Abstract
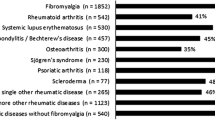
There is an ongoing debate about the importance and the extent to which psychological and psychopathological factors, adverse childhood experiences, and socio-demographic characteristics are associated with the development of certain types of rheumatic disease. With the aim of contributing to knowledge on the subject, the present study uses machine learning modeling to determine the importance of 20 psychological and social variables in predicting two classes of rheumatic disease: inflammatory rheumatic and musculoskeletal diseases (RMD) (rheumatoid arthritis = RA, spondyloarthritis = SA, and Sjögren’s syndrome = SS) versus non-inflammatory RMD, namely fibromyalgia = FM). A total of 165 French women with FM, RA, SA, and SS completed an inventory of personality traits, a psychopathology diagnosis questionnaire, and a fatigue/pain questionnaire. They also answered questions about adverse childhood experiences and socio-demographic characteristics. Random forest and logistic regression machine learning algorithms were used for data analysis. The main findings suggest that mistreatment during childhood ((MDA = 10.22), the agreeableness personality trait (MDA = 3.39), and somatic disorder (MDA = 3.25) are the main psychological and social predictors of the type of rheumatic disease diagnosed. The first two predictors (OR = 18.92 and OR = 6.11) are also more strongly associated with FM than with RA-SA-SS. Overall, adverse childhood experiences seem relatively more important than personality traits, psychopathological or demographic variables. The results of this study suggest that traumatic childhood experiences may lead to psychopathological disorders in adulthood, which in turn might underlie, at least in part, the development of FM. Since there are no imaging or biological markers of FM, the present findings contribute to the scientific literature offering information to help patients with FM understand their pathology. They may also provide physicians with more diagnostic information.



Similar content being viewed by others
Availability of data and material
Following the Ethic Committee recommendation, the data used in this study cannot be shared through public open repositories. However, researchers willing to access the data can make the request to the corresponding author.
Code availability
Researchers willing to access the data analysis R code can make the request to the corresponding author.
Notes
We included menopause in socio-demographic predictors because we did not have a more appropriate category in this study for this biological and psychosocial status.
The inflammatory RMD group includes patients with RA, SA or SS, whose diagnosis was based on clinician expertise and were included in the study when they met the classification criteria. The diagnosis of FM was also primarily based on clinician expertise, implying that inflammatory RMD had been ruled out. It must be noted that some patients from in the RA-SA-SS group may present with FM features, as reported in the literature as secondary FM.
Abbreviations
- RMD:
-
Rheumatic and musculoskeletal diseases
- RA:
-
Rheumatoid arthritis
- SA:
-
Spondyloarthritis
- SS:
-
Sjögren’s syndrome
- FM:
-
Fibromyalgia
- ACR:
-
American College of Rheumatology
- FIRST:
-
Fibromyalgia rapid screening tool
- ASAS:
-
Assessment of SpondyloArthritis international Society
- BFI:
-
Big five inventory
- MDA:
-
Mean decrease accuracy
- OR:
-
Odds ratio
References
World Health Organization (2021). Chronic rheumatic conditions. Geneva: WHO. Available from: https://www.who.int/chp/topics/rheumatic/en/. Accessed 10 Feb 2021
American College of Rheumatology (2021). Diseases and conditions. Washington DC: ACR. Available from: https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions. Accessed 11 Feb 2021
Hauser W, Fitzcharles M (2018) Facts and myths pertaining to fibromyalgia. Dialogues Clin Neurosci 20(1):53–62. https://doi.org/10.31887/DCNS.2018.20.1/whauser
Inanici FF, Yunus MB (2004) History of fibromyalgia: past to present. Curr Pain Headache Rep 8:369–378. https://doi.org/10.1007/s11916-996-0010-6
Wolfe F, Smythe HA, Yunus MB, Bennett RM et al (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheumatol 33(2):160–172. https://doi.org/10.1002/art.1780330203
