Abstract
Purpose
The presence of os acromiale is of clinical relevance before performing shoulder surgery but ethnic differences and little information regarding associated factors seem to be present. Population-based studies to clarify these topics are essential so the purpose of this study was to assess the prevalence, anatomy, and associations of os acromiale in a general adult population.
Methods
Both shoulders of 3050 participants from the population-based Study of Health in Pomerania (SHIP) were assessed on magnetic resonance imaging (MRI). Associations with the os acromiale were calculated for sex, age, body height, body weight, and heavy mechanical oscillations on the upper extremity.
Results
In total, 1.9% (58/3050) had an os acromiale, while 21 were unilateral left, 23 were unilateral right, and 14 were bilateral. Sixty-eight meso-acromions, three pre-acromions, and one meta-acromion were detected. Os acromiale were more frequent in men (right side: p = 0.037, left side: p = 0.005). Overall, no differences in sides (p = 0.808), to participants’ age (right: p = 0.993, left: p = 0.499), body height (right side: p = 0.241, left side: p = 0.154), and the exposure to heavy mechanical oscillations on the upper extremity (right: p = 0.054, left: p = 0.117) were detected.
Conclusion
Our results support the genetic theory for the aetiology of the os acromiale due to the lower prevalence of the os acromiale in north-eastern Germany compared to the worldwide prevalence (1.9 to 7%) and the lacking association to lifestyle, age, gender, or sides. Additionally, it is important to be aware of possible os acromiale before surgery.
Similar content being viewed by others
Introduction
The os acromiale is an accessory bone of the acromion, resulting from a failure of fusion during the development of the acromial process. The acromion is already formed in the early development. Fealy et al. documented its consistent cartilaginous shape throughout all gestational periods starting from gestational week 13 [1]. During physiological growth, three independent centres of ossification, the pre-, meso-, and meta-acromion, are formed until the age of 18 who will grow and fuse with the basi-acromion to the definite acromion between the age of 23–25 years [2,3,4]. Recent studies on adolescents described a considerably earlier complete osseous fusion between the age of 14 and 16 [5, 6].
During fusion-failures, seven types of os acromiale are possible [7]. However, mostly three different os acromiale occur: the pre-acromion is the lack of fusion between pre- and meso-acromion, the meso-acromion between meso- and meta-acromion, and the meta-acromion between meta- and basi-acromion (Fig. 1) [8]. The most common form is the meso-acromion, followed by pre-acromions while meta-acromions are a rare condition [2, 8,9,10,11,12,13]. The attachment of the os acromiale to the rest of the acromion can be nearly complete and immobile, fibrocartilaginous (pseudarthrotic), or even a synovial joint [3, 9]. Os acromiale can be detected with radiographs, but the most reliable diagnostic is achieved by MRI [7].
The exact aetiology and associated factors of the os acromiale are not completely resolved. One hypothesis suggests a genetic predisposition [9, 14]. Another theory holds mechanical stress during the development of the acromion accountable [15]. A third option could be a combination of genetic and mechanic influences [4]. The reported prevalence of os acromiale ranges between 0.7 and 18.2% [4, 11] with a mean of 7% [12].
Regarding further associations, various results are described: association with the dominant side [4, 8, 11, 16, 17], gender [4, 8, 9, 11,12,13, 16, 17], or work load [4, 15] is discussed controversially. However, most of the present studies were conducted on cadavers, archeological skeletons, small or hospital-based samples. Therefore, population-based studies are crucial to clarify these topics.
In respect of the clinical relevance of the os acromiale, associations with various shoulder pathologies were described. Older studies determined an association between os acromiale and subacromial impingement as well as rotator cuff pathology and subacromial bursitis [7, 18, 19]. Recent studies are strongly questioning these associations [8, 11, 13, 20]. Even for patients with reverse shoulder arthroplasty (RSA), a comparable outcome to patients without os acromiale was described [21, 22].
However, sometimes os acromiale is a possible cause for pain [23]. There are different theories about the pathogenesis of symptomatic os acromiale: an inflammation at the pseudarthrosis, an unstable os acromiale leading to dynamic subacromial impingement, or arthritic degeneration due to hypermobility of the unfused bone [24, 25]. Regarding treatment of symptomatic os acromiale, there is no consensus until today.
