Abstract
Background
The aim of this study was to elucidate the anatomical structures of supporting system of the infraorbital area.
Materials and methods
Forty-four hemifaces from eleven Korean and eleven Thai cadavers were used to dissect the infraorbital area. Based on the dissection and previous histologic results, they were analyzed.
Results
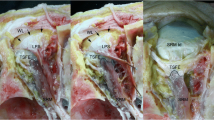
The orbicularis oculi muscle (OOc) had two portions (palpebral and orbital portion) and four subparts (pretarsal, preseptal, prezygomatic, and premaxillary part). The elliptical muscle fiber of OOc was supported by circumferential connective tissue including skin ligament, orbicularis retaining ligament, zygomatic ligament, and zygomatic cutaneous ligament. The vertical muscle fiber, the tear trough muscle fiber, and medial muscular band directly attached to the skin.
Conclusion
Full of subcutaneous tissue in the tear trough groove, strong attachment to the bone by tear trough ligament and to the skin by tear trough muscle fiber would multiply result in the tear trough on the face.







Similar content being viewed by others
Data availability
Data are available on request to corresponding author.
References
Davison SP, Irio M, Oh C (2015) Transconjunctival lower lid blepharoplasty with and without fat repositioning. Clin Plast Surg 42(1):51–56
Massry GG, Hartstein ME (2012) The lift and fill lower blepharoplasty. Ophthal Plast Reconstr Surg 28(3):213–218
Sharad J (2012) Dermal fillers for the treatment of tear trough deformity: a review of anatomy, treatment techniques, and their outcomes. J Cutan Aesthet Surg 5(4):229–238
Yoo DB, Peng GL, Massry GG (2013) Transconjunctival lower blepharoplasty with fat repositioning: a retrospective comparison of transposing fat to the subperiosteal vs supraperiosteal planes. JAMA Facial Plast Surg 15(3):176–181
Youn S, Shin JI, Kim JT, Kim YH (2014) Transconjunctival subperiosteal fat reposition for tear trough deformity: pedicled fat redraping versus septal reset. Ann Plast Surg 73(5):479–484
Standring SBNRGH (2008) Gray’s anatomy : the anatomical basis of clinical practice, 15th edn. Churchill Livingstone/Elsevier, Edinburgh
Stuzin JM, Baker TJ, Gordon HL (1992) The relationship of the superficial and deep facial fascias: relevance to rhytidectomy and aging. Plast Reconstr Surg 89(3):441–449 (discussion 450-441)
Jiang J, Wang X, Chen R, Xia X, Sun S, Hu K (2016) Tear trough deformity: different types of anatomy and treatment options. Postepy Dermatol Alergol 33(4):303–308
Muzaffar AR, Mendelson BC, Adams WP Jr (2002) Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg 110(3):873–884 (discussion 897-911)
Park JT, Youn KH, Lee JG, Kwak HH, Hu KS, Kim HJ (2012) Medial muscular band of the orbicularis oculi muscle. J Craniofac Surg 23(1):195–197
Mendelson BC, Muzaffar AR, Adams WP Jr (2002) Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg 110(3):885–896 (discussion 897-911)
Kampan N, Akita K, Mahakkanukrauh P (2019) The malaris muscle concept reconsidered. Anat Cell Biol 52(2):134–139
Kampan N, Tsutsumi M, Okuda I, Nasu H, Hur MS, Yamaguchi K, Akita K (2018) The malaris muscle: its morphological significance for sustaining the intraorbital structures. Anat Sci Int 93(3):364–371
Wong CH, Hsieh MK, Mendelson B (2012) The tear trough ligament: anatomical basis for the tear trough deformity. Plast Reconstr Surg 129(6):1392–1402
Furnas DW (1989) The retaining ligaments of the cheek. Plast Reconstr Surg 83(1):11–16
Kaye BL (1981) The extended face-lift with ancillary procedures. Ann Plast Surg 6(5):335–346
Mendelson BC (1997) SMAS fixation to the facial skeleton: rationale and results. Plast Reconstr Surg 100(7):1834–1842 (discussion 1843-1835)
Stuzin JM, Baker TJ, Gordon HL, Baker TM (1995) Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg 22(2):295–311
Okuda I, Akita K, Komemushi T, Irimoto M, Nakajima Y (2021) Basic consideration for facial aging: analyses of the superficial musculoaponeurotic system based on anatomy. Aesthet Surg J 41(3):NP113–NP123
Acknowledgements
This study was conducted in compliance with the principles set forth in the Declaration of Helsinki. Consent was received from the families of the deceased patients before beginning the dissections. The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.
Funding
There is no financial disclosure to be declared.
Ethics declarations
Conflict of interest
The author acknowledges that the conflict of interest statement included in the “Author Guidelines” has been considered. The author hereby certifies that, to the best of his/her knowledge, no aspect of the current personal or professional situation might reasonably be expected to significantly affect the views on the subject being presented.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, SH., Yi, KH., Bae, JH. et al. A novel description of the supporting system of the orbicularis oculi muscle in the infraorbital area: Tear trough muscle fiber. Surg Radiol Anat 46, 3–9 (2024). https://doi.org/10.1007/s00276-023-03265-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03265-x