Bannwarth B, Blotman F, Roué-Le Lay K et al (2009) Fibromyalgia syndrome in the general population of France: a prevalence study. Joint Bone Spine 76:184–187. https://doi.org/10.1016/j.jbspin.2008.06.002
Spitzer C, Wegert S, Wollenhaupt J, Wingenfeld K et al (2013) Gender-specific association between childhood trauma and rheumatoid arthritis: a case-control study. J Psychosom Res 74(4):296–300. https://doi.org/10.1016/j.jpsychores.2012.10.007
Walker EA, Keegan D, Gardner G, Sullivan M et al (1997) Psychosocial factors in fibromyalgia compared with rheumatoid arthritis: II. Sexual, physical, and emotional abuse and neglect. Psychosom Med 59(6):572–577. https://doi.org/10.1097/00006842-199711000-00003
Varinen A, Kosunen E, Mattila K, Koskela T et al (2017) The relationship between childhood adversities and fibromyalgia in the general population. J Psychosom Res 99:137–142. https://doi.org/10.1016/j.jpsychores.2017.06.011
Ottenhoff JSE, Kortlever JTP, Boersma EZ, Laverty DC et al (2019) Adverse childhood experiences are not associated with patient-reported outcome measures in patients with musculoskeletal illness. Clin Orthop Relat Res 477(1):219–228. https://doi.org/10.1097/CORR.0000000000000519
Gonzalez B, Baptista TM, Branco JC et al (2015) Fibromyalgia characterization in a psychosocial approach. Psychol Health Med 20:363–368. https://doi.org/10.1080/13548506.2014.931590
Johannsonn V (1993) Does a fibromyalgia personality exist? J Musculoskelet Pain 1:245–252. https://doi.org/10.1300/J094v01n03_26
Seto A, Han X, Price LL, Harvey WF et al (2019) The role of personality in patients with fibromyalgia. J Clin Rheumatol 38(1):149–157. https://doi.org/10.1007/s10067-018-4316-7
Vural M, Berkol TD, Erdogdu Z et al (2014) Evaluation of personality profile in patients with fibromyalgia syndrome and healthy controls. Mod Rheumatol 24:823–828. https://doi.org/10.3109/14397595.2013.868069
Bucourt E, Martaillé V, Mullemanb D, Goupille P et al (2017) Comparison of the Big Five personality traits in fibromyalgia and other rheumatic diseases. Joint Bone Spine 84:203–207. https://doi.org/10.1016/j.jbspin.2016.03.006
Gencay-Can A, Can S (2012) Temperament and character profile of patients with fibromyalgia. Rheumatol Int 32:3957. https://doi.org/10.1007/s00296-011-2324-x
Garcia-Fontanals A, García-Blanco S, Portell M et al (2014) Cloninger’s psychobiological model of personality and psychological distress in fibromyalgia. Int J Rheum Dis 19(9):852–863. https://doi.org/10.1111/1756-185X.12473
Cronan TA, Serber ER, Walen H, Jaffe M (2002) The influence of age on fibromyalgia symptoms. J Aging Health. https://doi.org/10.1177/08964302014003004
Lu K, Wang H-K, Yen C-C, Huang CY et al (2014) Association between autoimmune rheumatic diseases and the risk of dementia. Biomed Res Int 2014:861812. https://doi.org/10.1155/2014/861812
López-Castillo CA, Calderón-Rojas R, Amaya-Amayab J, DeSanVicente-Célis Z et al (2014) Impact of educational level on rheumatoid arthritis: a systematic review. Revista Colombiana de Reumatología 21(4):201–212. https://doi.org/10.1016/j.rcreu.2014.09.002
Eun Y, Jeon KH, Han K, Kim D et al (2020) Menopausal factors and risk of seropositive rheumatoid arthritis in postmenopausal women: a nationwide cohort study of 136 million women. Sci Rep 10(1):20793. https://doi.org/10.1038/s41598-020-77841-1
Nichols JA, Chan HWH, Baker MAB (2019) Machine learning: applications of artificial intelligence to imaging and diagnosis. Biophys Rev 11(1):111–118. https://doi.org/10.1007/s12551-018-0449-9
Perrot S, Bouhassira D, Fermanian J (2010) Development and validation of the fibromyalgia rapid screening tool (FiRST). Pain 150(2):250–256. https://doi.org/10.1016/j.pain.2010.03.034
Arnett FC, Edworthy SM, Bloch DA et al (1998) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheumatol 31(3):315–324. https://doi.org/10.1002/art.1780310302
Rudwaleit M, Landewe R, van der Heijde D et al (2009) The development of Assessment of SpondyloArthritis International Society Classification criteria for axial SpondyloArthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis 68(6):770–776. https://doi.org/10.1136/ard.2009.108217