Given the importance to not overlook an existing os acromiale, the lack of population-based values and knowledge on influencing factors, population-based studies are crucial. Therefore, the aim of this study was to assess the frequency, anatomy, and associations of os acromiale in a general adult population.
Methods
Design and sample
Data from the Study of Health in Pomerania (SHIP) was examined. The study is an ongoing population-based project with two independent cohorts, SHIP-START and SHIP-TREND. To achieve the population-based approach, participants were recruited randomly from official resident registry office files of a defined region in north-eastern Germany and stratified by sex, age, and city of residence. All participants were of Caucasian ethnicity.
As baseline (SHIP-START-0), 6265 eligible adults were chosen with a response of 68.8% in 1997. Between 2002 and 2006 (SHIP-START-1; n = 3300) and from 2008 to 2012 (SHIP-START-2; n = 2333), two follow-ups took place. The second cohort (SHIP-TREND-0, n = 4420) was examined baseline from 2008 to 2012. A high response rate was achieved by three written invitations, phone calls, and one personal contact. The local ethics commission approved the study and each participant gave written informed consent. Further study details have already been published [26].
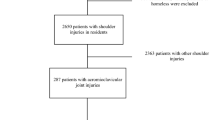
The presented analysis was performed on MRI of all participants from SHIP-START-2 and SHIP-TREND-0. 3317 of 6753 participants (SHIP-START-2 and SHIP-TREND-0) underwent the MRI examination, whereof 266 participants dropped-out because of claustrophobia, acute problems, metal implants, or personal reasons. One data was missing. In total, MRI of 3050 participants were investigated in the current analysis (Fig. 2).
MRI protocol
The MRI was part of the standardized whole-body MRI (1.5-T MR scanner, Magnetom Avanto; Siemens Medical Systems, Erlangen, Germany). All MRIs were performed by four trained technicians. To assess the os acromiale, axial T1 volume interpolated breath hold examination sequences (repetition time 3.1 ms; echo time 1.1 ms; flip angle 8°; voxel size 1.8 × 1.8 × 3.0 mm), an axial T2 Half Fourier-Acquired Single shot Turbo spin Echo sequence (repetition time 550 ms; echo time 22 ms; flip angle 150°; voxel size 2.3 × 1.8 × 5.0 mm), and an coronal turbo inversion recovery magnitude sequence (repetition time 4891 ms; echo time 67 ms; flip angle 180°; voxel size 2.1 × 1.6 × 5.0 mm) were used.
Image analysis
All MRI were examined by two trained examiners (CF, MF). The observers were blinded to all clinical information of the participants, while using the OsiriX (PIXMEO; Bernex, Switzerland) software. Since the axial plane is best to identify the “double joint” sign of an os acromiale [7, 8, 27], axial and coronal MRI in different thicknesses were used to perform all measurements and classifications. The presence and the type of an os acromiale were evaluated. Additionally, it was classified according to Gumina et al. [28] and its length, thickness, and width was measured in tenth of millimeter.
Patient-related parameters
As patient-related parameters, the participants’ age, gender, body height, and body weight were determined. Additionally, shoulder pain on the visual analog scale (VAS) in the last seven days, proximal humeral fracture in the patients’ medical history, and the exposure to heavy mechanical oscillations on the upper extremity (e.g., working with impact drill machines, chainsaw) at the workplace and the amount of years were assessed. Moreover, seeing a surgeon or orthopedist in the last 12 months and the number of visits were documented.
Statistics
Descriptive statistics such as mean values, standard deviations (SD), ranges, and percentiles were used to describe the sample. Student’s t-test was used for numerical variables; continuous variables were analyzed by Wilcoxon tests while categorical data was examined with Chi2-tests. A p value of < 0.05 was considered as statistically significant. Associations of demographic and anamnestic data with the os acromiale were analyzed by univariate logistic regression models. The statistical analysis was performed using Stata 16.1 (Stata Corp., College Station, TX, USA).
