Abstract
Purposes
The present study was conducted to assess the amount of bone present between root apices and the maxillary sinus floor in the maxillary lateral region, to compare the evaluations on cone beam computed tomography (CBCT) and orthopantomography (OPG), and to evaluate the bone density of the same region using three-dimensional images on CBCT.
Methods
Fifty-one dental patients were recruited for the study. All subjects were partially edentulous. The distances from the maxillary premolars and molars apices to the maxillary sinus floor were assessed using CBCT and OPG. Color codes were assigned to the bone density of edentulous loci. Parametric and non-parametric tests were used for statistical analyses. A p value <0.05 was considered statistically significant.
Results
The maxillary first and second molars recorded the shortest mean distances to the sinus floor, in contrast to the maxillary first premolar. The bone density of the maxillary lateral area increased from the maxillary first premolar to the second molar. No statistical significant differences were found between the evaluated sites.
Conclusions
Our results provide estimates of the minimal and maximal distances between teeth and sinus, as well as the average bone density in the maxillary lateral region. It is important that evaluation of a specific patient be performed during the preoperative planning of implants.
Similar content being viewed by others
Introduction
The maxillary sinus, through its size and relationship with the upper lateral teeth, directly influences the ease of surgical access in this area. The topography of the inferior wall of the sinus, as related to the maxillary root apices, varies according to an individual’s age, size and degree of pneumatization of the sinus and dental status [14]. Positive correlations between length of root projections and the degree of pneumatization after extraction have been proven based on orthopantomograms (OPG) [26]. Thus, the available bone height for implant placement is reduced.
It has been suggested that the roots of the second molars (especially mesiobuccal roots) have the closest proximity to the sinus floor, followed by the first molars (mainly buccal roots), third molars, second premolars and first premolars [2].
Computer tomography (CT) scans with frontal, axial and cross-sectional views are helpful to precisely localize anatomical structures and pathological lesions, including defects in the maxillary sinus wall or membrane, bone quality and quantity, and the relationship of the maxilla with other anatomic structures. The three-dimensional (3D) images of cone beam computer tomography (CBCT) are helpful in assessing the relationship with the maxillary sinus and add valuable information for evaluation of periodontal defects [18].
In 1989, CT was introduced as helical computed tomography, being the last generation that produces bi-dimensional images of the body, as very thin slices. Unfortunately, the images were obtained with high-radiation dose [10]. CBCT or digital volume tomography (DVT) produces 3D reconstructions of individual teeth and the surrounding tissues using a single scan, thus the patient needs to remain absolutely still throughout the exposure. The X-ray penetration of the structure is cone-shaped and the capture is made by a flat standard detector [11, 17]. The utility of CBCT is enhanced by the sophisticated software that allows the volume of data collected to be processed or re-constructed and displayed in axial, sagittal and coronal planes. The CBCT NewTom VGi is used only for scanning of the maxillo-facial region.
An anatomical evaluation of the relationship between the root apices of the maxillary teeth and the maxillary sinus floor is essential for diagnosing sinus pathoses and treatment planning for proper dental implant placement. Therefore, determination the proximity of teeth to the maxillary sinus as well as the cortical thickness between the root apex and the inferior wall of the sinus is recommended for preoperative assessment. Knowledge of the topography of the inferior wall of the maxillary sinus is also important to understanding pathways of dental infection in endodontics.
The aims of the present study were: (1) to assess the vertical relationships of the upper premolars and molars with the maxillary sinus floor, by use of CBCT, and to compare with those measured on OPG; (2) to evaluate the bone density in the maxillary lateral region, by determining the Hounsfield Units (HU) after CBCT scanning, prior to implant decisions.
Materials and methods
The study was conducted between March 2006 and September 2009. Patients were recruited from a Radiological Center in Bucharest. For all subjects, personal data were collected by interview. All the ethical requirements were fulfilled.
Fifty-one clinical cases were randomly selected from a total of 700 patients referred for both OPG and CBCT a priori dental implant planning. The age of the patients ranged from 20 to 77 years (48 ± 14). Distribution by gender was balanced, i.e., 25 females (49.02 %) and 26 males (50.98 %). All subjects were partially edentulous.
The teeth assessed included 123 premolars with fused roots, among which 61 were maxillary first premolars and 62 maxillary second premolars. There were 114 molars with separated roots, among which 48 were maxillary first molars and 66 maxillary second molars. The second premolars with separated roots, as well as molars with fused roots and upper third molars were excluded from the study due to the scarcity of data.
