Abstract
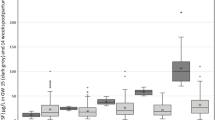
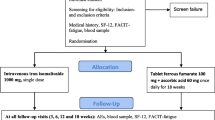
This study aims to evaluate iron prophylaxis in pregnant women from the individual aspect, i.e. according to serum ferritin levels at the beginning of pregnancy, and to assess which dose of iron would be adequate to prevent iron deficiency (ID) and iron deficiency anaemia (IDA) during pregnancy and postpartum. A randomised, double-blind study comprising 301 healthy Danish pregnant women allocated into four groups taking ferrous iron (as fumarate) in doses of 20 mg (n=74), 40 mg (n=76), 60 mg (n=77) and 80 mg (n=75) from 18 weeks gestation (inclusion) to 8 weeks postpartum. Iron status markers [serum ferritin, serum soluble transferrin receptor (sTfR), haemoglobin] were recorded at 18, 32 and 39 weeks gestation and 8 weeks postpartum. Body iron was calculated using the serum sTfR/serum ferritin ratio. ID was defined by serum ferritin <12 μg/l in pregnancy and <15 μg/l postpartum; IDA as serum ferritin <12 μg/l and haemoglobin <5th percentile in iron-replete pregnant women. Women in the iron supplement groups were stratified according to serum ferritin levels at inclusion; 50.7% had ferritin ≤30 μg/l, 37.7% ferritin 30–70 μg/l and 11.6% ferritin >70 μg/l. At 32 weeks, women with ferritin ≤30 μg/l had an ID frequency of: 20-mg group 54.1%, 40 mg 29.7%, 60 mg 24.4%, 80 mg 20.6% (p<0.001); women with ferritin >30 μg/l had an ID frequency of: 20-mg group 20.0%, 40 mg 13.9%, 60 mg 5.7%, 80 mg 5.1% (p<0.001). Women with ferritin >70 μg/l had no ID. Postpartum, ID was found in 4.7% in 20-mg group, 2.9% in group 40 mg and 0% in group 60 and 80 mg. IDA: At 32 weeks, women with ferritin ≤30 μg/l had an IDA frequency of: 20-mg group 2.7%, 40 mg 2.7%, 60 and 80 mg 0%; none of the women with ferritin >30 μg/l displayed IDA. Body iron at 18 weeks was 10.4 mg/kg, similar in the four iron groups. Later in pregnancy body iron declined significantly, being lower the 20 mg group, and similar in the 40, 60 and 80-mg groups. Postpartum body iron rose to inclusion levels being 9.3 mg/kg in the 20-mg group and 10.5 mg/kg in the 40-, 60- and 80-mg groups. This study gives an estimate of iron dosage in individual iron prophylaxis adjusted to serum ferritin levels in early pregnancy. In the prevention of ID, we suggest 80–100 mg ferrous iron/day to women having ferritin ≤30 μg/l and 40 mg ferrous iron/day to women having ferritin 31–70 μg/l. In the prevention of IDA, we suggest 40 mg ferrous iron/day to women having ferritin ≤70 μg/l. Women with ferritin >70 μg/l have no need for iron supplement.

Similar content being viewed by others
References
Bothwell TH (200) Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr 72(suppl 1):257S–264S
Milman N, Bergholt T, Byg K-E, Eriksen L, Graudal N (1999) Iron status and iron balance during pregnancy. A critical reappraisal of iron supplementation. Acta Obstet Gynecol Scand 78:749–757
van den Broek NR, Letsky EA, White SA, Shenkin A (1998) Iron status in pregnant women: which measurements are valid? Br J Haematol 103:817–824
Milman N (1996) Serum ferritin in Danes: studies of iron status from infancy to old age, during blood donation and pregnancy. Int J Hematol 63:103–135
Nordic Council of Ministers (2004) Nordic nutrition recommendations 2004, 4th edn. Nord, Copenhagen, pp 364–366
US Preventive Services Task Force (1993) Routine iron supplementation during pregnancy. Policy statement. Review article. JAMA 270:2846–2854
Milman N, Agger OA, Nielsen OJ (1991) Iron supplementation during pregnancy. Effect on iron status markers, serum erythropoietin and human placental lactogen. A placebo-controlled study in 207 Danish women. Dan Med Bull 38:471–476
Milman N, Byg K-E, Graudal N, Agger AO (2000) Reference values for hemoglobin and erythrocyte indices during normal pregnancy in 206 women with and without iron supplementation. Acta Obstet Gynecol Scand 78:89–98
Milman N, Clausen J, Byg K-E (1998) Iron status in 268 Danish women aged 18–30 years. Influence of menstruation, method of contraception, and iron supplementation. Ann Hematol 76:13–19
Institute of Medicine, Food and Nutrition Board (1993) Iron deficiency anemia: recommended guidelines for the prevention, detection, and management among US children and women of childbearing age. National Academy, Washington, District of Columbia
Haram K, Hervig T, Ulvik R (1997) New aspects on preventive iron supplementation in normal pregnancy. Tidsskr Nor Laegeforen 117:966–969
Milman N, Bergholt T, Eriksen, L, Byg K-E, Graudal N, Pedersen P, Hertz J (2005) Iron prophylaxis during pregnancy—how much iron is needed? A randomised dose response study of 20 to 80 mg ferrous iron daily to pregnant women. Acta Obstet Gynecol Scand 84:238–247