Results
Out of the 3,050 participants 52% were females while the mean age was 52.8 ± 13.8 years with marginal differences between the sexes. The mean values of body height, body weight, and BMI were higher in males than in females (Table 1). Shoulder pain in the last 7 days was 1.1 (VAS) in the mean. Only 20 participants were left-handed.
In total, 72 os acromiale were found in 58 different participants. Therefore, 1.9% of the whole sample showed an os acromiale, while 21 (36%) were unilateral left, 23 (40%) were unilateral right, and 14 (24%) were bilateral. Sixty-eight meso-acromions, three pre-acromions, and one meta-acromion were detected (Table 2). The meso-acromions had a mean size of 23.16 mm (length) × 24.33 mm (width) × 10.31 mm (thickness). Detailed information on the size is presented in Table 3. Following the classification of Gumina et al. [28], 56.9% of all os acromiale were classified as intermediate, 36.1% were cobra shaped, 2.8% square tip, and in 4.2% the Gumina classification was not possible. In males, there were 12 os acromiale on the left side, 11 on the right side, and 13 men had a bilateral os acromiale. One of the male participants with an os acromiale had had a humeral head fracture in his medical history, but on the contralateral side. The frequency in women was 12 unilateral os acromiale on the right side while nine were unilateral left and one bilateral. Therefore, unilateral and bilateral os acromiale were more frequent for men than for women (right side: p = 0.037, left side: p = 0.005). No differences in sides were detected (p = 0.808). Two out of the 20 left-handed participants had an os acromiale but on the right side. Participants with os acromiale had a greater body height than participants without, but after adjusting the results on gender no significant differences were found (right side: p = 0.241, left side: p = 0.154). Gender-adjusted body weight analyses showed a significant association to right os acromiale (p = 0.016), whereas no significant results occurred for the left side (p = 0.132).
No associations to participants’ age (right: p = 0.993, left: p = 0.499), shoulder pain (right: p = 0.559, left: p = 0.445), visiting a surgeon (right: p = 0.787, left: p = 0.367) or orthopedist (right: p = 0.600, left: p = 0.481), and to heavy mechanical oscillations on the upper extremity (right: p = 0.054, left: p = 0.117) were detected.
Discussion
The os acromiale is mostly investigated by studies on skeletons or cadavers. Only few authors published results in vivo using hospital-based data to conduct these studies (Table 4). In addition, the lack of population-based knowledge on frequency and influencing factors is still ongoing. For this reason, we decided to investigate MRI of the population-based SHIP project.
In this large population-based study, 1.9% of the 3050 participants had at least one os acromiale. The frequency of bilaterality was 24%.
As described in earlier studies [8,9,10,11,12], most os acromiale in the present study were os meso-acromiale (94.4%). Compared to previous studies on os acromiale (Table 4), frequency and proportion of bilaterality in the current study were considerably lower. In their review, Yammine described a prevalence of 5.78% in 3935 individuals, respectively 5.16% at the pooled rate from seven large-sample studies for os acromiale for people of white ancestry [12]. However, the prevalence varies depending on the ethnic group. Asian studies reported the lowest frequency with 0.7% [11]. The prevalence in Caucasians varies between 1 and 15% [3, 29, 30] while studies in African-Americans and Africans had the highest prevalence with 9.2–18.2% [4, 9]. Bilateral os acromiale were reported with a frequency of 12.5–62% [30, 31]. Additionally, a higher frequency of bilateral os acromiale is described for black people [9, 31].
Since Angel et al. [14] proposed the idea of a genetic influence on the formation of os acromiale due to their results on the remains of a Baptist graveyard in 1987, multiple studies supported this view [9, 12, 31]. An opposing theory was suggested by Stirland which considers mechanical stress as the main cause for the formation of os acromiale due to their observations on the British warship Mary Rose. On the basis of the high number of longbow archers and the high prevalence of os acromiale, Stirland proposed the theory of stress-induced trauma [15]. In opposition, Case et al. did not find any differences between people with higher and lower socioeconomic status, while for a lower socioeconomic status harder physical work was presumed [4]. The results of the present population-based study mainly support the genetic theory because no association between os acromiale and high exposure to heavy mechanical oscillations on the upper extremity was found. Additionally, with 1.9% a lower prevalence of the os acromiale was detected even though participants starting from the age of 18 were included. Consequently, falsely diagnosed os acromiale could possibly be included in our sample because they would have moved on to consolidation later in life. However, our exclusively Caucasian sample of north-eastern Germany seems to have a distinct genetic pool with a low rate of os acromiale compared to the worldwide prevalence of 7% [12] and therefore the sample’s low prevalence supports the genetic theory.
