Abstract
Purpose
To examine the safety, feasibility, and oncologic control following percutaneous image-guided thermal ablation of hepatocellular carcinoma (HCC) in a transplanted allograft.
Materials and Methods
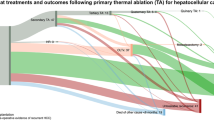
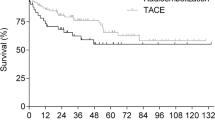
Retrospective review was performed to identify patients who underwent liver transplantation for HCC and subsequently underwent percutaneous hepatic thermal ablation for recurrent HCC within the allograft between January 1st, 2000-September 1st, 2016. Eleven patients with hepatic allograft HCC underwent twelve percutaneous thermal ablation procedures to treat 16 lesions. Patient, procedural characteristics, and local oncologic efficacy were reviewed. Complications were characterized via the Common Terminology for Clinically Adverse Events nomenclature [CTCAE] v4.03).
Results
Eleven transplant recipients underwent treatment of 16 HCC tumors in their allografts during 12 ablation sessions. Mean follow-up time was 25 months (range 2–96 months). Local oncologic control was achieved in 10 of 11 tumors (91%) with imaging follow-up. One patient (8%) with Roux-en-Y biliary reconstruction developed a major complication with hepatic abscess.
Conclusion
Thermal ablation of recurrent HCC in transplanted allografts can be accomplished safely with acceptable rates of local control for patients with duct-to-duct biliary reconstruction. Due to the high number of patients deemed surgically unresectable, the morbidity of surgical resection, the side effects of targeted therapies, and significant mortality associated with recurrences in the transplanted allograft, patients may benefit from percutaneous thermal ablative treatments. Further study is needed to assess the role of thermal ablation in allograft HCC recurrences as primary therapy or in a multimodality approach with emerging systemic therapies.
Similar content being viewed by others
References
Clavien PA, et al. (2012) Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol 13(1):e11–e22
de’Angelis N, et al. (2015) Managements of recurrent hepatocellular carcinoma after liver transplantation: a systematic review. World J Gastroenterol 21(39):11185–11198
Mazzaferro V, et al. (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334(11):693–699
Rubin J, et al. (2012) Management of recurrent hepatocellular carcinoma in liver transplant recipients: a systematic review. Exp Clin Transplant 10(6):531–543
Schwartz M (2004) Liver transplantation for hepatocellular carcinoma. Gastroenterology 127(5 Suppl 1):S268–S276
Yao FY, et al. (2002) Liver transplantation for hepatocellular carcinoma: comparison of the proposed UCSF criteria with the Milan criteria and the Pittsburgh modified TNM criteria. Liver Transplant 8(9):765–774
Clark ME, Smith RR (2014) Liver-directed therapies in metastatic colorectal cancer. J Gastrointest Oncol 5(5):374–387
de Baere T, et al. (2003) Adverse events during radiofrequency treatment of 582 hepatic tumors. AJR 181(3):695–700
Foltz G (2014) Image-guided percutaneous ablation of hepatic malignancies. Semin Interventional Radiol 31(2):180–186
Murata S, et al. (2014) Interventional treatment for unresectable hepatocellular carcinoma. World J Gastroenterol 20(37):13453–13465
Saied A, Katz SC, Espat NJ (2013) Regional hepatic therapies: an important component in the management of colorectal cancer liver metastases. Hepatobiliary Surg Nutr 2(2):97–107
Solbiati L, et al. (2012) Small liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-up. Radiology 265(3):958–968
Sucandy I, et al. (2016) Longterm survival outcomes of patients undergoing treatment with radiofrequency ablation for hepatocellular carcinoma and metastatic colorectal cancer liver tumors. HPB 18(9):756–763 ((Oxford))
Gringeri E, et al. (2014) Laparoscopic microwave thermal ablation for late recurrence of local hepatocellular carcinoma after liver transplant: case report. Prog Transplant 24(2):142–145
