Abstract
Purpose
γ9δ2 T lymphocytes have been shown to be directly cytotoxic against renal carcinoma cells. Lymphocytes T γδ can be selectively expanded in vivo with BrHPP (IPH1101, Phosphostim) and interleukin 2 (IL-2). A phase I Study was conducted in patients with metastatic renal cell carcinoma (mRCC) to determine the maximum-tolerated dose and safety of Innacell γδ™, an autologous cell-therapy product based on γ9δ2 T lymphocytes, in patients with mRCC.
Experimental design
A 1-h intravenous infusion of γ9δ2 T lymphocytes was administered alone during treatment cycle 1 and combined with a low dose of subcutaneous interleukin-2 (IL-2, 2 MIU/m2 from Day 1 to Day 7) in the two subsequent cycles (at 3-week intervals). The dose of γ9δ2 T lymphocytes was escalated from 1 up to 8 × 109 cells.
Results
Ten patients underwent a total of 27 treatment cycles. Immunomonitoring data demonstrate that γ9δ2 T lymphocytes are initially cleared from the blood to reappear at the end of IL-2 administration. Dose-limiting toxicity occurred in one patient at the dose of 8 × 109 cells (disseminated intravascular coagulation). Other treatment-related adverse events (AEs) included mainly gastrointestinal disorders and flu-like symptoms (fatigue, pyrexia, rigors). Hypotension and tachycardia also occurred, especially with co-administered IL-2. Six patients showed stabilized disease. Time to progression was 25.7 weeks.
Conclusion
The data collected in ten patients with mRCC indicate that repeated infusions of Innacell γδ™ at different dose levels (up to 8 × 109 total cells), either alone or with IL-2 is well tolerated. These results are in favor of the therapeutic value of cell therapy with Innacell γδ™ for the treatment of cancers.
Similar content being viewed by others
Introduction
Several signs point toward a possible immunologic disturbance at the origin of development of mRCC. Among these are reported cases of spontaneous regression of metastatic lesions, the presence of cytolytic T lymphocytes in renal tumors, and recent descriptions of tumor-associated antigens on renal cancer cells [2]. In line with these observations, much attention has been focused on immunotherapy, using mainly α-interferon (IFN-α), interleukin-2 (IL-2) or both. However, although tumor regressions were observed in 10–15% of patients with mRCC [9, 14], randomized trials demonstrated only a modest survival advantage through treatment with these cytokines [2, 12], at the cost of relatively severe toxic effects [12].
T-cell infiltrates in renal tumors, characterizing the host local antitumor immune response, involve conventional and non-conventional (i.e., non-MHC-restricted) effector cells, the latter constituting the innate immune response. Among the non-conventional immune effectors, γδ T lymphocytes (i.e., T lymphocytes carrying a γδ T-cell surface antigen receptor) represent a minor subset of human peripheral T cells (less than 10%). These cells are potent and are rapid producers of IFN-γ and TNF-α in response to bacterial antigens and to ligands expressed on tumor cells. They have been shown to exert a lytic potential against different tumor cells both in vitro [6, 17] and in vivo in animals after an adoptive transfer of ex vivo expanded human cells [24]. In patients with RCC, γδ T lymphocytes in peripheral blood were found to increase with increasing cancer stage and decrease after surgical resection of the tumor, suggesting that γδ T cells recognize certain RCC-related antigens and play a role in the surveillance against RCC [7].
Most human peripheral γδ T cells display the disulfide-linked γ9δ2 receptor and express the CD45RO+CD95+ effector/memory phenotype [13], while lacking CD4 and CD8 expressions. Activation of γ9δ2 T cells can be induced by non-peptidic natural and synthetic small molecular-weight phosphorylated compounds, through a non-MHC-restricted mechanism. One such synthetic compound, easily synthesized and active at nanomolar concentrations similarly to natural phosphoantigens, is bromohydrin pyrophosphate (BrHPP, IPH1101 Phosphostim®) [5]. In monkeys, BrHPP, particularly when combined with low doses of IL-2, was shown to induce a strong activation and amplification of γ9δ2 T cells accompanied by the production of considerable amounts of cytokines, with no associated toxicity [18]. Finally, peripheral γ9δ2 T cells from mRCC patients, activated and expanded in vitro with BrHPP, were found to exert a selective lytic potential toward autologous primary renal cell carcinoma lines, confirming γ9δ2 effectors as a promising approach for the treatment of mRCC [21].