Bone thickness between maxillary posterior teeth and maxillary sinus floor
Quantitative evaluations in each case were made using (1) OPGs (controls), (2) reconstructed panoramic sections of CBCTs images, and (3) tri-dimensional cross sections of CBCTs.
OPGs were performed with Orthopantomography Auto IIIN CM (Asahi Roentgen Ind. Co., Ltd., Japan). The images were made using Kodak cassette (Eastman Kodak Co., New York, USA), which had fine displays (Kodak, Eastman Kodak Co., New York, USA).
CBCTs were performed with NewTom VGi (QR SRL Co., Verona, Italy). Image detector was an amorphous silicon flat plate of 20 cm × 25 cm dimensions. The CBCT parameters were 110 kV, 1–20 mA, the emission of X-rays during 18 s, and the effective dose was 100 μSV. To achieve sagittal sections, CBCT reconstructions were set for a thickness of 1 mm. The original data were transferred to an independent work-station, with bundled software NewTom Implant Planning (Q.R. SRL, Verona, Italy), version 4.1.4, to generate 3D volume.
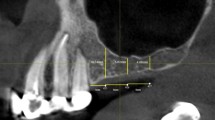
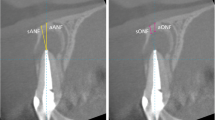
All measurements on OPGs and CBCTs were made from the root apex to the upper part of the cortical inferior wall of the sinus along the longitudinal axis of the root (Figs. 1, 2). The OPGs were scanned with Epson Perfection V600 (Photo, 3G International SRL, Bucharest, Romania). No changes of contrast and brightness were done during the scanning. Moreover, after scanning the OPGs, the measurements were done with an electronic calliper (PowerFix, PagetTrading Ltd., London, UK) with an accuracy of 10 μm. All these evaluations were repeated three times within 4 weeks, to obtain the reproducibility of values, by the same investigator (C.E.G.). Averages of these three measurements were then computed.
Bone quality between maxillary posterior teeth and maxillary sinus floor
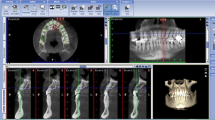
This was performed using colorimetric evaluations (Figs. 3, 4). Bone density was evaluated only on tridimensional reconstructions of the CBCT. Among the 97 investigated edentulous loci corresponding towards maxillary premolars, 51 were areas of first premolars and 46 of second premolars. Of the 96 investigated edentulous loci corresponding to maxillary molars, 52 were areas of first molars and 44 of second molars.
Color evaluations were made visually after a classification into 22 intervals corresponding to HU for bone density. Therefore, these categories were decreasing from the most dense bone (assigned as dark blue and corresponding to 3,000 HU) to the least dense one (assigned as red and corresponding to—1,000 UH) (Table 1 and Fig. 5).
Data from all records were processed. The 3D reconstruction program used was standard Open Graphics Library version 1.2.
Statistical analyses
Data were expressed as mean values, standard deviations (SD), percentages, as appropriate. One-way ANOVA test was used to assess mean differences between quantitative evaluations. Mann–Whitney (Wilcoxon) test was used to compare bone densities expressed by codes between different maxillary areas. StataIC 11 statistical software (StataCorp LP, Texas, USA, version 2009) was used for data analysis. A p value <0.05 was considered statistically significant.
Results
Bone thickness between maxillary posterior teeth and maxillary sinus floor
The mean values of the distances between the roots apices of the maxillary premolars and molars, and the maxillary sinus floor are shown in Tables 2 and 3. No statistical differences were recorded between the two methods used, when assessing the mean distances from the root apices to the maxillary sinus floor (p > 0.05, one-way ANOVA test).
Bone density assessment corresponding to maxillary posterior teeth on 3D CBCT images (after implant simulation)
The results of the mean bone densities obtained in the maxillary lateral area are presented in Table 4. The Mann–Whitney test showed no statistical evidence (p > 0.05) between bone density code evaluations of either first and second maxillary premolars, or first and second upper molars areas. However, there was a trend of increasing bone density between the areas corresponding to the maxillary first premolar gradually to that corresponding to the maxillary second molar.