Vitali C, Bombardieri S, Jonsson R et al (2002) Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 61(6):554–558. https://doi.org/10.1136/ard.61.6.554
Plaisant O, Courtois R, Réveillère C et al (2010) Validation par analyse factorielle du Big Five Inventory franc¸ ais (BFI-Fr). Analyse convergente avec le NEO-PI-R. Ann Med Psychol 168:97–106. https://doi.org/10.1016/j.amp.2009.09.003
Pariente PD, Challita H, Mesbah M, Guelfi JD (1992) The GHQ-28 questionnaire in French: a validation survey in a panel of 158 general psychiatric patients. Eur Psychiatry 7(1):15–20. https://doi.org/10.1017/S0924933800002455
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale. Arch Neurol 46:1121–1123. https://doi.org/10.1001/archneur.1989.00520460115022
Ferreri M, Vacher J, Tawil S, Alby JM (1987) Facteurs événementiels et dépression : le questionnaire EVE, une nouvelle approche de méthodologie prédictive. Psychologie médicale 19(13):2441–2448
Breiman L (2001) Random forests. Mach Learn 45:5–32. https://doi.org/10.1023/A:1010933404324
Kaleycheva N, Cullen A, Evans R, Harris T, Nicholson T, Chalder T (2021) The role of lifetime stressors in adult fibromyalgia: systematic review and meta-analysis of case-control studies. Psychol Med 51(2):177–193. https://doi.org/10.1017/S0033291720004547
Arnold LM (2010) The pathophysiology, diagnosis and treatment of fibromyalgia. Psychiatr Clin 33(2):375–408. https://doi.org/10.1016/j.psc.2010.01.001
Smith BW, Papp ZZ, Tooley EM, Montague EQ, Robinson AE, Cosper CJ (2010) Traumatic events, perceived stress and health in women with fibromyalgia and healthy controls. Stress Health 26(1):83–93. https://doi.org/10.1002/smi.126
Tuscic SJ, Flander GB, Matešković D (2013) The consequences of childhood abuse. Paediatr Today 9(1):24–35. https://doi.org/10.5457/p2005-114.58
Novo R, Gonzalez B, Peres R, Aguiar P (2017) A meta-analysis of studies with the Minnesota multiphasic personality inventory in fibromyalgia patients. Personality Individ Differ 116:96–108. https://doi.org/10.1016/j.paid.2017.04.026
Torres X, Bailles E, Valdes M, Gutierrez F, Peri J-M, Arias A, Gomez E, Collado A (2013) Personality does not distinguish people with fibromyalgia but identifies subgroups of patients. Gen Hosp Psychiatry 35(6):640–648. https://doi.org/10.1016/j.genhosppsych.2013.07.014
Acknowledgements
We are grateful to all the rheumatic patients who took part in this study, the team who worked in this research, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, receptionists and nurses. Particularly, we would like to thank Dr. Odile Plaisant, Professor Pierre Bourgeois and Professor Bruno Fautrel (Assistance Publique – Hôpitaux de Paris, University Hospital of Pitié-Salpêtrière), Dr. Stephanie Rist and Dr. Carine Salliot (Regional Hospital of Orleans) for their involvement in selecting the patients and the quality of data collection. In addition, the authors thank Agnès Caille and Bruno Giraudeau (CIC Inserm 1415, University Hospital of Tours) for providing their advice.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
GVC carried out data/statistical analysis and drafted the manuscript. EB collected the data. EB, RC, and CR conceived the study and initiated the scientific collaboration between the groups. VM, IJV, PG, and DM recruited the participants, performed the rheumatology diagnosis, and provided patient information. EB, DM, and RC edited the manuscript, with EB and DM providing meticulous revisions. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors are full-time employees at their indicated affiliation institutions, which are public universities and hospitals. None of the authors received fees, bonuses or other benefits for the work described in the manuscript.
Ethical approval
Ethical clearance was obtained from the ethical committee of the University of Tours. All participants provided written informed consent for data collection and publication prior to data collection. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vera Cruz, G., Bucourt, E., Réveillère, C. et al. Machine learning reveals the most important psychological and social variables predicting the differential diagnosis of rheumatic and musculoskeletal diseases. Rheumatol Int 42, 1053–1062 (2022). https://doi.org/10.1007/s00296-021-04916-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-04916-1