Moreover, no differences regarding sides were detected. A conclusive calculation regarding the dominant side was not possible because only 20 left-handed participants were present in our study sample. However, a correlation to the dominant side seems unlikely because the two left-handed participants with os acromiale were os acromiale on the right side. In previous works, Aibinder et al. discovered os acromiale more frequently on the dominant side [16], while other authors found higher frequencies on the left side [4] or on the right side [8]. Some studies did not find any differences in sides [11, 17].
Gumina et al. suggested in 2003 that the frequency of os acromiale increases with increasing distance between the anterior aspect of the acromion and the acromioclavicular joint [28]. However, the present results cannot support this thesis as most of the os acromiale were intermediate shaped according to the Gumina classification (56.9%).
Regarding associations to os acromiale, a higher prevalence for men was detected, while no associations for age and body height were present. The significant association between body weight and the os acromiale on the right side seems to be coincidentally. Previous studies revealed a higher prevalence of os acromiale in men [9, 16] as well but many authors did not confirm the gender differences [4, 8, 11,12,13, 17]. Associations to age were not found until now [4].
Given that stable and asymptomatic os acromiale can become unstable and symptomatic due to trauma or surgical interventions, e.g., subacromial decompression [32, 33], it is crucial to be aware of potential os acromiale before surgery. In addition, the os acromiale can be a cause of shoulder pain itself due to inflammation at the pseudarthrosis, dynamic subacromial impingement, or arthrosis [24, 25]. Therefore, it is of clinical relevance to recognize os acromiale and be aware of its prevalence.
Regarding treatment of symptomatic os acromiale, there is no consensus until today. Usually, a conservative approach is used as first-line therapy for at least six months. Afterwards, surgical intervention should be considered [34]. The discussion about the optimal surgical technique is still ongoing. Currently different methods like excision, acromioplasty, and open reduction and internal fixation (ORIF) are the topic of many reviews. With small os acromiale, there is a trend to excision, while for larger os acromiale ORIF seems to be beneficial to preserve the deltoid function [25, 32, 34].
A limitation of our study might be how representative our sample is. Due to selection by response to the baseline SHIP-TREND-0, to the baseline and follow-up examinations of SHIP-START-2 as well as to the MRI subproject, representativeness might have been diminished. Moreover, our study consists of an exclusively Caucasian population. With respect to known ethnic differences [9, 12], our results may not apply to non-Caucasian individuals. Another limitation is the possible inclusion of participants with shoulder pathology through the population-based study design. However, none of our participants with os acromiale showed any sign of previous shoulder surgery (metal implants, anchors etc.). One participant with os acromiale had a humeral fracture in his history, but on the contralateral side. Moreover, we investigated a general population, so it can be expected that the majority of the participants were healthy and without pathology. Since participants with metal implants are excluded due to the MRI, the prevalence could be underestimated. Another weakness of the current study is the cross-sectional design, which only provides associations, but no cause-and-effect relationships.
A last limitation might be the already mentioned inclusion of participants from the age of 18 which could lead to a degree of bias with falsely diagnosed os acromiale since some authors stated that the os acromiale should only be diagnosed after the age of 25 [18]. However, recent studies showed that the complete osseous fusion of the acromion takes place before the age of 18 [5, 6]. In MRI on 85 children, Kothary and Rosenberg detected a starting fusion of the ossification centers at the age of 14. Generally, it was completed after the age of 16 [5].
Conclusion
In conclusion, the prevalence of 1.9% of os acromiale in north-eastern Germany is relatively low comparing to the worldwide prevalence of 7%. This may be based on the genetic pool in this area. Additionally, no other association to lifestyle, age, gender, or sides was detected so our study supports the genetic theory for the etiology of the os acromiale. Despite the low prevalence, it is important to be aware of potential os acromiale before surgery, so MRI are advised. Since therapy on symptomatic os acromiale depends on the size of the os acromiale, current measurements were given.
