Abstract
The purpose of the present systematic review was to describe the diagnostic evaluation of rheumatoid arthritis in the cervical spine to provide a better understanding of the indications and options of surgical intervention. We performed a literature review of Pub-med, Embase, and Scopus database. Upon implementing specific inclusion and exclusion criteria, all eligible articles were identified. A total of 1878 patients with Rheumatoid Arthritis (RA) were evaluated for cervical spine involvement with plain radiographs. Atlantoaxial subluxation (AAS) ranged from 16.4 to 95.7% in plain radiographs while sub-axial subluxation ranged from 10 to 43.6% of cases. Anterior atlantodental interval (AADI) was found to between 2.5 mm and 4.61 mm in neutral and flexion position respectively, while Posterior Atlantodental Interval (PADI) was between 20.4 and 24.92 mm. 660 patients with RA had undergone an MRI. A pannus diagnosis ranged from 13.33 to 85.36% while spinal cord compression was reported in 0–13% of cases. When it comes to surgical outcomes, Atlanto-axial joint (AAJ) fusion success rates ranged from 45.16 to 100% of cases. Furthermore, the incidence of postoperative subluxation ranged from 0 to 77.7%. With regards to AADI it is evident that its value decreased in all studies. Furthermore, an improvement in Ranawat classification was variable between studies with a report improvement frequency by at least one class ranging from 0 to 54.5%. In conclusion, through careful radiographic and clinical evaluation, cervical spine involvement in patients with RA can be detected. Surgery is a valuable option for these patients and can lead to improvement in their symptoms.
Similar content being viewed by others
Introduction
Rheumatoid arthritis is estimated to affect 0.67% of the world population [1]. This systematic inflammatory process leads to synovitis and pannus formation which primarily involves peripheral joints. However, the inflammatory sequelae of RA can also involve the cervical spine region causing odontoid erosion, loosening of the cervical ligaments and subsequent spinal dislocation. This process was reported in 26.65% of cases in a large cohort of patients diagnosed with RA [2]. Interestingly, corticosteroid use, hands and feet involvement as well as high BMI were proved to be strong predictors of cervical involvement in patients diagnosed with RA [3].
The most common complication of the inflammatory cascade that affects the cervical region is atlantoaxial subluxation (AAS) with instability between C1 and C2 vertebrae. AAS can be divided anatomically to anterior, posterior and vertical AAS. The latter can cause superior migration of the odontoid into the foramen magnum resulting in a condition which is called cranial settling (CS) [4].
Sub-axial subluxation (SAS) is diagnosed when a vertebrae moves forward by at least 3 mm toward the lower adjacent vertebra and it mainly affect C3 to C7. In more severe cases, this process may result in spinal cord compression [5]. Cervical spine involvement in RA can manifest as persistent headaches or a positive Lhermitte’s sign. This sign is the result of compression of the greater and lesser occipital nerve and is usually described as a shooting electrical sensation running down the back when the neck is flexed [6]. Early detection of cervical spine instability is crucial as it can lead to significant neurological morbidity and worsening of quality of life due the compression of critical neural structures [7].
Radiological assessment has an important role to play in the evaluation of cervical spine involvement in RA. According to the European League Against Rheumatism (EULAR), a lateral radiography should be obtained both in neutral and flexion position [8]. The atlantoaxial joint is best assessed using the anterior atlanto-dental interval (AADI) and the posterior atlanto-dental interval (PADI) [9]. Conventional Radiography (CR) does not provide good information regarding synovial inflammation or soft tissue structural changes. For this reason, the leading imaging technique for the assessment of cervical spine involvement in patients with rheumatoid arthritis is MRI. This imaging method enables the early detection of soft tissue involvement and spinal cord compression [10]. MRI is indicated in patients with evidence of AAS on radiographs, in those with neurological signs suggestive cervical myelopathy or radiculopathy and in patients whose symptoms are not controlled with conservative management and are candidates for surgery [11]. MRI has demonstrated greater sensitivity for the detection of synovitis, soft tissue inflammatory changes and erosions at the cranio-vertebral junction when compared to either clinical examination or conventional radiography and also plays a unique role in providing important information early in the course of RA [12]. Despite the reduction in the incidence of cervical spine instability after the addition of the biological agents in the management of RA, surgery has still a vital role in the therapeutic approach [13, 14]. The reason this happens is that once myelopathy occurs, further neurological progression cannot be prevented with neither DMARDS nor biological agents [15]. In a study of patients with RA and myelopathy who did not wish to have surgery, 76% had further neurological deterioration, and all patients were bedridden within 3 years of development of myelopathy [11].
The ultimate goal of surgery is to relieve any neurologic compression and reduce any instability therefore preventing any further neurologic deficit. Many different surgical techniques have been developed over the past years. Occipito-cervical fusion is indicated in cases of cranial settling and C1–C2 fusion is the procedure of choice for atlantoaxial subluxation [16].
In this review, we will discuss the value of CR and MRI evaluated spine disease in RA and provide an overview of the modern surgical techniques as well as outcomes.
Methods
We performed a literature review on Pub-med/Medline, Embase, and Scopus database and assessed all relative references for eligible studies. The following search algorithm was used: “arthritis, rheumatoid” [MeSH Terms] OR (“arthritis” [All Fields] AND “rheumatoid” [All Fields]) OR “rheumatoid arthritis” [All Fields] OR (“rheumatoid” [All Fields] AND “arthritis” [All Fields])) AND (“cervical vertebrae” [MeSH Terms] OR (“cervical” [All Fields] AND “vertebrae” [All Fields]) OR “cervical vertebrae” [All Fields] OR (“cervical” [All Fields] AND “spine” [All Fields]) OR “cervical spine” [All Fields]) AND atlantoaxial [All Fields]. All studies between January 1983 and June 2020 were reviewed. This yielded a total of 259 results. Each of the results was independently reviewed by two authors T.S and C.T. Furthermore, the relative reference lists were manually searched to find eligible studies. The inclusion criteria were: (1) Studies including RA patients with CS available CR or MRI imaging (2) Studies that included patients undergoing surgery for cervical spine instability attributed to RA and it was clearly stated that they were followed post-operatively, (3) Studies including symptomatic patients with RA with regards to cervical involvement. We excluded: (1) Case reports, case series, review of literature, (2) Non-English literature. Improvement in Ranawat scale was considered when there was an improvement of at least 1 Ranawat class above the preoperative assessment. The postoperative outcome was evaluated at the end of the reported follow-up period rather than immediately after surgery. The detailed study flow chart is presented in Fig. 1.
The results were then categorized according to their theme as follows:
-
Commonly reported findings in plain radiographs of patients with RA as well as the incidence of Atlantoaxial and Sub-axial subluxation
-
Evaluation of the outcomes of cervical spine surgery in patients with RA
-
The deterioration of Sub-axial instability preoperatively
The articles selected were then classified according to an evidence-based classification proposed by Wright et al. [17]:
-
I.
High-quality randomized controlled trial
-
II.
Lesser quality randomized controlled trial; prospective comparative study
-
III.
Case–control study; retrospective comparative study
-
IV.
Case series. Expert opinion.
Radiological findings of CS in patients with RA using plain radiography
Plain radiographs are valuable tool for screening for cervical spine involvement (CS) in patients with RA. The main radiological findings in plain radiographs are described below.
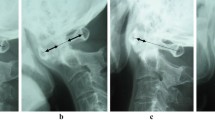
AAI is a condition that affects the stability of the atlanto-axial joint and has been associated with laxity or rupture of the transverse ligament and erosions or fracture of the odontoid process. AAI accounts for approximately 65% of the total subluxations of the spine [18, 19]. Measurement of the anterior atlanto-dental interval (AADI) and posterior atlanto-dental interval (PADI) is used to evaluate the AAI. AADI is defined as the interosseous distance between posterior surface of C1 and the anterior surface of C2. The normal value of AADI in adults should be less than 3 mm. In a study evaluating AADI and PADI during motion of cervical spine using lateral fluoroscopy, AADI in neutral position measures 1.62 mm ± 0.62, whereas at maximal flexion and extension, it increased to 1.88 mm ± 0.85 and 1.63 mm ± 0.61 respectively [20, 21].