The present Phase-I clinical study is aimed primarily to determine the maximum-tolerated dose of a γ9δ2 cell therapy product named Innacell γδ™ in mRCC patients. Innacell γδ™ is manufactured in vitro from an autologous peripheral blood mononuclear cell (PBMC) preparation, by a single stimulation with BrHPP followed by a 2-week period of culture and expansion with IL-2. Innacell γδ™ contains 95% of T lymphocytes, of which a high proportion (mean of 76% of total cell number) is of the γ9δ2 phenotype and a low proportion of the αβ phenotype, and a small minority of other cells of different phenotypes (mainly 4% of NK cells). Effector/memory (CD27-CD45RA-) T cells represent more than 90% of γ9δ2 cells. A secondary objective of the study was to gain preliminary information on the effectiveness of Innacell γδ™ against mRCC. Tolerability and effectiveness of Innacell γδ™ were evaluated after administration of the cell-therapy product either by itself, or in combination with repeated injections of a low dose of Il-2, sufficient to induce activation of γ9δ2 cells. The co-injection of IL-2 is required for the survival and efficacy of the cells injected in vivo as shown by previous cell therapy studies using T cell clones [23]. An additional objective was to examine the persistence of γ9δ2 cells in the blood and the evolution of other cell populations (immunomonitoring) as well as the potential effect of IL-2 administrations on these outcome measures.
Patients and methods
Patient selection
Patients with a histological-documented mRCC and at least one measurable or evaluable metastasis not localized in the irradiated area were candidates for the study. Failure of a preceding treatment had to be demonstrated through radiology. Other inclusion criteria included patients aged 18 years or older who have signed an informed consent, with a performance status of 0 to 2 with Eastern Cooperative Oncology Group (ECOG) as well as negative tests for HIV and B or C hepatitis. Patients who were excluded were those with the following cases: presence of brain metastases, other primary cancers, diagnosed and not cured, treatment with chemotherapy or immunotherapy in the last 6 weeks or ongoing anticancer treatment, previous organ allografts, contraindication to leukapheresis, hypersensitivity to IL-2, systemic infection, autoimmune disease, weak heart, liver, bone marrow, or kidney functions, also in the case of pregnancy or lactation. Immunosuppressive agents (cyclosporine, corticosteroids) were not authorized.
In addition, to be included in the study, patients had to demonstrate lymphocyte expansion in response to a single in vitro stimulation with BrHPP (“sensitivity test” defined as positive if amplification was >10, enrichment of the population of γ9δ2 cells was at least 70% with cell viability of at least 70%) in a preliminary test.
The study protocol was approved by the Independent Ethics Committee of Nantes, France and by the French National Committee of Cell Therapy. The study was conducted in compliance with the principles laid down by Good Clinical Practice (GCP) and the Declaration of Helsinki with subsequent amendments. Written informed consent was obtained from each patient before enrolment and completion of any study procedure.