References
Fealy S, Rodeo SA, Dicarlo EF et al (2000) The developmental anatomy of the neonatal glenohumeral joint. J Shoulder Elbow Surg 9:217–222. https://doi.org/10.1067/mse.2000.105624
McClure JG, Raney RB (1975) Anomalies of the scapula. Clin Orthop Relat Res.:22–31. https://doi.org/10.1097/00003086-197507000-00005
Macalister A (1893) Notes on acromion. J Anat Physiol 27:244.1-251
Case DT, Burnett SE, Nielsen T (2006) Os acromiale: population differences and their etiological significance. Homo 57:1–18. https://doi.org/10.1016/j.jchb.2005.11.001
Kothary P, Rosenberg ZS (2015) Skeletal developmental patterns in the acromial process and distal clavicle as observed by MRI. Skeletal Radiol 44:207–215. https://doi.org/10.1007/s00256-014-2020-5
Winfeld M, Rosenberg ZS, Wang A et al (2015) Differentiating os acromiale from normally developing acromial ossification centers using magnetic resonance imaging. Skeletal Radiol 44:667–672. https://doi.org/10.1007/s00256-015-2098-4
Park JG, Lee JK, Phelps CT (1994) Os acromiale associated with rotator cuff impingement: MR imaging of the shoulder. Radiology 193:255–257. https://doi.org/10.1148/radiology.193.1.8090902
Rovesta C, Marongiu MC, Corradini A et al (2017) Os acromiale: frequency and a review of 726 shoulder MRI. Musculoskelet Surg 101:201–205. https://doi.org/10.1007/s12306-017-0463-2
Hunt DR, Bullen L (2007) The frequency of os acromiale in the Robert. J Terry Collection Int J Osteoarchaeol 17:309–317. https://doi.org/10.1002/oa.877
Nicholson GP, Goodman DA, Flatow EL et al (1996) The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg 5:1–11. https://doi.org/10.1016/S1058-2746(96)80024-3
Kumar J, Park WH, Kim S-H et al (2013) The prevalence of os acromiale in Korean patients visiting shoulder clinic. Clin Orthop Surg 5:202–208. https://doi.org/10.4055/cios.2013.5.3.202
Yammine K (2014) The prevalence of os acromiale: a systematic review and meta-analysis. Clin Anat 27:610–621. https://doi.org/10.1002/ca.22343
Boehm TD, Rolf O, Martetschlaeger F et al (2005) Rotator cuff tears associated with os acromiale. Acta Orthop 76:241–244. https://doi.org/10.1080/00016470510030643
Angel JL, Kelley JO, Parrington M et al (1987) Life stresses of the free black community as represented by the First African Baptist Church, Philadelphia, 1823–1841. Am J Phys Anthropol 74:213–229. https://doi.org/10.1002/ajpa.1330740209
Stirland AJ (2000) Raising the dead: the skeleton crew of Henry VIII’s great ship, the Mary Rose. Wiley, Chichester
Aibinder WR, Schoch BS, Cofield RH et al (2017) Reverse shoulder arthroplasty in patients with os acromiale. J Shoulder Elbow Surg 26:1598–1602. https://doi.org/10.1016/j.jse.2017.02.012
Vallois H-V (1926) Les anomalies de l’omoplate chez l’homme. Bulletins et Mémoires de la Société d’Anthropologie de Paris 7:20–37. https://doi.org/10.3406/bmsap.1926.8987
Prescher A (2000) Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. Eur J Radiol 35:88–102. https://doi.org/10.1016/S0720-048X(00)00225-4
Mudge MK, Wood VE, Frykman GK (1984) Rotator cuff tears associated with os acromiale. J Bone Joint Surg Am 66:427–429
Ouellette H, Thomas BJ, Kassarjian A et al (2007) Re-examining the association of os acromiale with supraspinatus and infraspinatus tears. Skeletal Radiol 36:835–839. https://doi.org/10.1007/s00256-007-0305-7
Carpeggiani G, Hodel S, Götschi T et al (2020) Os acromiale in reverse total shoulder arthroplasty: a cohort study. Orthop J Sports Med 8:2325967120965131. https://doi.org/10.1177/2325967120965131
Shin W-J, Lee H-J, An K-Y (2020) Reverse shoulder arthroplasty with os acromiale. Clin Shoulder Elbow 23:100–104. https://doi.org/10.5397/cise.2019.00409