AADI > 5 mm is an indicator of clinically significant AAS instability. While AADI > 8 mm has been proposed as the optimal cut-off for surgical management, the various cut-offs range from 6 to 10 mm [5]. It is important to note that the reliability of AADI as an indicator of atlantoaxial instability is limited in patients with cranial settling. In this case, AADI might be mistakenly regarded as decreased when in fact the patient suffers from severe instability [22].
Posterior atlanto-dental interval (PADI) is defined as the distance between the dens and the posterior arch of C1. This distance reflects the width of the spinal cord on C1–C2 level and typically measures between 19 and 27 mm [23]. It is a reliable predictor of the width of the atlantoaxial canal and has shown to be a reliable indicator of myelopathy. This diagnostic tool can also help the surgeon predict postoperative neurologic outcome [24]. PADI < 14 mm has been correlated with adverse surgical outcomes and is more commonly complicated with vertical subluxation [25, 26].
Sub-axial subluxation in CS in RA patients
Sub-axial subluxation (SAS) is diagnosed when the vertebra is horizontally displaced by at least 3.5 mm forward to the adjacent vertebra in a lateral radiograph. This instability involves the lower joints of the cervical spine (C3–C7). The prevalence of SAS in patients who have not undergone surgery in the cervical spine ranges from 15 to 22% [27]. SAS is sometimes described according to the spinal canal diameter. Clinically significant stenosis occurs when the width of the sub-axial canal is less than 14 mm [28]. The patients with sub-axial cervical spine stenosis are more likely to be classified as a Ranawat class II or III (P = 0.01; odds ratio (OR) = 11.43] [29].
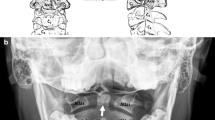
Basilar invagination in CS in RA patients
Basilar Invagination (BI), previously described as cranial settling (CS), is caused by the superior elevation of the odontoid into the already limited space of foramen magnum. The degree of dens displacement was first described with Chamberlain (DOCL) and McGregor line (DOMG). Modern diagnostic criteria include Ranawat criterion, Redlund-Johnell criterion and Clark station. Modified Ranawat measurement extends from midpoint of base of C2 to level of C1, along long axis of odontoid [30]. Redlund-Johnell criterion is the minimum distance between the midpoint of the base of C2 and McGregor’s line [31, 32]. In the Clark station, the dens is divided into three equal parts and determined by the level at which the anterior arch of C1 falls.
Because none of aforementioned criteria individually results in satisfactory sensitivity and specificity, Riew et al. suggested that the presence of CS is best evaluated using a combination of the Clark station, Ranawat criterion, and the Redlund-Johnell criterion. If any of the three criteria is positive, there is a strong probability of cranial settling (sensitivity of 94%, negative predictive value of 91%). However, this method yields only a positive predictive value of 56%, thus making the use of CT or MRI mandatory [33].
Basilar invagination can result in root compression. This complication can be predicted with the use of cervical–medullary angle, which is defined as the angle between a line drawn along the anterior aspects of the cervical–medullary cord and another line along the medulla. The normal angle is 135°–175°. Patients with a cervical–medullary angle < 135° may suffer from cranial settling and clinical signs of C2 root pain [34]. Plain radiographs have not been found to be a reliable diagnostic imaging modality for the detection of BI. Chung et al. reported that Vertical Subluxation (VS) was identified with plain radiographs in 2.30% of patients, whereas in 33.5% MRI scans [35].
Radiological findings of CS in patients with RA using MRI
MRI is mainly used to assess the presence of synovitis, bone marrow edema (BME), odontoid erosions, anterior, posterior or superior VS, and alterations of the cervico-medullary angle.
BME in CS in RA patients
Bone marrow edema (BME) is defined as a poorly defined area of low signal within bone on T1-weighted images that shows high signal intensity on Short Tau Inversion Recovery (STIR) images. The degree of BME is quantified according to an MRI scoring system by measuring the extension of BME in the dens axis as well as in the corpus, facet joints, and spinous process of C2–C7: the dens axis is scored for BME with a scoring of 0 when there is no BME, 1 when BME covers < 1/3 of the bone surface and 2 when BME covers ≥ 1/3 of the bone surface [36]. The presence of BME is strongly associated with the degree of synovitis and it has been proved to be a strong predictor of progressive erosion. In terms of its clinical value, the degree of BME found in MRI has not been proved to be associated with the degree of neck pain [37, 38].
Synovitis in CS in RA patients
Synovitis, as proposed by the OMERACT group, is defined as a thickening of the synovial membrane at the atlantoaxial joint (C1–C2), showing increased water content in fat-suppressed T2-weighted and STIR sequences or an abnormal post-gadolinium enhancement on T1-weighted images [39].
Recent research has focused on the quantitative assessment of inflammatory activity with the introduction of biomarkers such as synovial volume and synovial perfusion with the use of dynamic contrast-enhanced MRI (DCE-MRI) [40]. Fasler et al. demonstrated that DCE-MRI was feasible in 80% of patients despite potential artifacts attributed to the anatomy of the cervical region. Using this imaging modality, pannus volume was quantified and calculated at 5.7 ± 2.4 mL [41]. This kind of quantitative MRI techniques is crucial, since the differentiation between normal enhancement and enhancement attributed to synovitis, especially early in the course of RA, remains a challenge up to date [42].
One of the main benefits of MRI is that it enables early detection of pannus tissue, even when radiographic findings are negative and thus early identification of ligament destructions [43]. Many studies have correlated early atlantoaxial involvement with a number of prognostic factors, the most important of which are anti-citrullinated protein antibodies (ACPAs), high disease activity, as well peripheral erosive disease [36]. With regard to cervical spine, STIR images alone have been shown to be as sensitive and reliable in terms of detection of inflammation as T1-weighted post-contrast images. Omitting the administration of contrast agent saves time and is associated with less cost [44].
Erosion of the odontoid process in CS in RA patients
Odonotoid erosion is a common radiographic finding in patients with RA with a prevalence of 43–47% [43]. Erosion of the odontoid process is defined as a bone defect with sharp margins, visible in two planes. The degree of erosion can be quantified by a scale from 0 to 5 or being dichotomized to whether erosion is present or absent according to the simple erosion narrowing score (SENS) method [45]. Odontoid erosion further deteriorates atlantoaxial instability as it is highly associated with posterior AAS [19]. Furthermore, the chance of neurological dysfunction increases by 5 times when erosion is present [46].
Stenosis of the cervical spinal cord in RA patients
Upper cervical cord or brainstem compression occurs when the subarachnoid space is obstructed which is evident when the cerebrospinal fluid disappears in both the anterior and posterior subarachnoid spaces on T2-weighted images. A deformity of the spinal cord or brainstem appears on MRI imaging as decreased cord diameter at the level of subarachnoid space obstruction compared with the cord diameter superior or inferior to the stenotic level. Sub-axial spinal cord compression is present in cases of obstruction of the subarachnoid space and deformity of the medulla.
Stenosis of the spinal canal is primarily found in the sub-axial level (85%) followed by the atlantoaxial level (44%). Interestingly, a spinal stenosis detected with an MRI has not been found to be correlated with a clinically evident neurological dysfunction except for a stenosis that occurs in the sub-axial level [29].
Despite the significance of MRI in the early detection of spinal cord compression, its additional value compared to function plain radiographs in diagnosing spinal cord compression has been doubted [47]. According to a recent randomized clinical trial, patients who present with symptoms of myelopathy from an acutely inflamed atlantoaxial joint can be relieved by intraarticular injection of steroids [48].
New imaging techniques are gradually introduced in clinical practice and enable the clinician to diagnose abnormalities of the spinal cord before the onset of irreversible damage. One of them is DWI which has been found to be useful in the identification of spinal cord compression due to anterior AAS by measuring the ADC values at C1 level (ADC1). The latter have been found to be higher in the group with anterior AAS than in the group without AAS (P < 0.001) [49].