Innacell γδ™
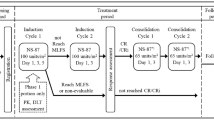
The cell therapy product Innacell γδ™, was manufactured in vitro, from a cryopreserved autologous peripheral blood mononuclear cells (PBMC) obtained by leukapheresis, as described [16], see Fig. 1. PBMC were stimulated with 3 μM BrHPP (IPH1101-Phosphostim 200TM, Innate Pharma, Marseille, France) at 1.2 × 106 cells/ml in RPMI1640 (Cambrex Biosciences, Verviers, Belgium) supplemented with 9% fetal calf serum (FCS; HyClone, Erembodegem, Belgium) and 20 ng/ml IL-2 (Proleukin®, Chiron Therapeutics, Emeryville CA, USA) (day of stimulation) or 60 ng/ml IL-2 (days 4–14 of culture). The use of FCS in ex vivo clinical preparations is permitted by the French National Committee for Cell Therapy. On culture day 15, the Innacell γδ(( cell therapy product were harvested from culture, washed with buffered saline (0.9% NaCL, pH 7; Braun Medical, Boulogne, France), resuspended at a concentration of 10–100 × 106 cells/ml in 4% human serum albumin solution (4% Vialebex, LFB Laboratory, Courtaboef, France), and stored at +5 ± 3°C. Innacell γδ(( infusions were administered within 24 h of release.
Innacell γδ™ characteristics
The cell therapy product contains 95% (range 86–99%) of CD3+ cells, of which the majority, namely, 76 (range 21–96%) is of the γ9δ2 phenotype; only 18 (range 2–56%) is TCR αβ(positive, and a small minority, 4% (range 0–12%) are NK cells. More than 90% of γ9δ2 T cells is of the Effector/memory (CD27-CD45RA-) phenotype.
Treatment plan, Innacell γδ™ dose and mode of administration
This was a two-center (Centre René Gauducheau, Nantes, France; Centre Léon Bérard, Lyon, France), open-label, phase-I study conducted in patients with mRCC. Innacell γδ™ (γ9δ2 cell therapy product) was administered via a central venous line for approximately 1 hour at a maximum flow rate of 3 ml/min. Each patient was to receive three infusions at 21-day intervals of the same dose of Innacell γδ™. During the first cycle, the patients received Innacell γδ™ without IL-2 co-administration. During cycles 2 and 3, the patients received morning and evening subcutaneous injections of IL-2 (2 × 106 IU/m²/day) for 7 days, the first injection being made 0.5 h prior to Innacell γδ™ infusion (cf. Fig. 1: Patient treatment schedule).
Four dose levels of Innacell γδ™ (1, 4, 8, and 12.109 cells) were planned to be tested in ascending order, depending on treatment tolerability. The maximum dose to be administered in the absence of dose-limiting toxicity (DLT; 12 × 109 cells) corresponds to the maximum amount of cells that can be industrially manufactured. In the absence of dose-limiting toxic effects, only one patient was to be treated at the first dose level. At least three patients were to be treated at the second and subsequent dose levels. Toxicity was assessed using the National Cancer Institute of Canada Common Toxicity Criteria version 2.0 [3]. DLT was defined as any one of the following: nadir neutrophils <0.5 × 109/l lasting 7 days or <0.1 × 109/l lasting 3 days; thrombocytopenia < 25 × 109/l or thrombocytopenia with bleeding or requiring platelet transfusion; febrile neutropenia was defined as absolute neutrophil count < 0.5 × 109/L and fever (three measured temperatures <38°C in 24 h or one >38.5°C); and/or any grade 3/4 major organ toxicity except alopecia or nonpremedicated nausea/vomiting. The maximum-tolerated dose (MTD) of Innacell γδ™ was defined as the highest-validated dose, i.e., with DLT in no more than one out of three, or two out of six patients. There was no intra-patient dose escalation.
Pretreatment and follow-up examinations
Prior to the inclusion, patients were evaluated after study of their complete medical history and a thorough physical examination (measurement of body weight, height, ECOG performance status, vital signs, examination of body systems). An electrocardiogram (ECG) and comprehensive laboratory tests (hematology, serum electrolytes, hepatic and renal function) were also performed. During the treatment period, laboratory tests were performed at each weekly visit.
Efficacy assessments
Tumor response to study treatment (complete (CR) or partial (PR) response, stable (SD) or progressive (PD) disease) was assessed on the basis of radiological examinations performed at inclusion and at 4 weeks, 8 weeks and 4 months after the last Innacell γδ™ infusion. Tumor response was to be analyzed according to the RECIST criteria [19]. In the case of SD, the relevant criteria had to be confirmed no less than 6 weeks after treatment beginning. Individual time to progression was appraised in connection with the estimated prognostic risk level according to Motzer’s score [10].