Ho CK, Chapman WC, Brown DB (2007) Radiofrequency ablation of recurrent hepatocellular carcinoma in a patient after liver transplantation: two-year follow-up. J Vasc Interv Radiol 18(11):1451–1453
Choi D, et al. (2005) Liver abscess after percutaneous radiofrequency ablation for hepatocellular carcinomas: frequency and risk factors. AJR 184(6):1860–1867
Elias D, et al. (2006) Liver abscess after radiofrequency ablation of tumors in patients with a biliary tract procedure. Clin Biol Gastroenterol 30(6–7):823–827
Fonseca AZ, et al. (2014) Complications of radiofrequency ablation of hepatic tumors: frequency and risk factors. World J Hepatol 6(3):107–113
Iida H, et al. (2014) Risk of abscess formation after liver tumor radiofrequency ablation: a review of 8 cases wtih a history of enterobiliary anastomosis. Hepato 61(135):1867–1870
Odisio BC, et al. (2016) Use of prophylactic antibiotics to prevent abscess formation following hepatic ablation in patients with prior enterobiliary manipulation. J Gastrointest Surg 20(8):1428–1434
Shibata T, et al. (2003) Cholangitis and liver abscess after percutaneous ablation therapy for liver tumors: incidence and risk factors. J Vasc Interv Radiol 14(12):1535–1542
Welch BT, et al. (2017) Evaluation of infectious complications following percutaneous liver ablation in patients with bilioenteric anastomoses. Abdom Radiol 42(5):1579–1582 ((NY))
Atwell TD, et al. (2010) Percutaneous renal cryoablation: local control at mean 26 months of followup. J Urol 184(4):1291–1295
Welch BT, et al. (2014) A single-institution experience in image-guided thermal ablation of adrenal gland metastases. J Vasc Interv Radiol 25(4):593–598
Welch BT, et al. (2014) Feasibility and oncologic control following percutaneous image-guided ablation of metastatic renal cell carcinoma. J Urol 192(2):357–363
National Cancer Institute (2009) Common terminology criteria for adverse events (CTCAE) version 4.0. National Institutes of Health, National Cancer Institute
Ahmed M, et al. (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. Radiology 273(1):241–260
Ioannou GN, Perkins JD, Carithers RL Jr (2008) Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology 134(5):1342–1351
Herden U, et al. (2010) Sorafenib-induced severe acute hepatitis in a stable liver transplant recipient. Transplantation 90(1):98–99
Lu DS, et al. (2005) Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology 41(5):1130–1137
Mazzaferro V, et al. (2004) Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg 240(5):900–909
Livraghi T, et al. (2008) Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology 47(1):82–89
Liang P, et al. (2009) Malignant liver tumors: treatment with percutaneous microwave ablation–complications among cohort of 1136 patients. Radiology 251(3):933–940
Liang P, et al. (2012) Percutaneous cooled-tip microwave ablation under ultrasound guidance for primary liver cancer: a multicentre analysis of 1363 treatment-naive lesions in 1007 patients in China. Gut 61(7):1100–1101
Martin RC, Scoggins CR, McMasters KM (2010) Safety and efficacy of microwave ablation of hepatic tumors: a prospective review of a 5-year experience. Ann Surg Oncol 17(1):171–178
Poulou LS, et al. (2015) Percutaneous microwave ablation vs radiofrequency ablation in the treatment of hepatocellular carcinoma. World J Hepatol 7(8):1054–1063
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were utilized.
Conflict of interest
All authors declare no conflicts of interest.
Ethical approval
This study was performed after approval by the institutional review board. Informed consent is obtained prior to each percutaneous ablation procedure.
Rights and permissions
About this article
Cite this article
Welch, B.T., Schmitz, J.J., Kurup, A.N. et al. Feasibility and outcomes of percutaneous thermal ablation of hepatocellular carcinoma in a transplanted allograft. Abdom Radiol 43, 1478–1481 (2018). https://doi.org/10.1007/s00261-017-1323-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1323-0