Abstract
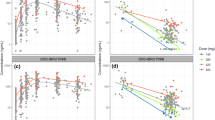
Belinostat was approved in 2014 for the treatment of relapsed or refractory peripheral T-cell lymphoma, however, there was insufficient data to recommend a dose in patients with moderate to severe hepatic impairment. The purpose of this analysis was to characterize the pharmacokinetic disposition of belinostat and its five metabolites in patients with advanced cancers and varying degrees of liver dysfunction. A population pharmacokinetic model was therefore developed to describe the parent-metabolite system. The final model was then implemented to assess the effect of liver impairment on each metabolic pathway of belinostat. It was determined that significant pharmacokinetic differences could only be demonstrated in patients with severe hepatic impairment. The final model estimated a 35%–47% reduction in metabolic clearance attributed to UGT1A1/2B7 glucuronidation, CYP2A6/3A4/2C9 metabolism, and β-oxidation. These hepatic impairment effects reduced between-subject variability by only 5%–8% for their respective parameter, with a large amount of remaining unexplained variability. With further validation, this model can be leveraged to assess the need for dose adjustments in this patient population.





Similar content being viewed by others
Data availability
The datasets used for this analysis are available upon reasonable request from the corresponding author after permission of the sponsor.
References
Gimsing P, Hansen M, Knudsen LM et al (2008) A phase I clinical trial of the histone deacetylase inhibitor belinostat in patients with advanced hematological neoplasia. Eur J Haematol 81(3):170–176
Mackay HJ, Hirte H, Colgan T et al (2010) Phase II trial of the histone deacetylase inhibitor belinostat in women with platinum resistant epithelial ovarian cancer and micropapillary (LMP) ovarian tumours. Eur J Cancer 46(9):1573–1579
Steele NL, Plumb JA, Vidal L et al (2008) A phase 1 pharmacokinetic and pharmacodynamic study of the histone deacetylase inhibitor belinostat in patients with advanced solid tumors. Clin Cancer Res 14(3):804–810
2017 Product Information: BELEODAQ(R) intravenous injection, belinostat intravenous injection. Spectrum Pharmaceuticals, Inc. (per FDA), Irvine, CA
Calvo E, Reddy G, Boni V et al (2016) Pharmacokinetics, metabolism, and excretion of (14)C-labeled belinostat in patients with recurrent or progressive malignancies. Invest New Drugs 34(2):193–201
Bailey H, McPherson JP, Bailey EB et al (2016) A phase I study to determine the pharmacokinetics and urinary excretion of belinostat and metabolites in patients with advanced solid tumors. Cancer Chemother Pharmacol 78(5):1059–1071
El-Khateeb E, Achour B, Al-Majdoub ZM, Barber J, Rostami-Hodjegan A (2021) Non-uniformity of changes in drug-metabolizing enzymes and transporters in liver cirrhosis: implications for drug dosage adjustment. Mol Pharm 18(9):3563–3577
Elbekai RH, Korashy HM, El-Kadi AO (2004) The effect of liver cirrhosis on the regulation and expression of drug metabolizing enzymes. Curr Drug Metab 5(2):157–167
Hoyumpa AM, Schenker S (1991) Is glucuronidation truly preserved in patients with liver disease? Hepatology 13(4):786–795
Patel H, Egorin MJ, Remick SC et al (2004) Comparison of child-pugh (CP) criteria and NCI organ dysfunction working group (NCI-ODWG) criteria for hepatic dysfunction (HD): implications for chemotherapy dosing. J Clin Oncol 22:6051
Elmeliegy M, Yang DZ, Salama E, Parivar K, Wang DD (2021) Discordance between child-pugh and national cancer institute classifications for hepatic dysfunction: implications on dosing recommendations for oncology compounds. J Clin Pharmacol 61:105–115
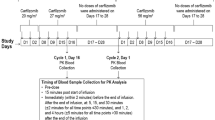
Takebe N, Beumer JH, Kummar S et al (2019) A phase I pharmacokinetic study of belinostat in patients with advanced cancers and varying degrees of liver dysfunction. Br J Clin Pharmacol 85(11):2499–2511
Kiesel BF, Parise RA, Tjørnelund J et al (2013) LC-MS/MS assay for the quantitation of the HDAC inhibitor belinostat and five major metabolites in human plasma. J Pharm Biomed Anal 81–82:89–98
Acknowledgements
This study was supported by the following grants: UM1 CA186690, U24CA247643, R50CA211241, and P30CA47904 (NCI).
Author information
Authors and Affiliations
Contributions
A.D. performed the analysis and wrote the main manuscript text. All authors reviewed the manuscript and provided valuable domain expertise that influenced the research conducted.
Corresponding author
Ethics declarations
Conflict OF Interest
J.G. is a co-founder of Pumas AI, the company that developed the software, Pumas, which was used to develop the population PK model.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The data was generated in trials registered under ClinicalTrials.gov Identifier NCT01273155.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dunn, A., Takebe, N., Chen, A. et al. The effect of liver dysfunction on the pharmacokinetic disposition of belinostat and its five metabolites in patients with advanced cancers. Cancer Chemother Pharmacol (2024). https://doi.org/10.1007/s00280-024-04651-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00280-024-04651-x