmet Investig Dermatol 8:205. https://doi.org/10.2147/CCID.S80446
Kluger N, De Cuyper C (2018) A practical guide about tattooing in patients with chronic skin disorders and other medical conditions. Am J Clin Dermatol 19(2):167–180
Chin KY, Chalmers CR, Bryson AV et al (2013) Breast reconstruction in the high risk patient with systemic connective tissue disease: a case series. J Plast Reconstr Aesthet Surg 66(1):61–66
Lemperle G, Rullan PP, Gautier-Hazan N (2006) Avoiding and treating dermal filler complications. Plast Reconstr Surg Suppl 118:92S-107S
Lafaille P, Benedetto A (2010) Fillers: contraindications, side effects and precautions. J Cutan Aesth Surg 3:16–19
den Broeder AA, Creemers MC, Fransen J et al (2007) Risk factors for surgical site infections and other complications in elective surgery in patients with rheumatoid arthritis with special attention for anti-tumor necrosis factor: a large retrospective study. J Rheumatol 34(4):689–695
Kawakami K, Ikari K, Kawamura K et al (2009) Complications and features after joint surgery in rheumatoid arthritis patients treated with tumour necrosis factor-α blockers: perioperative interruption of tumour necrosis factor-α blockers decreases complications? Rheumatology 49(2):341–347
Goodman SM, Springer BD, Chen AF et al (2022) 2022 American College of Rheumatology/American Association of Hip and Knee Surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. Arthritis Care Res 74(9):1399–1408. https://doi.org/10.1002/acr.24893
Takahashi T, De-La-Garza L (1995) Risk factors for operative morbidity in patients with systemic lupus erythematosus: an analysis of 68 surgical procedures. Am Surgeon 61:260–264
Tsai DM, Borah GL (2015) Implications of rheumatic disease and biological response-modifying agents in plastic surgery. Plast Reconstr Surg 136(6):1327–1336. https://doi.org/10.1097/PRS.0000000000001792
Sachdev M, Anantheswar YN, Ashok BC et al (2010) Facial granulomas secondary to injection of semi-permanent cosmetic dermal filler containing acrylic hydrogel particles. J Cutan Aesthet Surg 3(3):162
Owczarczyk-Saczonek A, Zdanowska N, Wygonowska E et al (2021) The immunogenicity of hyaluronic fillers and its consequences. Clin Cosmet Investig Dermatol 16(14):921–934. https://doi.org/10.2147/CCID.S316352
Koren A, Sarbagil-Maman H, Litinsky I et al (2022) Dermal filler injections in patients with autoimmune and inflammatory rheumatic diseases—the patients’ perspective. Dermatol Surg 48(1):82–86. https://doi.org/10.1097/DSS.0000000000002888
Creadore A, Watchmaker J, Maymone MBC et al (2020) Cosmetic treatment in patients with autoimmune connective tissue diseases: best practices for patients with lupus erythematosus. J Am Acad Dermatol 83(2):343–363
Decates TS, Velthuis PJ, Schelke LW et al (2020) Increased risk of late-onset, immune-mediated, adverse reactions related to dermal fillers in patients bearing HLA-B*08 and DRB1*03 haplotypes. Dermatol Ther 34(1):e14644. https://doi.org/10.1111/dth.14644
Rogowska P, Walczak P, Wrzosek-Dobrzyniecka K et al (2022) Tattooing in psoriasis: a questionnaire-based analysis of 150 patients. Clin Cosmet Investig Dermatol 6(15):587–593. https://doi.org/10.2147/CCID.S348165
Stolarczyk J, Kubiś M, Brzosko M (2016) Autoimmune/infl ammatory syndrome induced by adjuvants. ASIA Pomeranian J Life Sci 62(1):35–39
Alijotas-Reig J, Fernandez-Figueras MT, Puig L (2012) Inflammatory, immune-mediated adverse reactions related to soft tissue dermal fillers. Semin Arthritis Rheum 43:241–258
Watad A, Rosenberg V, Tiosano S et al (2018) Silicone breast implants and the risk of autoimmune/rheumatic disorders: a real-world analysis. Int J Epidemiol 47(6):1846–1854
Meijs J, de Vries-Bouwstra JK, Cohen Tervaert JW et al (2018) A case of late-onset systemic sclerosis with ruptured silicone breast implants. Neth J Med 76(5):243–248
Psarras A, Gkougkourelas I, Tselios K et al (2014) Systemic sclerosis and silicone breast implant: a case report and review of the literature. Case Rep Rheumatol 2014:809629
Balk EM, Earley A, Avendano EA et al (2016) Long-term health outcomes in women with silicone gel breast implants: a systematic review. Ann Intern Med 164(3):164–175
Kaplan J, Rohrich R (2021) Breast implant illness: a topic in review. Gland Surg 10(1):430–443
Janowsky EC, Kupper LL, Hulka BS (2000) Meta-analyses of the relation between silicone breast implants and the risk of connective-tissue diseases. N Engl J Med 42(11):781–790
Sanchez-Guerrero J, Colditz GA, Karlson EW et al (1995) Silicone breast implants and the risk of connective tissue diseases and symptoms. N Engl J Med 332:1666–1670
Gabriel SE, O’Fallon WM, Kurland LT et al (1994) Risk of connective tissue diseases and other disorders after silicone breast implantation. N Engl J Med 330:1697–1702
Hochberg MC, White B, Steen V (1993) The association of augmentation mammoplasty with systemic sclerosis: preliminary results from a case- control study. Arthritis Rheum 36(Suppl 1):S71
Nyren O, Yin L, Josefsson S et al (1998) Risk of connective tissue disease and related disorders among women with breast implants: a nation-wide retrospective cohort study in Sweden. Br Med J 316:417–422
Faaber P, Capel PJ, Rijke GP et al (1984) Cross-reactivity of anti-DNA antibodies with proteoglycans. Clin Exp Immunol 55:502–508
Sharad J (2020) Hyaluronic acid filler injection for localized scleroderma—case report and review of literature on filler injections for localized scleroderma. Clin Cosmet Investig Dermatol 15:1627–1637. https://doi.org/10.2147/CCID.S356641
Wollina U, Konrad H (2005) Managing adverse events associated with botulinum toxin type A. Am J Clin Dermatol 6(3):141–150
Small R (2014) Botulinum toxin injection for facial wrinkles. Am Fam Physician 90(3):168–175
Huang W, Foster JA, Rogachefsky AS (2000) Pharmacology of botulinum toxin. J Am Acad Dermatol 43(2):249–325
Nayfeh T, Shah S, Malandris K et al (2021) A systematic review supporting the American Society for Dermatologic Surgery guidelines on the prevention and treatment of adverse events of injectable fillers. Dermatol Surg 47(2):227–234. https://doi.org/10.1097/DSS.0000000000002911
Balk EM, Earley A, Avendano EA, Raman G (2016) Long-term health outcomes in women with silicone gel breast implants: a systematic review. Ann Intern Med 164(3):164–175. https://doi.org/10.7326/M15-1169
Funding
The authors received no financial support for the research.
Author information
Authors and Affiliations
Contributions
All the authors conducted the research, prepared, and approved the final version of the manuscript. AFG: conceptualization, investigation, writing. AM and AW: methodology, formal analysis, writing. MO conceptualization, writing. Special thanks to Kornelia Chmurzyńska for reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Felis-Giemza, A., Matusiewicz, A., Wajda, A. et al. Safety of esthetic procedures in rheumatic patients: single-center survey of patients. Rheumatol Int 44, 357–362 (2024). https://doi.org/10.1007/s00296-023-05481-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05481-5