Abstract
Purpose
The aim of this study was to determine the incidence of prolonged wound drainage (PWD) and the amount of drainage fluid after hip hemiarthroplasty (HA) and to investigate the risk factors for the development of PWD associated with the patient, fracture and surgical treatment.
Methods
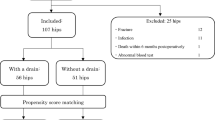
Data from 313 patients who underwent HA were prospectively analysed. The mean drainage time and drainage amount of patients with PWD were calculated. Patient demographic data, pre-operative ASA scores and anticoagulation status, presence of diabetes, fracture type, surgical approach, femoral stem type, cable usage, amount of drain output, blood transfusion quantity, time from injury to surgery, time from surgery to discharge and patient blood tests were investigated.
Results
The incidence of PWD after HA was 8.9% (28 patients). The mean drainage time in patients with PWD was 4.9 ± 1.85 (3–9) days, and the mean collected total fluid volume was 51.1 ± 26.9 (21–132) mL. PWD was more commonly observed in the lateral approach group (p < 0.001) and morbidly obese patients (p < 0.001). In the PWD group, the mean post-operative first-day haemoglobin value was lower (p < 0.001), more blood transfusions were required (p < 0.001) and the amount of drainage output from the closed suction drain (CSD) was higher (p < 0.001). The duration of hospitalization was longer in patients with PWD (p < 0.001). Lateral approach, morbid obesity and increased drainage output were found to be associated with PWD in logistic regression analysis.
Conclusion
Lateral approach, morbid obesity and increased drainage output were found to be risk factors for the occurrence of PWD.




Similar content being viewed by others
References
Cordero-Ampuero J, de Dios M (2010) What are the risk factors for infection in hemiarthroplasties and total hip arthroplasties? Clin Orthop Relat Res 468:3268–3277. https://doi.org/10.1007/s11999-010-1411-8
Florschutz AV, Fagan RP, Matar WY, Sawyer RG, Berrios-Torres SI (2015) Surgical site infection risk factors and risk stratification. J Am Acad Orthop Surg 23(Suppl):S8–s11. https://doi.org/10.5435/jaaos-d-14-00447
Noailles T, Brulefert K, Chalopin A, Longis PM, Gouin F (2016) What are the risk factors for post-operative infection after hip hemiarthroplasty? Systematic review of literature. Int Orthop 40:1843–1848. https://doi.org/10.1007/s00264-015-3033-y
Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J (2008) Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res 466:1710–1715. https://doi.org/10.1007/s11999-008-0209-4
Wagenaar FBM, Lowik CAM, Zahar A, Jutte PC, Gehrke T, Parvizi J (2019) Persistent wound drainage after total joint arthroplasty: a narrative review. J Arthroplasty 34:175–182. https://doi.org/10.1016/j.arth.2018.08.034
CAM L, Wagenaar FC, van der Weegen W, Poolman RW, Nelissen R, Bulstra SK, Pronk Y, Vermeulen KM, Wouthuyzen-Bakker M, van den Akker-Scheek I, Stevens M, Jutte PC, group Ls (2017) LEAK study: design of a nationwide randomised controlled trial to find the best way to treat wound leakage after primary hip and knee arthroplasty. BMJ Open 7:e018673. https://doi.org/10.1136/bmjopen-2017-018673
Ghanem E, Heppert V, Spangehl M, Abraham J, Azzam K, Barnes L, Burgo FJ, Ebeid W, Goyal N, Guerra E, Hitt K, Kallel S, Klein G, Kosashvili Y, Levine B, Matsen L, Morris MJ, Purtill JJ, Ranawat C, Sharkey PF, Sierra R, Stefansdottir A (2014) Wound management. J Orthop Res 32(Suppl 1):S108–S119. https://doi.org/10.1002/jor.22554
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27:61-65.e61. doi:https://doi.org/10.1016/j.arth.2012.02.022
Al-Houraibi RK, Aalirezaie A, Adib F, Anoushiravani A, Bhashyam A, Binlaksar R, Blevins K, Bonanzinga T, Chih-Kuo F, Cordova M, Deirmengian GK, Fillingham Y, Frenkel T, Gomez J, Gundtoft P, Harris MA, Harris M, Heller S, Jennings JA, Jiménez-Garrido C, Karam JA, Khlopas A, Klement MR, Komnos G, Krebs V, Lachiewicz P, Miller AO, Mont MA, Montañez E, Romero CA, Schwarzkopf R, Shaffer A, Sharkey PF, Smith BM, Sodhi N, Thienpont E, Villanueva AO, Yazdi H (2019) General assembly, prevention, wound management: proceedings of international consensus on orthopedic infections. J Arthroplasty 34:S157–s168. https://doi.org/10.1016/j.arth.2018.09.066