Studies looking at cervical involvement in patients with RA with plain radiographs and MRI
We identified 18 studies evaluating cervical spine involvement in patients with rheumatoid arthritis with plain radiographs that met our inclusion and exclusion criteria.
A total of 1878 patients were included (Table 1). Useful views for evaluation are upright AP and lateral, open-mouth (odontoid view), and flexion–extension for detection of instability. AAS was the most frequently encountered cervical abnormality, with its frequency ranging from 16.4 to 95.7% in plain radiographs. SAS diagnosis was found in 10–43.6% of cases. ADI was found to be ranging from 2.5 to 4.61 mm in neutral position. PADI ranged from 20.4 to 24.92 mm.
With regard to the evaluation of CS in RA patients with MRI, 13 studies were found. The most commonly reported MRI findings in patients with rheumatoid arthritis are found in Table 2. In a total of 660 patients, AAS and SAS frequency ranged from 4 to 87.8% and 0 to 13.6% respectively. Odontoid erosion was a frequently encountered finding reported in 16–85.36%. A pannus diagnosis ranged from 13.33 to 85.36%, while evidence of spinal cord compression was reported in 0–13% of cases. What is more, very few studies reported BME either at the atlantoaxial or sub-axial level.
Surgical management of CS involvement in RA patients
Surgical management is mainly indicated when the patient suffers from myelopathy and/or neurological dysfunction. Surgery typically consists of a decompressive procedure to relieve the compression of the spinal cord in combination with a fusion procedure which aim to eradicate any instability. This stabilization process also prevents further progression into VS or SAS.
Atlantoaxial stabilization can be performed via either an anterior or posterior approach depending on the site of compression and the surgeon’s preference [71]. Sunahara et al. demonstrated the vital role of cervical spine surgery in a sample of 21 patients with RA who were not managed surgically. 16 of the patients deteriorated at follow-up and the chance of surviving 7 years after the onset of myelopathy was 0% [72]. Surgery has also played a role in pannus regression, an inflammatory complication of RA. Bydon et.al demonstrated that the mean volume of pannus decreased by 44% in patients managed with posterior fusion with or without decompression [73].
The most commonly employed technique for C1–C2 instability is C1–C2 fusion. This technique is mainly indicated in patients without other coexisting cervical deformities. With regard to preoperative considerations, methotrexate should not be discontinued. As for the biological agents, it is recommended that they should be stopped one week prior to the operation although this view has been challenged by Kawakami et.al who found no significant adverse effects postoperatively in patients who continued taking biological agent before surgery. On the other hand, Ozen et al., in a large series of 11.623 patients found that the incidence of surgical infection was higher in patients taking tumor necrosis factor α inhibitors (TNFis) when compared to the ones taking conventional DMARDS [74, 75].
The technique most commonly employed is the one introduced by Harms and Melcher and involves the fixation of posterior C1 lateral mass and C2 pedicle using screws and rods. In this procedure, the surgeon must seriously consider the course of the vertebral artery (VA), as the risk of injuring the latter is estimated at 4.1%. Patients with RA may have a special anatomy of the cervical region as they were found to have smaller left internal height 4.21 ± 1.63 and a pedicle width of 4.11 ± 1.05 of C2 [76,77,78].
Furthermore, after the comparison between anterior and posterior approach, Chieng found in a meta-analysis that 68% of patients treated with an anterior approach improved their neurological status, while the same figure for patients managed with posterior approach was 98% [79]. When AAI occurs posteriorly, occipito-cervical fixation is mandatory. The latter is also indicated as a reoperation technique when the instrumentation in C1–C2 fail. This occurred in a series of 66 patients in 11% of cases at a mean time of 28 months. The most important consideration in the occipito-cervical fusion is the occipito-cervical angle, as it has a significant impact on the postoperative outcome. Two cervical angles that have proved of great importance are Occipitoaxial Angle and Posterior Occipitocervical Angle which normally measure 14.5° ± 3.7° and 108.2° ± 8.1°, respectively. The latter has been correlated with the need for reoperation when elevated [80, 81].
With the regard to the outcome of cervical spine approaches used to treat myelopathy, this is evaluated with the use of Japanese Orthopaedic Association scoring system (JOA). The latter is a questionnaire which is answered by the patients themselves and assesses preoperative versus postoperative neurological status. JOA score is significantly improved postoperatively in patients without SAS. To overcome some limitations of JOA score, a new score was introduced called the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ), which focuses more on the patients’ quality of life and general health [82]. Preoperative Ranawat classification is also an important predictor of postoperative outcome. Postoperative improvement is defined as improvement of at least 1 Ranawat classification above the preoperative assessment. Interestingly, outcome of surgery in terms of neurological function is not affected by the degree of dislocation preoperatively [83]. The degree of atlantoaxial fusion can be evaluated by comparing preoperative ADI versus postoperative ADI. The visual analog scale (VAS) is frequently used to measure treatment outcome in patients with cervical spine disorders in a scale of 0–100 mm [84].
Endoscopical approach
An anterior approach is mainly indicated when there is anterior spinal cord compression due to irreducible basilar invagination (BI) and/or rheumatoid pannus (RP). Otherwise, posterior C1–C2 fusion is the preferred technique. The former approach enables direct decompression, while the latter enables stabilization of the alignment of the cervical spine. The optimal method to treat cervical spine instability remains still a controversy to date [85].
The odontoid can be accessed either with the trans-oral or the endo-nasal approach. The latter, which is often referred to as Endoscopic Endo-nasal Approach (EEA) provides a better surgical field and presents less postoperative complications as opposed to the trans-oral approach (TOA), but no clear superiority of the EEA over the endoscopic TOA has been proved [86, 87]. This procedure is in most cases accompanied by posterior fusion to prevent subsequent C1–C2 instability. However, Iacongeli et al. presented a case series of 7 patients which showed that C1 ach can be preserved. The main advantage of this less invasive approach is that it prevents future cranial settling and progression of C1–C2 instability [88]. Despite its crucial benefits, it is important to note that trans-nasal approach has been more frequently associated with intra-operative CSF leaks than the trans-oral approach (30 and 0.3% respectively). This leak, however, remains in the follow-up period only in a minority of patients. In a review of literature, Morales Varelo et al. included 72 patients undergoing EEA due to various etiologies including 28 with rheumatoid pannus. This study showed that EEA is a safe approach with a procedure-related mortality of just 1.4% [89].
Odontoidectomy can also be performed via the trans-cervical root which offers significant improvement in terms of myelopathy and is accompanied by only few complications, such as a urinary tract infection, upper airway swelling, and dysphagia. This is the technique of choice once cranial settling has occurred [90].
Novel surgical techniques are gradually introduced in clinical setting. For instance, cervical pedicle placement with intraoperative CT guidance in 20 consecutive patients with rheumatoid arthritis was reported to have an overall malposition rate of 2.4%. Jha et al. proposed an alternative technique of C1–C2 posterior fusion with use of operative video, thus minimizing intra-operative blood loss and C2 dorsal root ganglia [91]. It is worth mentioning that in the event of surgical failure, a conservative approach has been proved to reduce rheumatoid pannus considerably using a rigid cervical collar [92].
Studies looking at the surgical management of CS in RA patients
Looking at the studies assessing surgical management of CS involvement in patients with RA, we found a total of 17 studies which assessed postoperative outcomes and seven studies that evaluated the potential rise in the incidence of postoperative subluxation compared to the preoperative ones. There were studies that evaluated both outcomes and were therefore reported twice in each individual table.
