Abstract
Purpose
Laminectomy with lateral mass screw fixation has been proven to be an effective method to treat the multilevel cervical degenerative myelopathy and severe cervical spondylosis. However, accurate and safe insertion of the lateral mass screw is technically demanding due to the individual variations of the anatomy of the lateral mass of the subaxial cervical spine. Misplaced lateral mass screw is not uncommon, and operation-related complications still beset the surgeons, which may impair the clinical outcomes. This study aimed to introduce a novel strategy for safe and accurate insertion of lateral mass screw in the subaxial cervical spine.
Methods
From July 2014 to March 2015, 24 patients with multilevel cervical degenerative myelopathy at C3-C6 levels received laminectomy. Before the operation, the screw insertion technique depended on the pre-operative imaging and operative exploration. Following this strategy, the lateral mass screws were inserted into the subaxial cervical spines. Post-operative radiograph was performed to observe the locations of the lateral mass screws and the cervical curvature. Patients were followed up, and the functional neurological recovery was evaluated by the modified Japanese Orthopedic Association (JOA) disability scale, the Neck Disability Index (NDI) and NDI ranking system.
Results
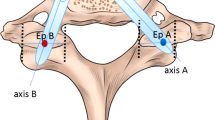
All screws were inserted into the lateral mass of C3-C6 cervical vertebrae following the current technique. Post-operative CT scans confirmed all screws inserted into the safe zone and relative safe zone of the lateral mass without any screw placed into the transverse foramen. The angle between the lateral mass screw and the vertical line was 40.49 ± 5.44 degrees on the axial CT images. Twenty-four patients were followed up for an average of 25.79 months (range, 20–30 months), and 22 cases evaluated as no or mild disability. According to the JOA score, NDI score and NDI ranking system, the postoperative function of the patients was significantly better when compared with their preoperative corresponding data (all p < 0.001)
Conclusion
Inserting lateral mass screw following this new strategy is safe and easy to perform without any screw-related neurovascular complications, which contribute to the rigid fixation of the subaxial cervical spine and the satisfactory functional recovery.





Similar content being viewed by others
References
Ebraheim NA, Shafiq Q, Xu R, Alhamdan FA, Madsen TD (2004) Roy-Camille technique for traumatic instability of the lower cervical spine. Internet J Spine Surg 2(1):1–6
Korres D, Nikolaou VS, Kaseta M, Evangelopoulos D, Markatos K, Lazarettos J, Efstathopoulos N (2014) Posterior stabilization of cervical spine injuries using the Roy-Camille plates: a long-term follow-up. Eur J Orthop Surg Traumatol 24(Suppl 1):125–130. doi:10.1007/s00590-013-1376-x
Barbarawi MMA, Audat ZA, Obeidat MM, Qudsieh TM, Dabbas WF, Obaidat MH, Malkawi AA (2011) Decompressive cervical laminectomy and lateral mass screw-rod arthrodesis. Surgical analysis and outcome. Scoliosis 6(1):1–6. doi:10.1186/1748-7161-6-10
Anderson PA, Matz PG, Groff MW, Heary RF, Holly LT, Kaiser MG, Mummaneni PV, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK (2009) Laminectomy and fusion for the treatment of cervical degenerative myelopathy. J Neurosurg Spine 11:150–156
Du W, Wang L, Shen Y, Zhang Y, Ding W, Ren L (2013) Long-term impacts of different posterior operations on curvature, neurological recovery and axial symptoms for multilevel cervical degenerative myelopathy. Eur Spine J 22(7):1594–1602. doi:10.1007/s00586-013-2741-5
6.Roy-Camille R, Gaillant G, Bertreaux D (1979) Early management of spinal injuries. In: McKibben B (ed) Recent Advances in Orthopedics. Churchill-Livingstone, Edinburgh, p 57–87
Manning F (1991) Posterior stabilization of the cervical spine with hook plates. Spine 16(3 Suppl):56–63
Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR (1991) Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine 16(3 Suppl):72–79
An HS, Gordin R, Renner K (1991) Anatomic considerations for plate-screw fixation of the cervical spine. Spine 16(10 Suppl):548–551