Immunomonitoring
The immunomonitoring measurements carried out aimed (1) to assess the persistence of γ9δ2 T cells in peripheral blood after each Innacell γδ™ infusion and the possible influence of IL-2 co-administration, and (2) to monitor the other subpopulations in peripheral blood to assess the pharmacodynamic outcomes of the therapy. Blood samples for immunomonitoring were taken within 6 h before and at different times up to 10 days after each Innacell γδ™ infusion. Patient peripheral blood cells were collected on EDTA. Whole blood cells, measuring 100 μL was incubated with mAbs for 10 min, washed in PBS buffer, lysed with 500 μl of immunolyse (Beckman Coulter), washed and fixed with 1% paraformaldehyde in PBS. Monoclonal antibodies and analysis method used were described in our previous publications [16].
Descriptive statistics
Quantitative variables were summarized by the number of observations, mean and standard deviation or median and range. Categorical variables were summarized by the number of observations and relative frequencies in the corresponding categories. Median time to progression was estimated by the Kaplan–Meier method.
Results
Patient sample
Between October 2002 and September 2005, 36 patients were screened for entry to the trial: 32 patients at the Nantes center and 4 at the Lyon center. Of these patients, 26 were not entered into the trial. The reason for non-inclusion was mainly the absence of lymphocyte response in vitro in the BrHPP expansion test (17 patients). Other reasons were non-conformity of Innacell γδ™ before treatment (three patients), deterioration of performance status (three patients), report of one exclusion criteria, decision of the investigator, and decision of the patient for one patient each. The treated patient population thus involved ten patients.
Baseline characteristics at inclusion and main disease characteristics of the patients included are presented in Table 1. Among them, seven patients had been treated with immunotherapy (IFN-α and/or IL-2) alone or in combination with chemotherapy and prognostic risk as evaluated by the Motzer’s score was poor or intermediate for six patients (Table 2).
Study progress
The ten patients included received a total of 27 different batches of Innacell γδ™ in three dose levels (Table 3). One patient treated at the lowest dose level (1 × 109 cells) did not exhibit DLT. Dose-escalation, thus proceeded to the next higher main dose level (4 × 109 cells). At this dose level, one patient received only one dose of Innacell γδ™ due to disease progression, one patient received an overdose (6 × 109 cells) at the third administration with an unacceptable toxicity (grade 3 hypotension), and one patient received an underdose (2.8 × 109 cells, third administration) without toxicity. As these patients were not assessable for MTD determination, three additional patients were treated at the 4 × 109 dose level; none of these patients experienced DLT. The following group of three patients was treated at the next dose level (8 × 109 cells): one patient experienced DLT after the second administration as described below.
The dose-escalation strategy would have then required testing the same dose level in a new cohort of three patients. However, recruitment of patients for the study was stopped at this point for ethical reasons and on the grounds of recent availability of targeted therapies for mRCC with acknowledged effectiveness (e.g., tyrosine kinase inhibitors) [11, 15].
Four patients were withdrawn prematurely from the study, three due to progression of the disease, and one for DLT at the dose of 8 × 109 cells (disseminated intravascular coagulation). Overall, among 27 cycles delivered, 22 were evaluable for MTD (Table 3).
For 8 of the 10 patients, duration on study treatment was at least 60 days. Duration of follow-up after study end was at least 10 weeks for 8 patients.