Discussion
The aims of the study were to assess the quantity and quality of maxillary bone situated between maxillary posterior teeth and maxillary sinus floor. These assessments are essential for implant treatment planning. For successful dental therapy, an accurate diagnosis is recommended in order to identify a disease and to treat it, consequently. Beside clinical examination, the interpretation of radiographs provides additional valuable information. Even a good clinician, who possesses interpretive skills to identify normal structures on conventional radiographs, has difficulty in the evaluation of the intimate relationship that exists between the roots apices of maxillary teeth and the floor of the maxillary sinus, because of the superimpositions of multiple roots. Among the most recent radiographic imaging techniques, CT facilitates the assessment of the jaw bone and internal morphology of soft tissue, now serving as the gold standard [6]. CBCT has been used in dentistry since 1998. The amount of radiation delivered by this technique is much lower than that used in CT [12], although the dose of radiation used is at least four times higher than the dose used during OPG.
CBCT is appropriate for implant treatment planning and good supervision of implant placement due to the 3D imaging of hard tissue structures. CBCT is also recommended for sinus floor integrity evaluation after tooth extraction and before impression techniques [8]. Besides, the CBCT hardware and software are user-friendly [15]. Instead, the OPG, being a two-dimensional view, has limited value for predicting sinus perforation because of the morphology of the sinus floor [16]. In a previous study, the use of preoperatory OPG to predict maxillary sinus perforation after extraction, was not a reliable method [16, 19]. In the present study, the two methods seem of comparable reliability, as the values determined by them were not significantly different. In agreement with this, the fewest changes made on implant dimensions after using tomogram in addition to OPG were observed in the maxillary premolar region [21]. Sharan and Madjar [23] stated that the OPGs consistently showed a 2.1 times longer projection of the root on the sinus cavity in comparison to the root protrusion length into the sinus in the CT for roots classified as 3 (the root apex projecting on the sinus cavity) or 4 (a superiorly curving sinus floor enveloping part or all of the tooth root). These contradictory results are probably due to the fact that the topographic relationships of the roots to the maxillary sinus floor were not analyzed by stratification in the current study.
The maxillary sinus floor thickness may be influenced by anatomic features [4], demographic factors [24], as well as close proximity of perioral muscles [7]. The bone thickness measurements showed similarity to those of Kwak et al. [13]. Thus, the distance from the roots apices to the inferior wall of the sinus was the shortest in the second molar area (average 2.76 mm for the mesio-buccal root) and the longest in the first premolar area (average 7.65 mm). Eberhardt et al. [9] reported that the average distance from the root apices of the maxillary premolars and molars to the inferior wall of the maxillary sinus ranged from 1.97 mm for the mesio-buccal root of the second molars areas to 7.05 mm for the buccal roots of the first premolars. In our study, the shortest distance to the sinus floor was that from the apices of the mesio-buccal roots of the second molars (average 2.76 mm), whilst the longest one was measured from the apices of the first premolars’ united roots (average 7.56 mm). The roots of the posterior teeth are located close to the maxillary sinus floor and can be found outside the maxilla by 30 weeks of gestation. Therefore, the roots of the first and second molars are located in close proximity to the maxillary sinus floor [5].
With respect to the bone density assessed in the maxillary lateral area, the present results (1,060–1,392 HU) (Table 4) were higher than those of other studies, where the mean results were 673 HU, 333 HU, and 455 HU, respectively [20, 22, 25]. These differences might be explained by the use of CBCT in the current study, compared to conventional CT in the above mentioned studies [3].
Bone density of maxillary lateral area is higher corresponding to molars region, comparing to premolars area. Although the mean bone density was higher in the maxillary second molar region than in the maxillary first molar region (1,392 ±522 HU vs. 1,275 ± 380 HU), the difference was not statistically significant. It has been suggested that bone density values greater than 600 HU indicate dense trabecular bone [1]. The knowledge of the bone density is very important, the positive outcome for osseointegration depending mainly on it. With this respect, OPG is not a useful tool.
Even though our results support the minimal and maximal distances from tooth-to-sinus, as well as the average bone density in the maxillary lateral region, individual evaluation of each patient is required for proper preoperative planning.