In Table 3, we present the surgical outcomes of the included studies. This was evaluated by the degree of increase in JOA score, whether patients were classified at lower Ranawat class after surgery, by the proportion of patients which AAJ fusion was successful and by the drop in mean AADI postoperatively. JOA score increased postoperatively in all but one study (Kurogochi et.al) in which it remained stable. AAJ fusion was successful in the vast majority of patients undergoing cervical stabilization surgery and more specifically ranged from 45.16 to 100% of cases. With regard to AADI, it is evident that its value decreased post-operatively in all studies. Furthermore, an improvement in Ranawat classification was variable between studies with a reported improvement frequency by at least one class ranging from 0 to 54.5%.
In Table 4, we present the studies evaluating the incidence of preoperative sub-axial subluxation compared to the respective figure after surgery. In a sample of 213 patients undergoing posterior C1–C2 fixation postoperative subluxation ranging from 0 to 77.7%. This is in line with literature which suggests that one feared complication of posterior C1–C2 fixation is SAS.
Discussion
RA diagnosis in CS patients is important as it is associated with high morbidity and mortality [19]. The frequency of the radiological findings of CS in RA patients varies significantly, mostly due to the study design of published articles [59]. The most commonly reported abnormality in plain radiographs of patients with RA and CS involvement was AAS followed by SAS. Interestingly, SAS was diagnosed in 10–43.6% of cases using plain radiography versus 0 to 13.6% when using MRI. MRI is a useful technique for the evaluation of soft tissue changes and bone erosive changes for instance odontoid erosion, pannus formation and spinal cord compression. RA disease duration was high in the included studies ranging from 1 to 18.1 years. It is worth noting that most of the cases with early radiological changes were noted in the MRI group of studies [36, 64, 65]. This is in line with literature that suggests radiological changes visible in plain radiography present usually at a later stage [71].
Regarding surgical management of CS in RA patients, although the aim of atlantoaxial fixation is to hinder further progression of cervical instability, post-operative SAS ranged from 0 to 77% in our sample. This complication is possibly attributed to the high mechanical stress during the surgical procedure [110]. Interestingly, Ishii et.al demonstrated that SAS occurred mainly at the C3-C4 level in 42% of cases [107].
Post-operative outcomes after cervical spine surgery in RA patients were variable. Improvement in Ranawat scale by a least one class was noted from 0 to 54% of cases. This is in line with literature which states that patients typically improve by one class after undergoing cervical spine fusion [71, 105, 111].
There have been significant changes in the management of RA during the last decades. This is mostly due to the development and approval of new biological (b) DMARDs in the treatment protocol of patients with RA. The novel target to treat (T2T) approach using conventional synthetic (cs) or targeting synthetic (ts) DMARDs, along with bDMARDs has improved significantly the outcomes and the rates of disease progression [112]. According to the NEO-RACo Study, in patients with early RA that received a triple combination of csDMARD and prednisolone, the rate of CS involvement was only 4.7% by 10 years, with AAS and SAS rate being only 1.2%. This is particularly important given the high rates of post-operative complications of surgically managed cases of RA, namely SAS. In patients with already unstable spine, surgery seems to be the mainstay of treatment to decelerate disease progression and improve long term outcomes [101].
There are limitations to this study that should be considered when interpreting the results. The frequency of radiological findings of CS involvement in patients with RA varies significantly. This is because the majority of the included articles are cross-sectional and retrospective and only a minority of them were designed for early RA assessment. There are multiple factors that might affect the frequency of the radiological findings in CS for instance disease duration, suboptimal treatment, seropositivity, involvement of multiple joints and the degree of joint damage. Radiological findings in cervical spine in RA patients are usually late findings. Therefore, prospective studies evaluating the incidence of cervical spine involvement in RA and the radiological abnormalities would be recommended. Furthermore, we only looked at studies including patients with recorded post-operative follow-up to assess post-operative outcomes.
Conclusion
To the best of our knowledge, this the first study that summarizes the data regarding imaging findings and surgical management in patients with RA and cervical spine involvement. Plain radiographs have an important role to play in the evaluation of cervical spine involvement in RA. Given that radiological findings present at a later stage, screening of patient with CS involvement with CR is encouraged. MRI enables the early detection of soft tissue involvement and spinal cord compression. AAS was the most frequently encountered radiological abnormality. Although the incidence of cervical spine instability has been decreased after the addition of the biological agents in the management of RA, surgery has still a vital role in the therapeutic approach.
Data availability statement
Data available on request.
Abbreviations
- AADI:
-
Anterior atlantodental interval
- AAJ:
-
Atlanto-axial joint
- AAS:
-
Atlantoaxial subluxation
- ACPA:
-
Anti-citrullinated protein antibodies
- BI:
-
Basilar Invagination (BI)
- BME:
-
Bone marrow edema
- CR:
-
Conventional radiography
- CS:
-
Cervical spine
- CS:
-
Cranial settling
- CT:
-
Computed tomography
- DCE- MRI:
-
Dynamic contrast-enhanced magnetic resonance imaging
- DMARD:
-
Disease modifying drugs
- EEA:
-
Endoscopic endonasal approach
- JOA:
-
Japanese Orthopaedic Association scoring system
- MRI:
-
Magnetic resonance imaging
- OCF:
-
Occipitocervical fixation
- PADI:
-
Posterior atlantodental interval
- RA:
-
Rheumatoid arthritis
- SAS:
-
Subaxial subluxation
- SCC:
-
Spinal cord compression
- STIR:
-
Short tau inversion recovery
- TOA:
-
Transoral approach
- VS:
-
Vertical subluxation
References
Abhishek A, Doherty M, Kuo C-F, Mallen CD, Zhang W, Grainge MJ (2017) Rheumatoid arthritis is getting less frequent–results of a nationwide population-based cohort study. Rheumatology (Oxford) 56:736–744. https://doi.org/10.1093/rheumatology/kew468
Zhu S, Xu W, Luo Y, Zhao Y, Liu Y (2017) Cervical spine involvement risk factors in rheumatoid arthritis: a meta-analysis. Int J Rheum Dis 20:541–549. https://doi.org/10.1111/1756-185X.13096
Han M-H, Ryu JI, Kim CH, Kim JM, Cheong JH, Bak KH, Chun HJ, Yi H-J, Jun JB, Chung JW (2017) Factors that predict risk of cervical instability in rheumatoid arthritis patients. Spine 42:966–973. https://doi.org/10.1097/BRS.0000000000001942