Dose limiting toxicity
A 73-year-old male patient had polymetastatic disease (lung, liver and adrenal gland metastases). The first infusion of Innacell γδ™ (8 × 109 cells) was well tolerated (grade 1 fever and chills). The second infusion (Innacell γδ™ + IL-2) was followed by hypotension (88/66 mmHg), thrombopenia (grade 2) and coagulation abnormalities (prothrombin index: 46%; activated partial thromboplastin time––aPTT––ratio: 1.57; decreased coagulation factors II, VII and X; presence of fibrin degradation products in plasma). The absence of any clinical sign led to the diagnosis of biologically disseminated intravascular coagulation. The biological test returned to normal within 24 h after platelet and plasma transfusion. The other case of unacceptable toxicity––grade 3 hypotension––noted during the study occurred during a non-assessable cycle because of overdosage (see above). This patient also developed a deep-vein thrombosis with pulmonary embolism and the relationship with the treatment could not be excluded.
As no additional patients were treated at the dose level of 8 × 109 cells, the study having been closed at this point for external reasons (see above), the MTD of Innacell γδ™ could not be determined precisely from the data of the present study, but was at least of 4 × 109 cells.
Other clinical adverse events
At all doses, treatment with Innacell γδ™ alone (cycle 1) was well tolerated (Table 4). The most frequent AEs occurred during concomitant treatment with IL-2 (cycles 2 and 3). Main AEs were grade 1 or grade 2 flu-like symptoms: chills, fever, fatigue and gastrointestinal symptoms. These transient toxicity signs of flu-like symptoms suggest a cytokine-release syndrome.
Immunomonitoring
In the nine patients with assessable data, γ9δ2 T cells were initially cleared from the circulating blood during the first 2 days following infusion of Innacell γδ™ (Fig. 2). After infusions 2 and 3 (with co-administered IL-2), the initial decrease was more pronounced and prolonged, and the values noted at Day 7 and Day 10 were considerably (two to fourfold) higher than the corresponding baseline values. However, the percentage of γ9δ2 T cells relative to the total number of lymphocytes generally showed only small and inconsistent variations. As shown in Fig. 3, without co-administered IL-2 (infusion 1), fold increase (relative to baseline at start of cycle 1) was only slightly affected except after infusion of the dose of 8 × 109 cells (initial reduction followed by an increase). With co-administered IL-2 (infusions 2 and 3), there was a dramatic initial reduction followed by a marked increase in fold increase and the variations observed were related to the dose of Innacell γδ™ administered. Concerning specific characteristics observed during the study, only one patient showed a significant expansion (fold increase × 30) of the NK population during the third infusion of Innacell with IL-2 treatment.
Efficacy
The best overall response rate according to RECIST criteria that was recorded after treatment with Innacell γδ™ was SD for six patients (60%) and PD for four patients (40%). Individual Time to progression according to the dose level of Innacell γδ™ is displayed in Table 2. The maximal individual percent change in the sum of the longest diameter of target lesions was observed in two patients treated with 4 or 8 × 109 cells showing substantial tumor shrinkage at the 14-week evaluation (−22 and −48%, respectively). These shrinkages were not confirmed as recommended by RECIST criteria. According to the Kaplan–Meier method, illustrated in Fig. 4, median time to progression was 25.7 weeks.
Discussion
RCC is an immunosensitive cancer; however, conventional immunotherapy has not provided major advances in mRCC therapy. Therefore, some elements of the immune system with strong anti-tumor properties such as the cytotoxic γ9δ2 human T lymphocytes, deserve particular attention.
Innacell γδ™ was used in the present phase I trial to evaluate its safety and tolerability profile and secondarily its therapeutic potential in patients with mRCC. At the two first-dose levels (1 and 4 × 109 cells) Innacell and IL-2 coadministration was well tolerated without DLT. Of note, one patient treated in the medium-dose group who received an overdose of Innacell γδ™ (6 × 109 cells) exhibited a toxic effect (grade 3 hypotension). At the dose level 8 × 109 total cells, one patient experienced grade 3 biological disseminated intravascular coagulation. This study was stopped for ethical reasons (availability of tyrosine-kinase inhibitors on the therapeutic arena) so that the MTD Innacell γδ™ cannot be precisely determined. Nevertheless, the dose of 4 × 109 cells was correctly evaluated in the present study and showed good safety and tolerability.
