Abstract
Purpose
The purpose of our study was to investigate the performance of MRI findings to predict instability of osteochondral lesion of the talus (OLT) in children and the association between skeletal maturity and lesion stability.
Materials and method
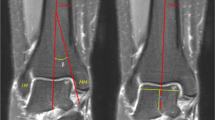
This retrospective IRB-approved and HIPPA-compliant study included children with OLT, who underwent an ankle MRI examination between March 1, 2011, and May 31, 2018. Blinded to the clinical outcome, 2 radiologists retrospectively assessed each MRI study for the presence or absence of various features on the articular side, along the interface, and on the subchondral side of each lesion. Regional skeletal maturity was recorded. Lesion stability was classified using clinical and surgical findings. Mann-Whitney U, Chi-square, Fisher’s exact, and Cochran-Armitage tests were used to compare demographic and MRI findings between children with stable and unstable lesions.
Results
Of the 48 ankles identified, 36 were stable (12.7 + 3.9 years) and 12 were unstable (14.2 + 1.6 years) lesions. None of the lesions presented as a detached fragment. Skeletal immaturity (p = 0.01) was significantly more common in stable than unstable lesions. No other MRI features were found to be significantly different between stable and unstable lesions, which included the presence of an effusion (p = 0.27), intra-articular body (p = 0.25), cartilage changes (p = 0.19), subchondral disruption (p = 0.51), T2-weighted signal intensity rim (p = 0.16), cysts (p = 0.48), marginal sclerosis (p = 0.70), and perilesional marrow edema (p = 0.17).
Conclusion
Results from our study suggest that previously published OCD criteria using conventional MRI are not sufficient for predicting stability of OLT in children. Regional skeletal maturity and older age were more predictive of unstable lesions.


Similar content being viewed by others
References
Higuera J, Laguna R, Peral M, Aranda E, Soleto J. Osteochondritis dissecans of the talus during childhood and adolescence. J Pediatr Orthop. 1998;18(3):328–32.
Letts M, Davidson D, Ahmer A. Osteochondritis dissecans of the talus in children. J Pediatr Orthop. 2003;23(5):617–25.
Kessler JI, Weiss JM, Nikizad H, Gyurdzhyan S, Jacobs JC Jr, Bebchuk JD, et al. Osteochondritis dissecans of the ankle in children and adolescents: demographics and epidemiology. Am J Sports Med. 2014;42(9):2165–71.
Naran KN, Zoga AC. Osteochondral lesions about the ankle. Radiol Clin N Am. 2008;46(6):995–1002 v.
Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959(41-a):988–1020.
Edmonds EW, Polousky J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from Konig to the ROCK study group. Clin Orthop Relat Res. 2013;471(4):1118–26.
Saxena A, Eakin C. Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med. 2007;35(10):1680–7.
Pritsch M, Horoshovski H, Farine I. Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1986;68(6):862–5.
Deginder WL. Osteochondritis dissecans of the talus. Radiology. 1955;65(4):590–8.
De Smet AA, Fisher DR, Burnstein MI, Graf BK, Lange RH. Value of MR imaging in staging osteochondral lesions of the talus (osteochondritis dissecans): results in 14 patients. AJR Am J Roentgenol. 1990;154(3):555–8.
Perumal V, Wall E, Babekir N. Juvenile osteochondritis dissecans of the talus. J Pediatr Orthop. 2007;27(7):821–5.
Vannini F, Cavallo M, Baldassarri M, Castagnini F, Olivieri A, Ferranti E, et al. Treatment of juvenile osteochondritis dissecans of the talus: current concepts review. Joints. 2014;2(4):188–91.
Dipaola JD, Nelson DW, Colville MR. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991;7(1):101–4.
Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 1999;20(12):789–93.
Mintz DN, Tashjian GS, Connell DA, Deland JT, O'Malley M, Potter HG. Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation. Arthroscopy. 2003;19(4):353–9.
Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993;21(1):13–9.
Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle Int. 2000;21(2):119–26.
Lam KY, Siow HM. Conservative treatment for juvenile osteochondritis dissecans of the talus. J Orthop Surg (Hong Kong). 2012;20(2):176–80.