El-Khoury GY, Wener MH, Menezes AH, Dolan KD, Kathol ME (1980) Cranial settling in rheumatoid arthritis. Radiology 137:637–642. https://doi.org/10.1148/radiology.137.3.7444048
Mańczak M, Gasik R (2017) Cervical spine instability in the course of rheumatoid arthritis–imaging methods. Reumatologia 55:201–207. https://doi.org/10.5114/reum.2017.69782
Behrouz R (2014) The risk of ischemic stroke in major rheumatic disorders. J Neuroimmunol 277:1–5. https://doi.org/10.1016/j.jneuroim.2014.09.009
Reijnierse M, van der Helm-Mil A, Eshed I, Schueller-Weidekamm C (2018) Magnetic resonance imaging of rheumatoid arthritis: peripheral joints and spine. Semin Musculoskelet Radiol 22:127–146. https://doi.org/10.1055/s-0038-1639474
Colebatch AN, Edwards CJ, Østergaard M, van der Heijde D, Balint PV, D’Agostino M-A, Forslind K, Grassi W, Haavardsholm EA, Haugeberg G, Jurik A-G, Landewé RBM, Naredo E, O’Connor PJ, Ostendorf B, Potocki K, Schmidt WA, Smolen JS, Sokolovic S, Watt I, Conaghan PG (2013) EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis 72:804–814. https://doi.org/10.1136/annrheumdis-2012-203158
Joaquim AF, Ghizoni E, Tedeschi H, Appenzeller S, Riew KD (2015) Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg Focus 38:E4. https://doi.org/10.3171/2015.1.FOCUS14664
Tehranzadeh J, Ashikyan O, Dascalos J (2003) Magnetic resonance imaging in early detection of rheumatoid arthritis. Semin Musculoskelet Radiol 7:79–94. https://doi.org/10.1055/s-2003-41342
Wasserman BR, Moskovich R, Razi AE (2011) Rheumatoid arthritis of the cervical spine–clinical considerations. Bull NYU Hosp Jt Dis 69:136–148
Suppiah R, Doyle A, Rai R, Dalbeth N, Lobo M, Braun J, McQueen FM (2010) Quantifying bone marrow edema in the rheumatoid cervical spine using magnetic resonance imaging. J Rheumatol 37:1626–1632. https://doi.org/10.3899/jrheum.091299
Kaito T, Ohshima S, Fujiwara H, Makino T, Yonenobu K, Yoshikawa H (2017) Incidence and risk factors for cervical lesions in patients with rheumatoid arthritis under the current pharmacologic treatment paradigm. Mod Rheumatol 27:593–597. https://doi.org/10.1080/14397595.2016.1253649
Sandström T, Rantalaiho V, Yli-Kerttula T, Kautiainen H, Malmi T, Karjalainen A, Uusitalo T, Julkunen H (2019) Cervical spine involvement is very rare in patients with rheumatoid arthritis treated actively with treat to target strategy. Ten-year results of the NEORACo study. J Rheumatol. https://doi.org/10.3899/jrheum.190139
Mallory GW, Halasz SR, Clarke MJ (2014) Advances in the treatment of cervical rheumatoid: less surgery and less morbidity. World J Orthop 5:292–303. https://doi.org/10.5312/wjo.v5.i3.292
Kaito T, Ohshima S, Fujiwara H, Makino T, Takenaka S, Sakai Y, Yoshikawa H (2019) Predictors for progression of two different types of cervical lesions in rheumatoid arthritis treated with biologic agents. J Orthop Sci 24:214–218. https://doi.org/10.1016/j.jos.2018.09.001
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85:1–3
Shen FH, Samartzis D, Jenis LG, An HS (2004) Rheumatoid arthritis: evaluation and surgical management of the cervical spine. Spine J 4:689–700. https://doi.org/10.1016/j.spinee.2004.05.001
Nguyen HV, Ludwig SC, Silber J, Gelb DE, Anderson PA, Frank L, Vaccaro AR (2004) Rheumatoid arthritis of the cervical spine. Spine J 4:329–334. https://doi.org/10.1016/j.spinee.2003.10.006
Meyer C, Bredow J, Heising E, Eysel P, Müller LP, Stein G (2017) Rheumatoid arthritis affecting the upper cervical spine: biomechanical assessment of the stabilizing ligaments. Biomed Res Int. https://doi.org/10.1155/2017/6131703
Da Côrte FC, Neves N (2014) Cervical spine instability in rheumatoid arthritis. Eur J Orthop Surg Traumatol 24:83–91. https://doi.org/10.1007/s00590-013-1258-2
Casey ATH, Crockard HA, Geddes JF, Stevens J (1997) Vertical translocation: the enigma of the disappearing atlantodens interval in patients with myelopathy and rheumatoid arthritis. Part I. Clinical, radiological, and neuropathological features. J Neurosurg 87:856–862. https://doi.org/10.3171/jns.1997.87.6.0856
Monsey RD (1997) Rheumatoid arthritis of the cervical spine. J Am Acad Orthop Surg 5:240–248. https://doi.org/10.5435/00124635-199709000-00002
Boden SD, Dodge LD, Bohlman HH, Rechtine GR (1993) Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am 75:1282–1297. https://doi.org/10.2106/00004623-199309000-00004
Imagama S, Oishi Y, Miura Y, Kanayama Y, Ito Z, Wakao N, Ando K, Hirano K, Tauchi R, Muramoto A, Matsuyama Y, Ishiguro N (2010) Predictors of aggravation of cervical spine instability in rheumatoid arthritis patients: the large joint index. J Orthop Sci 15:540–546. https://doi.org/10.1007/s00776-010-1475-z
Drosos AA, Pelechas E, Voulgari PV (2020) Radiological findings of the cervical spine in rheumatoid arthritis: what a rheumatologist should know. Curr Rheumatol Rep 22:19. https://doi.org/10.1007/s11926-020-00894-8
Neva MH, Häkkinen A, Mäkinen H, Hannonen P, Kauppi M, Sokka T (2006) High prevalence of asymptomatic cervical spine subluxation in patients with rheumatoid arthritis waiting for orthopaedic surgery. Ann Rheum Dis 65:884–888. https://doi.org/10.1136/ard.2005.042135
Panjabi MM, White AA (1980) Basic biomechanics of the spine. Neurosurgery 7:76–93. https://doi.org/10.1227/00006123-198007000-00014
Narváez J, Narváez JA, Serrallonga M, de Lama E, Hernández-Gañan J, Gómez-Vaquero C, Nolla JM (2015) Subaxial cervical spine involvement in symptomatic rheumatoid arthritis patients: comparison with cervical spondylosis. Semin Arthritis Rheum 45:9–17. https://doi.org/10.1016/j.semarthrit.2015.02.014
Ranawat CS, O’Leary P, Pellicci P, Tsairis P, Marchisello P, Dorr L (1979) Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am 61:1003–1010
Redlund-Johnell I, Pettersson H (1984) Radiographic measurements of the craniovertebral region designed for evaluation of abnormalities in rheumatoid arthritis. Acta Radiol Diagn (Stockh) 25(1):23–28
Kwong Y, Rao N, Latief K (2011) Craniometric measurements in the assessment of craniovertebral settling: are they still relevant in the age of cross-sectional imaging? Am J Roentgenol 196:W421-425. https://doi.org/10.2214/AJR.10.5339
Riew KD, Hilibrand AS, Palumbo MA, Sethi N, Bohlman HH (2001) Diagnosing basilar invagination in the rheumatoid patient. The reliability of radiographic criteria. J Bone Joint Surg Am 83:194–200. https://doi.org/10.2106/00004623-200102000-00006
Guo X, Han Z, Xiao J, Chen Q, Chen F, Guo Q, Yang J, Ni B (2019) Cervicomedullary angle as an independent radiological predictor of postoperative neurological outcome in type A basilar invagination. Sci Rep 9:1–7. https://doi.org/10.1038/s41598-019-55780-w
Chung J, Bak KH, Yi H-J, Chun HJ, Ryu JI, Han M-H (2019) Upper cervical subluxation and cervicomedullary junction compression in patients with rheumatoid arthritis. J Korean Neurosurg Soc 62:661–670. https://doi.org/10.3340/jkns.2018.0234
Carotti M, Salaffi F, Di Carlo M, Sessa F, Giovagnoni A (2019) Magnetic resonance imaging of the craniovertebral junction in early rheumatoid arthritis. Skeletal Radiol 48:553–561. https://doi.org/10.1007/s00256-018-3055-9