Cook JD, Flowers CH, Skikne BS (2003) The quantitative assessment of body iron. Blood 101:3359–3364
Milman N, Juul-Jørgensen B, Bentzon MW (1997) Calibration of the Abbott AxSYM Ferritin kit using the WHO Human Liver Ferritin International Standard 80/602. Clin Chem 35:631–632
Cook JD, Skikne B (1989) Iron deficiency: definition and diagnosis. J Intern Med 226:349–355
Worwood M (1994) Laboratory determination of iron status. In Brock, JH, Halliday JW, Pippard MJ, Powell LW (eds) Iron metabolism in health and disease. WB Saunders, London, pp 449–476
Milman N, Pedersen NS, Visfeldt J (1983) Serum ferritin in healthy Danes: relation to marrow haemosiderin iron stores. Dan Med Bull 30:115–120
Wright RO, Shannon MW, Wright RJ, Hu H (2000) Association between iron deficiency and low-level lead poisoning in an urban primary care clinic. Am J Public Health 89:1049–1053
Akesson A, Berglund M, Schutz A, Bjellerup P, Bremme K, Vahter M (2002) Cadmium exposure in pregnancy and lactation in relation to iron status. Am J Public Health 92:284–287
Skikne B, Baynes RD (1994) Iron absorption. In Brock JH, Halliday JW, Pippard MJ, Powell LW (eds) Iron metabolism in health and disease. Saunders, London, pp 151–187
Rossander-Hultén L, Brune M, Sandström B, Lönnerdal B, Hallberg L (1991) Competitive inhibition of iron absorption by manganese and zinc in humans. Am J Clin Nutr 54:152–156
Lund EK, Wharf SG, Fairweather-Tait SJ, Johnson IT (1999) Oral ferrous sulfate supplements increase the free radical-generating capacity of feces from healthy volunteers. Am J Clin Nutr 69:250–255
Taylor DJ, Mallen C, McDougall N, Lind T (1982) Effect of iron supplementation on serum ferritin levels during and after pregnancy. Br J Obstet Gynaecol 89:1011–1017
Galan P, Wainer R, De Benaze C, Hercberg S (1990) Prevention de l’anemie ferriprive au cours de la grossesse: effet de la supplementation precoce en fer. In: Hercberg S, Galan P, Dupin H (eds) Recent knowledge on iron and folate deficiencies in the World. INSERM, Paris, 615–621
Eskeland E, Malterud K, Ulvik RJ, Hunskaar S (1997) Iron supplementation in pregnancy: is less enough? Acta Obstet Gynecol Scand 76:822–828
Makrides M, Crowther CA, Gibson RA, Gibson RS, Skeaff CM (2003) Efficacy and tolerability of low-dose iron supplements during pregnancy: a randomized controlled trial. Am J Clin Nutr 78:145–153
Byg K-E, Milman N, Agger AO (2000) Correlations between iron status markers during normal pregnancy in women with and without iron supplementation. Hematology 4:529–539
Thompson WG (1988) Comparison of tests for diagnosis of iron depletion in pregnancy. Am J Obstet Gynecol 5:1132–1134
van den Broek NR, Letsky EA, White SA, Shenkin A (1998) Iron status in pregnant women: which measurements are valid? Br J Haematol 103:817–824
Carriage MT, Skikne S, Finley B, Cutler B, Cook JD (1991) Serum transferrin receptor for the detection of iron deficiency. Am J Clin Nutr 54:107–181
Akesson A, Bjellerup P, Berglund M, Bremme K, Vahter M (1998) Serum transferrin receptor: a specific marker of iron deficiency in pregnancy. Am J Clin Nutr 68:1241–1246
Milman N, Clausen J, Byg K-E (1998) Iron status in 268 Danish women aged 18–30 years: influence of menstruation, contraceptive method, and iron supplementation. Ann Hematol 76:13–19
Danish National Board of Health (1992) Recommendations about iron supplementation during pregnancy. Ugeskr Laeger 154:3445
Milman N (2006) Iron and pregnancy—a delicate balance. Ann Hematol May 12 (Epub ahead of print)
Nokes C, van den Bosch C, Bundy D (1998) The effects of iron deficiency and anemia on mental and motor performance, educational achievement, and behavior in children. A report of the INACG. International Life Sciences Institute, Washington, DC
Lozoff B (2000) Perinatal iron deficiency and the developing brain. Pediatr Res 48:137–139
Grantham-McGregor S, Ani C (2001) A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr 131:649S–668S
Milman N, Pedersen P, Ovesen L, Melsen GV, Fenger K (2004) Frequency of the C282Y and H63D mutations of the haemochromatosis (HFE) gene in 2501 ethnic Danes. Ann Hematol 83:654–657
Acknowledgements
The study was supported by grants from Apotekerfonden and Den Lægevidenskabelige Forskningsfond ved Region 3. The authors appreciate the great help of the midwives at the Department of Obstetrics during the study and the enthusiasm of Chief Physician Robert Jordal† and the laboratory technicians at the Department of Clinical Biochemistry, Gentofte Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milman, N., Byg, KE., Bergholt, T. et al. Body iron and individual iron prophylaxis in pregnancy—should the iron dose be adjusted according to serum ferritin?. Ann Hematol 85, 567–573 (2006). https://doi.org/10.1007/s00277-006-0141-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-006-0141-1