Let alone the DLT experienced by one patient treated with Innacell γδ™ at the dose of 8 × 109 total cells, and the adverse effect that occurred in a patient who received an overdose of γ9δ2 T cells, the AEs recorded were relatively mild and were noted mainly during treatment cycles 2 and 3 when Innacell γδ™ was administered with co-administration of IL-2. The signs and symptoms most frequently reported (fatigue, fever, hypotension, gastrointestinal disorders) are suggestive of the cytokine-release syndrome commonly encountered after administration of interleukins. Activated γ9δ2 T lymphocytes themselves can produce high amounts of cytokines, which, in synergy with co-administered IL-2, may cause flu-like symptoms. In this connection, a parallel can be drawn between the present study and the pilot study recently carried out by Kobayashi et al. [8], with adoptive therapy using γδ T cells in seven patients with advanced RCC. These authors administered autologous γδ T cells (∼3 × 109 cells) activated in vitro with a phosphoantigen in association with concomitant infusions of recombinant human IL-2 every week or every other week for 12 weeks in co-treated patient with pamidronate [8]. Similar to Kobayashi et al. [8], a decrease in lymphocyte count was observed in a proportion of our patients, which may indicate lymphocyte trapping in tissues as a result of some treatment-immune effects. Among the 36 patients screened in the study, only 10 have been treated. The screening was based on a BrHPP expansion test performed in order to determine the feasibility and the cell culture parameters of the targeted specific T-cell expansion. According to previously published observations [20], based on the percentage of δ2+ T cells observed on Day 14 of culture, RCC patients can be grouped into three subsets: the high-sensitivity subset represents about 50% of RCC patients, whereas the intermediate- and low-sensitivity subsets represent about 25% each. Healthy volunteers were analyzed in parallel, of whom 91% display a high-sensitivity status, do not present any low-sensitivity subset, suggesting that the low-sensitivity status is specific to (m)RCC patients. This phenomenon is congruent with the selection of the best sensitive patients for inclusion into the present study.
As regards the assessment of Innacell γδ™ efficacy for the treatment of mRCC, the limited number of patients treated in this phase I study as well as the absence of a control group do not allow drawing any firm conclusion. For ethical reasons, this was the first time that Innacell γδ™ was administered to patients. The patients recruited for the study had generally advanced disease and failed to standard therapy. They are not necessarily representative of the true target population of Innacell γδ™ which may be more indicated for the treatment of residual lesions after standard therapy. Innacell γδ™ indeed intends to restimulate the immune system in a different fashion from the formerly used vaccines and to act as an adjuvant in conjunction with standard chemotherapies or administration of antiangiogenic agents [21]. This is the first time that targeted innate lymphocytes could be selectively activated, which can play a role on the tumor either directly with the expansion of the cytotoxic effector or by an indirect effect through restimulation of adaptive immunity. Finally, the objectives of this Phase I study to primarily determine the maximum-tolerated dose of Innacell γδ™ were not met as the conditions were not quite adapted to the demonstration of Innacell γδ™ anticancer effectiveness in real-world settings.
Nevertheless, tumor shrinkage (−22 and −48%) was observed in two patients. Even though one tumor shrinkage cannot be qualified as a PR, this can be correlated with the disease stabilization observed in 6 patients (60%) treated with Innacell γδ™. The median time to progression of patients treated with Innacell γδ™ was 25.7 weeks, compared with 12–13 weeks in mRCC patients receiving placebo in other studies [4, 22]. Moreover, of the seven patients who had an end-of-study visit after 2 months (1 patient) or 4 months after the last Innacell γδ™ infusion, four patients showed no change in ECOG-PS score from baseline and three patients a decrease of one score unit. Comparable efficacy results were obtained in the study of Kobayashi et al. [8], with three of five patients exhibiting prolongation of tumor-doubling time and better survival in patients responding well to the stimulating antigen compared with poor responders.