Dreyer SJ, Boden SD (1999) Natural history of rheumatoid arthritis of the cervical spine. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199909000-00013
Baraliakos X, Heldmann F, Callhoff J, Suppiah R, McQueen FM, Krause D, Klink C, Schmitz-Bortz E, Igelmann M, Kalthoff L, Kiltz U, Schmuedderich A, Braun J (2016) Quantification of bone marrow edema by magnetic resonance imaging only marginally reflects clinical neck pain evaluation in rheumatoid arthritis and ankylosing spondylitis. J Rheumatol 43:2131–2135. https://doi.org/10.3899/jrheum.150553
Østergaard M, Peterfy C, Conaghan P, McQueen F, Bird P, Ejbjerg B, Shnier R, O’Connor P, Klarlund M, Emery P, Genant H, Lassere M, Edmonds J (2003) OMERACT rheumatoid arthritis magnetic resonance imaging studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol 30:1385–1386
Notohamiprodjo M, Glaser C, Horng A, Helck A, Bauner KU, Reiser MF, Hatz HJ, Weckbach S (2012) Dynamic 3D-MR-angiography for assessing rheumatoid disease of the hand–a feasibility study. Eur J Radiol 81:951–956. https://doi.org/10.1016/j.ejrad.2011.01.031
Fasler DA, Ingrisch M, Nanz D, Weckbach S, Kyburz D, Fischer DR, Guggenberger R, Andreisek G (2020) Rheumatoid cervical pannus: feasibility of volume and perfusion quantification using dynamic contrast enhanced time resolved MRI. Acta Radiol 61:227–235. https://doi.org/10.1177/0284185119854200
Ejbjerg B, Narvestad E, Rostrup E, Szkudlarek M, Jacobsen S, Thomsen HS, Østergaard M (2004) Magnetic resonance imaging of wrist and finger joints in healthy subjects occasionally shows changes resembling erosions and synovitis as seen in rheumatoid arthritis. Arthritis Rheum 50:1097–1106. https://doi.org/10.1002/art.20135
Hermann K-GA, Bollow M (2004) Magnetic resonance imaging of the axial skeleton in rheumatoid disease. Best Pract Res Clin Rheumatol 18:881–907. https://doi.org/10.1016/j.berh.2004.06.005
Axelsen MB, Eshed I, Østergaard M, Hetland ML, Møller JM, Jensen DV, Krintel SB, Hansen MS, Terslev L, Klarlund M, Poggenborg RP, Balding L, Pedersen SJ (2017) Monitoring total-body inflammation and damage in joints and entheses: the first follow-up study of whole-body magnetic resonance imaging in rheumatoid arthritis. Scand J Rheumatol 46:253–262. https://doi.org/10.1080/03009742.2016.1231338
Dias EM, Lukas C, Landewé R, Fatenejad S, van der Heijde D (2008) Reliability and sensitivity to change of the simple erosion narrowing score compared with the sharp-van der Heijde method for scoring radiographs in rheumatoid arthritis. Ann Rheum Dis 67:375–379. https://doi.org/10.1136/ard.2007.072785
Reijnierse M, Bloem JL, Dijkmans BAC, Kroon HM, Holscher HC, Hansen B, Breedveld FC (1996) The cervical spine in rheumatoid arthritis: relationship between neurologic signs and morphology on MR imaging and radiographs. Skeletal Radiol 25:113–118. https://doi.org/10.1007/s002560050046
Reijnierse M, Breedveld FC, Kroon HM, Hansen B, Pope TL, Bloem JL (2000) Are magnetic resonance flexion views useful in evaluating the cervical spine of patients with rheumatoid arthritis? Skeletal Radiol 29:85–89. https://doi.org/10.1007/s002560050015
Hetta DF, Elawamy AM, Hassanein MM, Aljohi AS, Hasan RA-R, Mohammed NAA, Seifeldein GS (2019) Efficacy of atlantoaxial joint glucocorticoid injection in patients with rheumatoid arthritis: a randomized trial. Pain Physician 22:E295–E302
Mańczak M, Pracoń G, Sudoł-Szopińska I, Gasik R (2019) Apparent diffusion coefficient as an indicator of spinal cord compression due to anterior atlanto-axial subluxation in rheumatoid arthritis patients. Eur Spine J 28:2352–2358. https://doi.org/10.1007/s00586-019-06058-2
Passos Cardoso AL, Da Silva NA, Daher S, De Moraes FB, Do Carmo HF (2010) Evaluation of the cervical spine among patients with rheumatoid arthritis. Rev Bras Ortop 45:160–165. https://doi.org/10.1016/S2255-4971(15)30287-1
Alcala JMF, Douat D, Pinheiro DL, Kamei DJ, dos Santos FRM, Silva MB, Skare TL (2013) Radiographic changes of cervical spine in rheumatoid arthritis. Rev Bras Reumatol 53:388–393
Younes M, Belghali S, Kriâa S, Zrour S, Bejia I, Touzi M, Golli M, Gannouni A, Bergaoui N (2009) Compared imaging of the rheumatoid cervical spine: prevalence study and associated factors. Joint Bone Spine 76:361–368. https://doi.org/10.1016/j.jbspin.2008.10.010
Zikou AK, Alamanos Y, Argyropoulou MI, Tsifetaki N, Tsampoulas C, Voulgari PV, Efremidis SC, Drosos AA (2005) Radiological cervical spine involvement in patients with rheumatoid arthritis: a cross sectional study. J Rheumatol 32:801–806
Macovei L-A, Rezus E (2016) Cervical spine lesions in rheumatoid arthritis patients. Med Surg J 120:70–76
Hagenow A, Seifert J, Zeissig A, Conrad K, Kleymann A, Aringer M (2013) Relevant incidence of cervical arthritis in patients with erosive seropositive rheumatoid arthritis even today. Clin Exp Rheumatol 31:213–218
Kanayama Y, Kojima T, Hirano Y, Shioura T, Hayashi M, Funahashi K, Ishiguro N (2010) Radiographic progression of cervical lesions in patients with rheumatoid arthritis receiving infliximab treatment. Mod Rheumatol 20:273–279. https://doi.org/10.1007/s10165-010-0276-8
Taniguchi D, Tokunaga D, Hase H, Mikami Y, Hojo T, Ikeda T, Oda R, Takatori R, Imai K, Kida Y, Otakara E, Ito H, Nishimura T, Kubo T (2008) Evaluation of lateral instability of the atlanto-axial joint in rheumatoid arthritis using dynamic open-mouth view radiographs. Clin Rheumatol 27:851–857. https://doi.org/10.1007/s10067-007-0809-5
Maeda T, Saito T, Harimaya K, Shuto T, Iwamoto Y (2004) Atlantoaxial instability in neck retraction and protrusion positions in patients with rheumatoid arthritis. Spine 29:757–762. https://doi.org/10.1097/01.brs.0000113891.27658.5f
Blom M, Creemers MCW, Kievit W, Lemmens JAM, van Riel PLCM (2013) Long-term follow-up of the cervical spine with conventional radiographs in patients with rheumatoid arthritis. Scand J Rheumatol 42:281–288. https://doi.org/10.3109/03009742.2012.747625
Yurube T, Sumi M, Nishida K, Miyamoto H, Kohyama K, Matsubara T, Miura Y, Hirata H, Sugiyama D, Doita M (2014) Accelerated development of cervical spine instabilities in rheumatoid arthritis: a prospective minimum 5-year cohort study. PLoS ONE 9:e88970. https://doi.org/10.1371/journal.pone.0088970
Yurube T, Sumi M, Nishida K, Takabatake M, Kohyama K, Matsubara T, Ozaki T, Maeno K, Kakutani K, Zhang Z, Doita M, Conference KS (2011) Progression of cervical spine instabilities in rheumatoid arthritis: a prospective cohort study of outpatients over 5 years. Spine 36:647–653. https://doi.org/10.1097/BRS.0b013e3181da21c5
Yan W-J, Liu T-L, Zhou X-H, Chen X-S, Yuan W, Jia L-S (2008) Clinical characteristics and diagnosis of rheumatoid arthritis of upper cervical spine: analysis of 71 cases. Zhonghua Yi Xue Za Zhi 88:901–904
Takahashi S, Suzuki A, Koike T, Yamada K, Yasuda H, Tada M, Sugioka Y, Okano T, Nakamura H (2014) Current prevalence and characteristics of cervical spine instability in patients with rheumatoid arthritis in the era of biologics. Mod Rheumatol 24:904–909. https://doi.org/10.3109/14397595.2014.895123