Arenas-Miquelez A, Hertel R (2020) The unstable os acromiale: a cause of pain in the young athlete. JSES Int 4:559–563. https://doi.org/10.1016/j.jseint.2020.02.008
Barbier O, Block D, Dezaly C et al (2013) Os acromiale, a cause of shoulder pain, not to be overlooked. Orthop Traumatol Surg Res 99:465–472. https://doi.org/10.1016/j.otsr.2012.10.020
Purnell JA, Bourget-Murray J, Kwapisz A et al (2019) Clinical results and complications following surgical management of symptomatic os acromiale: a systematic review. J Orthop Surg Res 14:26. https://doi.org/10.1186/s13018-018-1041-5
Völzke H, Alte D, Schmidt CO et al (2011) Cohort profile: the study of health in Pomerania. Int J epidemiol 40:294–307. https://doi.org/10.1093/ije/dyp394
Uri DS, Kneeland JB, Herzog R (1997) Os acromiale: evaluation of markers for identification on sagittal and coronal oblique MR images. Skeletal Radiol 26:31–34. https://doi.org/10.1007/s002560050187
Gumina S, de Santis P, Salvatore M et al (2003) Relationship between os acromiale and acromioclavicular joint anatomic position. J Shoulder Elbow Surg 12:6–8. https://doi.org/10.1067/mse.2003.128136
Coskun N, Karaali K, Cevikol C et al (2006) Anatomical basics and variations of the scapula in Turkish adults. Saudi Med J 27:1320–1325
Liberson F (1937) Os acromiale—a contested anomaly. JBJS 19:683–689
Sammarco VJ (2000) Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am 82:394–400. https://doi.org/10.2106/00004623-200003000-00010
Hurst SA, Gregory TM, Reilly P (2019) Os acromiale: a review of its incidence, pathophysiology, and clinical management. EFORT Open Rev 4:525–532. https://doi.org/10.1302/2058-5241.4.180100
Neyton L, Noël E, Walch G et al (2014) Acromion reconstruction after failed subacromial decompression in shoulders with os acromiale (meso-acromion): the tongue-and-groove assembly. J Shoulder Elbow Surg 23:e261–e265. https://doi.org/10.1016/j.jse.2014.07.002
Viner GC, He JK, Brabston EW et al (2020) Os acromiale: systematic review of surgical outcomes. J Shoulder Elbow Surg 29:402–410. https://doi.org/10.1016/j.jse.2019.05.047
Acknowledgements
We thank our four trained technicians Angela Doss, Petra Bartel, Brigitte Olbrich, and Vera Radons, who performed all MRI examinations; the members of the Institute of Community Medicine; and all participants.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was performed as an associated project to SHIP at University Medicine Greifswald, Greifswald, Germany. The SHIP study is part of the Community Medicine Research Net of the University of Greifswald, Germany, which is funded by the Federal Ministry of Education and Research (grant No. 03ZIK012), the Ministry of Cultural Affairs, as well as the Social Ministry of the Federal State of Mecklenburg-West Pomerania. MR imaging was supported by the Federal State of Mecklenburg-Vorpommern, the Federal Ministry of Education and Research, and a joint grant from Siemens Healthcare, Erlangen, Germany.
Author information
Authors and Affiliations
Contributions
C.F. performed all measurements. C.F., M.F., J.L., and MD.A. were responsible for the study design and the scientific subsumption. T.I. performed the statistical analyses. H.V. and R.B. were responsible for data collection and provided advice on study design. All authors revised and approved the manuscript applied for publication.
Corresponding author
Ethics declarations
Consent participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fischer, C.S., Floß, M., Ittermann, T. et al. Os acromiale: prevalence and associated patient-related factors—a population-based study of three thousand and fifty participants. International Orthopaedics (SICOT) 46, 1583–1590 (2022). https://doi.org/10.1007/s00264-022-05406-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05406-0