Kurd MF, Millhouse PW, Schroeder GD, Kepler CK, Vaccaro AR (2015) Lateral mass fixation in the subaxial cervical spine. J Spinal Disord Tech 28(7):259–263. doi:10.1097/BSD.0000000000000302
Sekhon LH (2005) Posterior cervical lateral mass screw fixation: analysis of 1026 consecutive screws in 143 patients. J Spinal Disord Tech 18(4):297–303
Ebraheim NA, Xu R, Yeasting RA (1996) The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. Spine 21(11):1291–1295
Abdullah KG, Nowacki AS, Steinmetz MP, Wang JC, Mroz TE (2011) Factors affecting lateral mass screw placement at C-7. J Neurosurg Spine 14(3):405–411. doi:10.3171/2010.11.SPINE09776
Takeshita K, Murakami M, Kobayashi A, Nakamura C (2001) Relationship between cervical curvature index (Ishihara) and cervical spine angle (C2--7). J Orthop Sci 6(3):223–226
Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Machino M, Ito ZY, Matsuyama Y (2008) Postoperative changes in spinal cord signal intensity in patients with cervical compression myelopathy: comparison between preoperative and postoperative magnetic resonance images. J Neurosurg Spine 8(6):524–528. doi:10.3171/SPI/2008/8/6/524
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K (1981) Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 6(4):354–364
Eskander MS, Balsis SM, Balinger C, Howard CM, Lewing NW, Eskander JP, Aubin ME, Lange J, Eck J, Connolly PJ, Jenis LG (2012) The association between preoperative spinal cord rotation and postoperative C5 nerve palsy. J Bone Joint Surg Am 94(17):1605–1609
Ryken TC, Heary RF, Matz PG (2009) Cervical laminectomy for the treatment of cervical degenerative myelopathy. J Neurosurg Spine 11(2):142–149. doi:10.3171/2009.1.SPINE08725
Mikawa Y, Shikata J, Yamamuro T (1987) Spinal deformity and instability after multilevel cervical laminectomy. Spine 12(1):6–11
Guigui P, Benoist M, Deburge A (1998) Spinal deformity and instability after multilevel cervical laminectomy for spondylotic myelopathy. Spine 23(23):440–447
Raab P, Juergen K, Gloger H, Soerensen N, Wild A (2008) Spinal deformity after multilevel osteoplastic laminotomy. Int Orthop 32(3):355–359
Luo J, Cao K, Huang S, Li L, Yu T, Cao C, Zhong R, Gong M, Zhou Z, Zou X (2015) Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J 24(8):1621–1630. doi:10.1007/s00586-015-3911-4
Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC (2014) The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine 39(4):280–285. doi:10.1097/BRS.0000000000000133
Zhang YP, Xu QF, Lu LJ, Li J, Hong JJ (2015) Application of the pedicle screw in the subaxial cervical spine. Zhongguo Gu Shang 28(2):126–129
Neo M, Sakamoto T, Fujibayashi S, Nakamura T (2005) The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine 30(24):2800–2805
Kotani Y, Abumi K, Ito M, Minami A (2003) Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg 99(3 Suppl):257–263
Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, Ploumis A, Xenakis TA (2012) Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 21(2):247–255. doi:10.1007/s00586-011-2011-3
Xu R, Haman SP, Ebraheim NA, Yeasting RA (1999) The anatomic relation of lateral mass screws to the spinal nerves. A comparison of the Magerl, Anderson, and An techniques. Spine 24(19):2057–2061
Tessitore E, El-Hassani Y, Schaller K (2011) How I do it: cervical lateral mass screw fixation. Acta Neurochir 153(8):1695–1699. doi:10.1007/s00701-011-1068-4
Acknowledgements
We thank all patients who took part in this study and the information provided by all of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have read and contributed to the submitted manuscript and have no conflict of interest to declare.
Funding
There is no funding source.
Ethical approval
This study was approved by the Institutional Ethics Board of the 3rd Hospital of Hebei Medical University.
Additional information
Di Zhang and Xianda Gao contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, D., Gao, X., Jiang, J. et al. Safe placement of lateral mass screw in the subaxial cervical spine: a case series. International Orthopaedics (SICOT) 41, 781–788 (2017). https://doi.org/10.1007/s00264-017-3423-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3423-4