Jeromel M, Jevtič V, Serša I, Ambrožič A, Tomšič M (2012) Quantification of synovitis in the cranio-cervical region: dynamic contrast enhanced and diffusion weighted magnetic resonance imaging in early rheumatoid arthritis–a feasibility follow up study. Eur J Radiol 81:3412–3419. https://doi.org/10.1016/j.ejrad.2012.04.006
Magarelli N, Simone F, Amelia R, Leone A, Bosello S, D’Antona G, Zoli A, Ferraccioli G, Bonomo L (2010) MR imaging of atlantoaxial joint in early rheumatoid arthritis. Radiol Med 115:1111–1120. https://doi.org/10.1007/s11547-010-0574-4
Narváez JA, Narváez J, Serrallonga M, De Lama E, de Albert M, Mast R, Nolla JM (2008) Cervical spine involvement in rheumatoid arthritis: correlation between neurological manifestations and magnetic resonance imaging findings. Rheumatology (Oxford) 47:1814–1819. https://doi.org/10.1093/rheumatology/ken314
Oláh C, Kardos Z, Kostyál L, Hodosi K, Tamási L, Bereczki D, Szekanecz Z (2020) Assessment of cervical spine involvement in rheumatoid arthritis patients in the era of biologics: a real-life, cross-sectional MRI study. Rheumatol Int. https://doi.org/10.1007/s00296-020-04549-w
Zikou AK, Argyropoulou MI, Alamanos Y, Tsifetaki N, Tsampoulas C, Voulgari PV, Efremidis SC, Drosos AA (2005) Magnetic resonance imaging findings of the cervical spine in patients with rheumatoid arthritis. A cross-sectional study. Clin Exp Rheumatol 23:665–670
Schwarz-Eywill M, Friedberg R, Stösslein F, Unger L, Nüsslein H (2005) Rheumatoid arthritis at the cervical spine—an underestimated problem. Dtsch Med Wochenschr 130:1866–1870. https://doi.org/10.1055/s-2005-871909
Daoud L, Kochbati S (2009) Magnetic resonance imaging evaluation of the cervical spine in patients with rheumatoid arthritis. Report of 30 cases. Tunis Med 87:375–379
Gillick JL, Wainwright J, Das K (2015) Rheumatoid arthritis and the cervical spine: a review on the role of surgery. Int J Rheumatol. https://doi.org/10.1155/2015/252456
Sunahara N, Matsunaga S, Mori T, Ijiri K, Sakou T (1997) Clinical course of conservatively managed rheumatoid arthritis patients with myelopathy. Spine 22:2603–2607. https://doi.org/10.1097/00007632-199711150-00004 (discussion 2608)
Bydon M, Macki M, Qadi M, De la Garza-Ramos R, Kosztowski TA, Sciubba DM, Wolinsky J-P, Witham TF, Gokaslan ZL, Bydon A (2015) Regression of an atlantoaxial rheumatoid pannus following posterior instrumented fusion. Clin Neurol Neurosurg 137:28–33. https://doi.org/10.1016/j.clineuro.2015.06.010
Kawakami K, Ikari K, Kawamura K, Tsukahara S, Iwamoto T, Yano K, Sakuma Y, Tokita A, Momohara S (2010) Complications and features after joint surgery in rheumatoid arthritis patients treated with tumour necrosis factor-alpha blockers: perioperative interruption of tumour necrosis factor-alpha blockers decreases complications? Rheumatology (Oxford) 49:341–347. https://doi.org/10.1093/rheumatology/kep376
Ozen G, Pedro S, Schumacher R, Simon TA, Michaud K (2019) Safety of abatacept compared with other biologic and conventional synthetic disease-modifying antirheumatic drugs in patients with rheumatoid arthritis: data from an observational study. Arthritis Res Ther 21:141. https://doi.org/10.1186/s13075-019-1921-z
Harms J, Melcher RP (2001) Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 26:2467–2471. https://doi.org/10.1097/00007632-200111150-00014
Wright NM, Lauryssen C (1998) Vertebral artery injury in C1–2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American association of neurological surgeons/congress of neurological surgeons. J Neurosurg 88:634–640. https://doi.org/10.3171/jns.1998.88.4.0634
Moon BJ, Choi KH, Shin DA, Yi S, Kim KN, Yoon DH, Ha Y (2018) Anatomical variations of vertebral artery and C2 isthmus in atlanto-axial fusion: consecutive surgical 100 cases. J Clin Neurosci 53:147–152. https://doi.org/10.1016/j.jocn.2018.04.058
Chieng LO, Madhavan K, Vanni S (2015) Pooled data analysis on anterior versus posterior approach for rheumatoid arthritis at the craniovertebral junction. Neurosurg Focus 38:E18. https://doi.org/10.3171/2015.1.FOCUS14838
Maulucci CM, Ghobrial GM, Sharan AD, Harrop JS, Jallo JI, Vaccaro AR, Prasad SK (2014) Correlation of posterior occipitocervical angle and surgical outcomes for occipitocervical fusion. Evid Based Spine Care J 5:163–165. https://doi.org/10.1055/s-0034-1386756
Tang C, Li GZ, Liao YH, Tang Q, Ma F, Wang Q, Zhong DJ (2019) Importance of the Occipitoaxial Angle and Posterior Occipitocervical Angle in Occipitocervical Fusion. Orthop Surg 11:1054–1063. https://doi.org/10.1111/os.12553
Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T, Takahashi K, Takeshita K, Tani T, Toyama Y, Yonenobu K, Wada E, Tanaka T, Hirota Y (2008) Japanese orthopaedic association cervical myelopathy evaluation questionnaire (JOACMEQ): part 4. Establishment of equations for severity scores. J Orthop Sci 13:25–31. https://doi.org/10.1007/s00776-007-1194-2
Iizuka H, Iizuka Y, Mieda T, Kobayashi R, Nishinome M, Ara T, Sorimachi Y, Nakajima T, Takagishi K (2017) A retrospective analysis of subaxial subluxation after atlanto-axial arthrodesis in patients with rheumatoid arthritis based on annual radiographs obtained for 5 years. Clin Spine Surg 30:E598. https://doi.org/10.1097/BSD.0000000000000277
MacDowall A, Skeppholm M, Robinson Y, Olerud C (2017) Validation of the visual analog scale in the cervical spine. J Neurosurg Spine 28:227–235. https://doi.org/10.3171/2017.5.SPINE1732
Casey AT, Crockard HA, Stevens J (1997) Vertical translocation. Part II. Outcomes after surgical treatment of rheumatoid cervical myelopathy. J Neurosurg 87:863–869. https://doi.org/10.3171/jns.1997.87.6.0863
Alfieri A, Jho H-D, Tschabitscher M (2002) Endoscopic endonasal approach to the ventral cranio-cervical junction: anatomical study. Acta Neurochir (Wien) 144:219–225. https://doi.org/10.1007/s007010200029
Visocchi M, Signorelli F, Liao C, Rigante M, Ciappetta P, Barbagallo G, Olivi A (2019) Transoral versus transnasal approach for craniovertebral junction pathologies: which route is better? Acta Neurochir Suppl 125:181–186. https://doi.org/10.1007/978-3-319-62515-7_27
Iacoangeli M, Nasi D, Colasanti R, Pan B, Re M, Di Rienzo A, di Somma L, Dobran M, Specchia N, Scerrati M (2017) endoscopic endonasal odontoidectomy with anterior C1 arch preservation in rheumatoid arthritis: long-term follow-up and further technical improvement by anterior endoscopic C1–C2 screw fixation and fusion. World Neurosurg 107:820–829. https://doi.org/10.1016/j.wneu.2017.08.063
Morales-Valero SF, Serchi E, Zoli M, Mazzatenta D, Van Gompel JJ (2015) Endoscopic endonasal approach for craniovertebral junction pathology: a review of the literature. Neurosurg Focus 38:E15. https://doi.org/10.3171/2015.1.FOCUS14831
Dasenbrock HH, Clarke MJ, Bydon A, Sciubba DM, Witham TF, Gokaslan ZL, Wolinsky J-P (2012) Endoscopic image-guided transcervical odontoidectomy: outcomes of 15 patients with basilar invagination. Neurosurgery 70:351–359. https://doi.org/10.1227/NEU.0b013e318230e59a (discussion 359-360)