Ng VY, Lustenberger D, Hoang K, Urchek R, Beal M, Calhoun JH, Glassman AH (2013) Preoperative risk stratification and risk reduction for total joint reconstruction: AAOS exhibit selection. J Bone Joint Surg Am 95:e191–e115. https://doi.org/10.2106/jbjs.l.00603
Parvizi J, Gehrke T, Chen A (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J 95:1450–1452. https://doi.org/10.1302/0301-620X.95B11.33135
Adelani M, Johnson S, Keeney J, Nunley R, Barrack R (2014) Clinical outcomes following re-admission for non-infectious wound complications after primary total knee replacement. Bone Joint J 96:619–621. https://doi.org/10.1302/0301-620X.96B5.33479
Jaberi FM, Parvizi J, Haytmanek CT, Joshi A, Purtill J (2008) Procrastination of wound drainage and malnutrition affect the outcome of joint arthroplasty. Clin Orthop Relat Res 466:1368–1371. https://doi.org/10.1007/s11999-008-0214-7
Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE (2007) Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am 89:33–38. https://doi.org/10.2106/JBJS.F.00163
Maathuis P, de Hartog B, Bulstra S (2009) Timing of open debridement for suspected infection of joint prosthesis: a report on 551 patients. Curr Orthop Pract 20:541–545. https://doi.org/10.1097/BCO.0b013e3181a0a7fb
Aggarwal VK, Elbuluk A, Dundon J, Herrero C, Hernandez C, Vigdorchik JM, Schwarzkopf R, Iorio R, Long WJ (2019) Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Joint J 101-b:646-651. doi:https://doi.org/10.1302/0301-620x.101b6.bjj-2018-1474.r1
van der Sijp MPL, van Delft D, Krijnen P, Niggebrugge AHP, Schipper IB (2018) Surgical approaches and hemiarthroplasty outcomes for femoral neck fractures: a meta-analysis. J Arthroplasty 33:1617-1627.e1619. doi:https://doi.org/10.1016/j.arth.2017.12.029
Biber R, Brem M, Singler K, Moellers M, Sieber C, Bail HJ (2012) Dorsal versus transgluteal approach for hip hemiarthroplasty: an analysis of early complications in seven hundred and four consecutive cases. Int Orthop 36:2219–2223. https://doi.org/10.1007/s00264-012-1624-4
Ahmed AA, Mooar PA, Kleiner M, Torg JS, Miyamoto CT (2011) Hypertensive patients show delayed wound healing following total hip arthroplasty. PLoS One 6:e23224. https://doi.org/10.1371/journal.pone.0023224
Kilpadi DV, Cunningham MR (2011) Evaluation of closed incision management with negative pressure wound therapy (CIM): hematoma/seroma and involvement of the lymphatic system. Wound Repair Regen 19:588–596. https://doi.org/10.1111/j.1524-475X.2011.00714.x
Pauser J, Nordmeyer M, Biber R, Jantsch J, Kopschina C, Bail HJ, Brem MH (2016) Incisional negative pressure wound therapy after hemiarthroplasty for femoral neck fractures - reduction of wound complications. Int Wound J 13:663–667. https://doi.org/10.1111/iwj.12344
Strahovnik A, Fokter SK, Kotnik M (2010) Comparison of drainage techniques on prolonged serous drainage after total hip arthroplasty. J Arthroplasty 25:244–248. https://doi.org/10.1016/j.arth.2008.08.014
Abdel MP, Barreira P, Battenberg A, Berry DJ, Blevins K, Font-Vizcarra L, Frommelt L, Goswami K, Greiner J, Janz V, Kendoff DO, Limberg AK, Manrique J, Moretti B, Murylev V, O'Byrne J, Petrie MJ, Porteous A, Saleri S, Sandiford NA, Sharma V, Shubnyakov I, Sporer S, Squire MW, Stockley I, Tibbo ME, Turgeon T, Varshneya A, Wellman S, Zahar A (2019) Hip and knee section, treatment, two-stage exchange spacer-related: proceedings of international consensus on orthopedic infections. J Arthroplasty 34:S427–s438. https://doi.org/10.1016/j.arth.2018.09.027
Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA (2016) Periprosthetic joint infection. Lancet 387:386–394. https://doi.org/10.1016/S0140-6736(14)61798-0
Toma O, Suntrup P, Stefanescu A, London A, Mutch M, Kharasch E (2011) Pharmacokinetics and tissue penetration of cefoxitin in obesity: implications for risk of surgical site infection. Anesth Analg 113:730–737. https://doi.org/10.1213/ANE.0b013e31821fff74
D’Apuzzo MR, Novicoff WM, Browne JA (2015) The John Insall award: morbid obesity independently impacts complications, mortality, and resource use after TKA. Clin Orthop Relat Res 473:57–63. https://doi.org/10.1007/s11999-014-3668-9
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Canbek, U., Akgun, U., Aydogan, N.H. et al. Factors associated with prolonged wound drainage after hemiarthroplasty for hip fractures in elderly. International Orthopaedics (SICOT) 44, 1823–1831 (2020). https://doi.org/10.1007/s00264-020-04738-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04738-z