Immunomonitoring results show that γ9δ2 cells are initially cleared from blood during the first 2 days after Innacell γδ™ infusion and that their number progressively increases afterwards. This bi-phasic course is classically observed with IL-2 co-administration and assumed to be due to transient lymphocyte margination in tissues. Finally, 1 week after Innacell γδ™ infusion (i.e., at the end of IL-2 administrations) at the dose of 4 or 8 × 109 cells, the number of circulating γ9δ2 T cells is up to two to fourfold higher than at baseline, which indicates amplification of γ9δ2 T cells by IL-2.
In conclusion, the data collected in this study of patients with advanced RCC indicate that repeated infusions of Innacell γδ™ either alone or with co-administration of IL-2 is well tolerated up to the dose of 4 × 109 γ9δ2 cells. The maximum-tolerated dose could not be determined though, due to discontinuation of the study following the recent availability of new therapies (tyrosine kinase inhibitors) in mRCC. Regarding Innacell γδ™ efficacy, time to progression appeared more prolonged in this group of patients treated with Innacell γδ™ than in placebo-receiving groups of patients with renal cell carcinoma reported in the literature. Innacell γδ™ thus retains valuable potential for further evaluation in mRCC and the treatment of other types of cancer refractory to conventional treatments. It will therefore be assessed, starting at the dose of 6 × 109 γ9δ2 cells, in other clinical situations, where no effective treatment is yet available. Despite the relative complexity of cell therapy, such treatment may have a role, in conjunction with other therapies, in the treatment of cancers refractory to conventional treatments alone. In the near future, immunotherapy should be considered in association with tyrosine kinase inhibitors for appropriately selected patients. Indeed, recent prospective studies suggest that the potential exists for identifying predictors of immunotherapy response in patients with good or intermediate prognosis [1].
References
Atkins M, Regan M, McDermott D, Mier J, Stanbridge E, Youmans A, Febbo P, Upton M, Lechpammer M, Signoretti S (2005) Carbonic anhydrase IX expression predicts outcome of interleukin-2 therapy for renal cancer. Clin Cancer Res 11:3714–21
Bukowski RM (2001) Cytokine therapy for metastatic renal cell carcinoma. Semin Urol Oncol 19:148–54
Common Toxicity Criteria (CTC) (1999) Cancer Therapy Evaluation Program. Common Toxicity Criteria, version 2.0. DCTD, NCI, NIH, DHHS
Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, Rolland F, Demkow T, Hutson TE, Gore M, Freeman S, Schwartz B, Shan M, Simantov R, Bukowski RM; TARGET Study Group (2007) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356:125–134
Espinosa E, Belmant C, Pont F, Luciani B, Poupot R, Romagné F, Brailly H, Bonneville M, Fournié JJ (2001) Chemical synthesis and biological activity of bromohydrin pyrophosphate, a potent stimulator of human γδ T cells. J Biol Chem 276:18337–18344
Kato Y, Tanaka Y, Miyagawa F, Yamashita S, Minato N (2001) Targeting of tumor cells for human γδ T cells by nonpeptide antigens. J Immunol 167:5092–5098
Kobayashi H, Tanaka Y, Yagi J, Toma H, Uchiyama T (2001) Gamma/delta T cells provide innate immunity against renal cell carcinoma. Cancer Immunol Immunother 50:115–124
Kobayashi H, Tanaka Y, Yagi J, Osaka Y, Nakazawa H, Uchiyama T, Minato N, Toma H (2006) Safety profile and anti-tumor effects of adoptive immunotherapy using gamma-delta T cells against advanced renal cell carcinoma: a pilot study. Cancer Immunol Immunother 56:469–476
Medical Research Council Renal Cancer Collaborators (1999) Interferon-α and survival in metastatic renal carcinoma: early results of a randomised controlled trial. Lancet 353:14–17