References
Aamodt A, Kvistad KA, Andersen E, Lund-Larsen J, Eine J, Benum P, Husby OS (1999) Determination of Hounsfield value for CT-based design of custom femoral stems. J Bone Jt Surg Br 81:143–147
Abubaker A (1999) Applied anatomy of the maxillary sinus. Oral Maxillofac Surg Clin North Am 11:1–13
Aranyarachkul P, Caruso J, Gantes B, Schulz E, Riggs M, Dus I, Yamada JM, Crigger M (2005) Bone density assessments of dental implant sites: 2. Quantitative cone-beam computerized tomography. Int J Oral Maxillofac Implants 20:416–424
Arman C, Ergür I, Atabey A, Güvencer M, Kiray A, Korman E, Tetik S (2006) The thickness and the lengths of the anterior wall of adult maxilla of the West Anatolian Turkish people. Surg Radiol Anat 28:553–558
Asaumi R, Sato I, Miwa Y, Imura K, Sunohara M, Kawai T, Yosue T (2010) Understanding the formation of maxillary sinus in Japanese human foetuses using cone beam CT. Surg Radiol Anat 32:745–751
Brook I (2006) Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg 135:349–355
D’Andrea E, Barbaix E (2006) Anatomic research on the perioral muscles, functional matrix of the maxillary and mandibular bones. Surg Radiol Anat 28:261–266
Dimitrakopoulos I, Papadaki M (2008) Foreign body in the maxillary sinus: report of an unusual case. Quintessence Int 39:698–701
Eberhardt JA, Torabinejad M, Christiansen EL (1992) A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol 73:345–346
Kalender WA, Seissler W, Klotz E, Vock P (1990) Spiral volumetric CT with single-breath-hold technique, continuous transport, and continuous scanner rotation. Radiology 176:181–183
Kiessling F, Greschus S, Lichy MP, Bock M, Fink C, Vosseler S, Moll J, Mueller MM, Fusenig NE, Traupe H, Semmler W (2004) Volumetric computed tomography (VCT): a new technology for noninvasive, high-resolution monitoring of tumor angiogenesis. Nat Med 10:1133–1138
Kim IH, Mupparapu M (2009) Dental radiographic guidelines: a review. Quintessence Int 40:389–398
Kwak HH, Park HD, Yoon HR, Kang MK, Koh KS, Kim HJ (2004) Topographic anatomy of the inferior wall of the maxillary sinus in Koreans. Int J Oral Maxillofac Surg 33:382–388
Laine F (1999) Diagnostic imaging of the maxillary sinus. Oral Maxillofac Surg Clin North Am 11:45–67
Mupparapu M, Singer SR (2011) Dose reduction and cone beam CT: perception is reality. Quintessence Int 42:279
Nedbalski TR, Laskin DM (2008) Use of panoramic radiography to predict possible maxillary sinus membrane perforation during dental extraction. Quintessence Int 39:661–664
Nikolaou K, Flohr T, Stierstorfer K, Becker CR, Reiser MF (2005) Flat panel computed tomography of human ex vivo heart and bone specimens: initial experience. Eur Radiol 15:329–333
Obayashi N, Ariji Y, Goto M, Izumi M, Naitoh M, Kurita K, Shimozato K, Ariji E (2004) Spread of odontogenic infection originating in the maxillary teeth: computerized tomographic assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98:223–231
Oberli K, Bornstein MM, von Arx T (2007) Periapical surgery and the maxillary sinus: radiographic parameters for clinical outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103:848–853
Ozan O, Turkyilmaz I, Yilmaz B (2007) A preliminary report of patients treated with early loaded implants using computerized tomography-guided surgical stents: flapless versus conventional flapped surgery. J Oral Rehabil 34:835–840
Schropp L, Wenzel A, Kostopoulos L (2001) Impact of conventional tomography on prediction of the appropriate implant size. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92:458–463
Shapurian T, Damoulis PD, Reiser GM, Griffin TJ, Rand WM (2006) Quantitative evaluation of bone density using the Hounsfield index. Int J Oral Maxillofac Implants 21:290–297
Sharan A, Madjar D (2006) Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102:375–381
Teke HY, Duran S, Canturk N, Canturk G (2007) Determination of gender by measuring the size of the maxillary sinuses in computerized tomography scans. Surg Radiol Anat 29:9–13
Turkyilmaz I, Tözüm TF, Tumer C (2007) Bone density assessments of oral implant sites using computerized tomography. J Oral Rehabil 34:267–272
Wehrbein H, Diedrich P (1992) Progressive pneumatization of the basal maxillary sinus after extraction and space closure. Fortschr Kieferorthop 53:77–83
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Georgescu, C.E., Rusu, M.C., Sandulescu, M. et al. Quantitative and qualitative bone analysis in the maxillary lateral region. Surg Radiol Anat 34, 551–558 (2012). https://doi.org/10.1007/s00276-012-0955-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-012-0955-6