Jha RT, Dietz N, Dowlati E, Sandhu F (2020) Placement of C1 lateral mass screw—alternative technique: 2-dimensional operative video. Oper Neurosurg (Hagerstown). https://doi.org/10.1093/ons/opz418
Oseni A, Kakavas G, Scholz M, Petridis A (2016) Resolution of a periodontoid rheumatoid pannus mass in an elderly patient treated with a rigid cervical collar: a case report and literature review. S Afr Med J 106:687–688. https://doi.org/10.7196/SAMJ.2016.v106i7.9861
Miyamoto H, Sumi M, Uno K (2013) Outcome of surgery for rheumatoid cervical spine at one institute over three decades. Spine J 13:1477–1484. https://doi.org/10.1016/j.spinee.2013.05.023
Park J-H, Hong JT, Lee JB, Kim IS (2019) Clinical analysis of radiologic measurements in patients with basilar invagination. World Neurosurg 131:e108–e115. https://doi.org/10.1016/j.wneu.2019.07.080
Sorimachi Y, Iizuka H, Ara T, Nishinome M, Iizuka Y, Nakajima T, Takagishi K (2011) Atlanto-axial joint of atlanto-axial subluxation patients due to rheumatoid arthritis before and after surgery: morphological evaluation using CT reconstruction. Eur Spine J 20:798–803. https://doi.org/10.1007/s00586-010-1611-7
Uei H, Tokuhashi Y, Maseda M (2018) Radiographic and clinical outcomes of C1–C2 intra-articular screw fixation in patients with atlantoaxial subluxation. J Orthop Surg Res 13:273. https://doi.org/10.1186/s13018-018-0985-9
Vanek P, Bradac O, de Lacy P, Pavelka K, Votavova M, Benes V (2017) Treatment of atlanto-axial subluxation secondary to rheumatoid arthritis by short segment stabilization with polyaxial screws. Acta Neurochir (Wien) 159:1791–1801. https://doi.org/10.1007/s00701-017-3274-1
Janssen I, Nouri A, Tessitore E, Meyer B (2020) Cervical myelopathy in patients suffering from rheumatoid arthritis-a case series of 9 patients and a review of the literature. J Clin Med. https://doi.org/10.3390/jcm9030811
Ryu JI, Bak KH, Kim JM, Chun H-J (2017) Comparison of transarticular screw fixation and C1 lateral mass-C2 pedicle screw fixation in patients with rheumatoid arthritis with atlantoaxial instability. World Neurosurg 99:179–185. https://doi.org/10.1016/j.wneu.2016.12.028
Kurogochi D, Takahashi J, Uehara M, Ikegami S, Kuraishi S, Futatsugi T, Oba H, Takizawa T, Munakata R, Hatakenaka T, Koseki M, Kato H (2019) Ten-year results of reconstruction for rheumatoid cervical spine lesions and occurrence factor of subaxial subluxation. Asian Spine J 13:730–737. https://doi.org/10.31616/asj.2018.0343
Bhatia R, Haliasos N, Vergara P, Anderson C, Casey A (2014) The surgical management of the rheumatoid spine: has the evolution of surgical intervention changed outcomes? J Craniovertebr Junction Spine 5:38–43. https://doi.org/10.4103/0974-8237.135221
Clarke MJ, Cohen-Gadol AA, Ebersold MJ, Cabanela ME (2006) Long-term incidence of subaxial cervical spine instability following cervical arthrodesis surgery in patients with rheumatoid arthritis. Surg Neurol 66:136–140. https://doi.org/10.1016/j.surneu.2005.12.037
Werle S, Ezzati A, ElSaghir H, Boehm H (2013) Is inclusion of the occiput necessary in fusion for C1–2 instability in rheumatoid arthritis? J Neurosurg Spine 18:50–56. https://doi.org/10.3171/2012.10.SPINE12710
Yoshida G, Kamiya M, Yukawa Y, Kanemura T, Imagama S, Matsuyama Y, Ishiguro N (2012) Rheumatoid vertical and subaxial subluxation can be prevented by atlantoaxial posterior screw fixation. Eur Spine J 21:2498–2505. https://doi.org/10.1007/s00586-012-2444-3
Nagaria J, Kelleher MO, McEvoy L, Edwards R, Kamel MH, Bolger C (2009) C1–C2 transarticular screw fixation for atlantoaxial instability due to rheumatoid arthritis: a seven-year analysis of outcome. Spine 34:2880–2885. https://doi.org/10.1097/BRS.0b013e3181b4e218
Ito H, Neo M, Sakamoto T, Fujibayashi S, Yoshitomi H, Nakamura T (2009) Subaxial subluxation after atlantoaxial transarticular screw fixation in rheumatoid patients. Eur Spine J 18:869–876. https://doi.org/10.1007/s00586-009-0945-5
Ishii K, Matsumoto M, Takahashi Y, Okada E, Watanabe K, Tsuji T, Takaishi H, Nakamura M, Toyama Y, Chiba K (2010) Risk factors for development of subaxial subluxations following atlantoaxial arthrodesis for atlantoaxial subluxations in rheumatoid arthritis. Spine 35:1551–1555. https://doi.org/10.1097/BRS.0b013e3181af0d85
Mukai Y, Hosono N, Sakaura H, Ishii T, Fuchiya T, Fijiwara K, Fuji T, Yoshikawa H (2004) Laminoplasty for cervical myelopathy caused by subaxial lesions in rheumatoid arthritis. J Neurosurg 100:7–12. https://doi.org/10.3171/spi.2004.100.1.0007
Iizuka H, Iizuka Y, Mieda T, Tsunoda D, Kobayashi R, Sorimachi Y (2017) The clinical outcomes of atlanto-axial arthrodesis in patients with rheumatoid arthritis–Assessment according to the Japanese orthopaedic association cervical myelopathy evaluation questionnaire (JOACMEQ). J Orthop Sci 22:401–404. https://doi.org/10.1016/j.jos.2017.01.016
Yoshimoto H, Ito M, Abumi K, Kotani Y, Shono Y, Takada T, Minami A (2004) A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1–C2 fusion. Spine 29:175–181. https://doi.org/10.1097/01.BRS.0000107225.97653.CA
Ronkainen A, Niskanen M, Auvinen A, Aalto J, Luosujärvi R (2006) Cervical spine surgery in patients with rheumatoid arthritis: longterm mortality and its determinants. J Rheumatol 33:517–522
Smolen JS, Breedveld FC, Burmester GR, Bykerk V, Dougados M, Emery P, Kvien TK, Navarro-Compán MV, Oliver S, Schoels M, Scholte-Voshaar M, Stamm T, Stoffer M, Takeuchi T, Aletaha D, Andreu JL, Aringer M, Bergman M, Betteridge N, Bijlsma H, Burkhardt H, Cardiel M, Combe B, Durez P, Fonseca JE, Gibofsky A, Gomez-Reino JJ, Graninger W, Hannonen P, Haraoui B, Kouloumas M, Landewe R, Martin-Mola E, Nash P, Ostergaard M, Östör A, Richards P, Sokka-Isler T, Thorne C, Tzioufas AG, van Vollenhoven R, de Wit M, van der Heijde D (2016) Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis 75:3–15. https://doi.org/10.1136/annrheumdis-2015-207524
Naranjo A, Carmona L, Gavrila D, Balsa A, Belmonte MA, Tena X, Rodríguez-Lozano C, Sanmartí R, González-Alvaro I, EMECAR Study Group (2004) Prevalence and associated factors of anterior atlantoaxial luxation in a nation-wide sample of rheumatoid arthritis patients. Clin Exp Rheumatol 22:427–432
Funding
Open access funding provided by HEAL-Link Greece. None.
Author information
Authors and Affiliations
Contributions
TS: Data curation, Investigation, Writing—original draft, Writing–review & editing. CT: Data curation, Investigation, Writing—original draft, Writing–review & editing. AZ: Data curation, Writing—original draft, Writing–review & editing. GAA: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing—original draft, Writing–review & editing. SV: Data curation, Methodology, Supervision. MIA: Formal analysis, Methodology, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Siempis, T., Tsakiris, C., Anastasia, Z. et al. Radiological assessment and surgical management of cervical spine involvement in patients with rheumatoid arthritis. Rheumatol Int 43, 195–208 (2023). https://doi.org/10.1007/s00296-022-05239-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05239-5