Motzer RJ, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J (1999) Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol 17:2530–2540
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, Baum CM, Figlin RA (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356:115–124
Negrier S, Escudier B, Lasset C, Douillard JY, Savary J, Chevreau C, Ravaud A, Mercatello A, Peny J, Mousseau M, Philip T, Tursz T (1998) Recombinant human interleukin-2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma. N Engl J Med 338:1272–1278
Poccia F, Boullier S, Lecoeur H, Cochet M, Poquet Y, Colizzi V, Fournie JJ, Gougeon ML (1996) Peripheral V gamma 9/V delta 2 T cell deletion and anergy to nonpeptidic mycobacterial antigens in asymptomatic HIV-1-infected persons. J Immunol 157:449–461
Pyrhönen S, Ellmén J, Vuorinen J, Gershanovich M, Tominaga T, Kaufmann M, Hayes DF (1999) Prospective randomized trial of interferonalfa-2a plus vinblastine versus vinblastine alone in patients with advanced renal cell cancer. J Clin Oncol 17:2859–2867
Reddy GK, Bukowski RM (2006) Sorafenib: recent update on activity as a single agent and in combination with interferon-alpha2 in patients with advanced-stage renal cell carcinoma. Clin Genitourin Cancer 4:246–248
Salot S, Laplace C, Saïagh S, Bercegeay S, Tenaud I, Cassidanius A, Romagne F, Dreno B, Tiollier J (2007) Large scale expansion of g9d2 T lymphocytes: Innacell gd™ cell therapy product. J Immunol Methods 326:63–75
Sicard H, Al Saati T, Delsol G, Fournie JJ (2001) Synthetic phosphoantigens enhance human Vγ9Vδ2 T lymphocytes killing of non-Hodgkin’s B lymphoma. Mol Med 7:711–22
Sicard H, Ingoure S, Luciani B, Serraz C, Fournié JJ, Bonneville M, Tiollier J, Romagné F (2005) In vivo immunomanipulation of Vγ9Vδ2 T cells with a synthetic phosphoantigen in a preclinical nonhuman primate model. J Immunol 175:5471–80
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Viey E, Fromont G, Escudier B, Morel Y, Da Rocha S, Chouaib S, Caignard A (2005) Phosphostim-activated γδ T cells kill autologous metastatic renal cell carcinoma. J Immunol 174:1338–1347
Viey E, Laplace C., Escudier B (2005) Peripheral γδ T lymphocytes as an innovative tool in immunotherapy for metastatic renal cell carcinoma. Expert Rev Anticancer Ther 5:973–86
Yang JC, Haworth L, Sherry RM, Hwu P, Schwartzentruber DJ, Topalian SL, Steinberg SM, Chen HX, Rosenberg SA (2003) A randomised trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cell cancer. N Engl J Med 349:427-434
Yee C, Thompson JA, Roche P, Byrd D, Lee P, Piepkorn M, Kenyon K, Davis M, Riddell S, Greenberg P (2000) Melanocyte destruction after antigen-specific immunotherapy of Melanoma: direct evidence of T cell-mediated vitiligo. J Exp Med 192:1637–1643
Zheng BJ, Ng SP, Chua DT, Sham JS, Kwong DL, Lam CK, Ng MH (2002) Peripheral gamma delta T-cell deficit in nasopharyngeal carcinoma. Int J Cancer 99:213–217
Acknowledgments
Grand support: Innate Pharma SAS, Marseille, France.
Conflict of interest
Consultancy Agreement: Jaafar Bennounax. Clinical Investigator: Emmanuelle Bompas, Eve Marie Neidhardt, Frédéric Rolland, Irène Philip, Sylvie Négrier. Innate Pharma personnel: Céline Galéa, Samuel Salot, Sylvie Lafaye-de Micheaux, Jérôme Tiollier.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bennouna, J., Bompas, E., Neidhardt, E.M. et al. Phase-I study of Innacell γδ™, an autologous cell-therapy product highly enriched in γ9δ2 T lymphocytes, in combination with IL-2, in patients with metastatic renal cell carcinoma. Cancer Immunol Immunother 57, 1599–1609 (2008). https://doi.org/10.1007/s00262-008-0491-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-008-0491-8