Heyse TJ, Schuttler KF, Schweitzer A, Timmesfeld N, Efe T, Paletta JR, et al. Juvenile osteochondritis dissecans of the talus: predictors of conservative treatment failure. Arch Orthop Trauma Surg. 2015;135(10):1337–41.
Hembree WC, Wittstein JR, Vinson EN, Queen RM, Larose CR, Singh K, et al. Magnetic resonance imaging features of osteochondral lesions of the talus. Foot Ankle Int. 2012;33(7):591–7.
Nguyen JC, Allen H, Liu F, Woo KM, Zhou Z, Kijowski R. Maturation-related changes in T2 relaxation times of cartilage and meniscus of the pediatric knee joint at 3 T. AJR Am J Roentgenol. 2018;211(6):1369–75.
Nguyen JC, Lin B, Potter HG. Maturation-dependent findings in the shoulders of pediatric baseball players on magnetic resonance imaging. Skelet Radiol. 2019;48(7):1087–94.
Elias I, Jung JW, Raikin SM, Schweitzer MW, Carrino JA, Morrison WB. Osteochondral lesions of the talus: change in MRI findings over time in talar lesions without operative intervention and implications for staging systems. Foot Ankle Int. 2006;27(3):157–66.
Higashiyama I, Kumai T, Takakura Y, Tamail S. Follow-up study of MRI for osteochondral lesion of the talus. Foot Ankle Int. 2000;21(2):127–33.
Nguyen JC, Degnan AJ, Barrera CA, Hee TP, Ganley TJ, Kijowski R. Osteochondritis Dissecans of the elbow in children: MRI findings of instability. AJR Am J Roentgenol. 2019;213(5):1145–51.
Kijowski R, Blankenbaker DG, Shinki K, Fine JP, Graf BK, De Smet AA. Juvenile versus adult osteochondritis dissecans of the knee: appropriate MR imaging criteria for instability. Radiology. 2008;248(2):571–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Kramer J, Stiglbauer R, Engel A, Prayer L, Imhof H. MR contrast arthrography (MRA) in osteochondrosis dissecans. J Comput Assist Tomogr. 1992;16(2):254–60.
Ellermann J, Johnson CP, Wang L, Macalena JA, Nelson BJ, LaPrade RF. Insights into the epiphyseal cartilage origin and subsequent osseous manifestation of juvenile osteochondritis dissecans with a modified clinical MR imaging protocol: a pilot study. Radiology. 2017;282(3):798–806.
Uozumi H, Sugita T, Aizawa T, Takahashi A, Ohnuma M, Itoi E. Histologic findings and possible causes of osteochondritis dissecans of the knee. Am J Sports Med. 2009;37(10):2003–8.
Eismann EA, Pettit RJ, Wall EJ, Myer GD. Management strategies for osteochondritis dissecans of the knee in the skeletally immature athlete. J Orthop Sports Phys Ther. 2014;44(9):665–79.
Samora WP, Chevillet J, Adler B, Young GS, Klingele KE. Juvenile osteochondritis dissecans of the knee: predictors of lesion stability. J Pediatr Orthop. 2012;32(1):1–4.
Blumer MJ, Longato S, Fritsch H. Structure, formation and role of cartilage canals in the developing bone. Ann Anat. 2008;190(4):305–15.
O'Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38(2):392–404.
Millington SA, Grabner M, Wozelka R, Anderson DD, Hurwitz SR, Crandall JR. Quantification of ankle articular cartilage topography and thickness using a high resolution stereophotography system. Osteoarthr Cartil. 2007;15(2):205–11.
Athanasiou KA, Niederauer GG, Schenck RC Jr. Biomechanical topography of human ankle cartilage. Ann Biomed Eng. 1995;23(5):697–704.
Bruns J, Rosenbach B. Osteochondrosis dissecans of the talus. Comparison of results of surgical treatment in adolescents and adults. Arch Orthop Trauma Surg. 1992;112(1):23–7.
Kim HK, Laor T, Graham TB, Anton CG, Salisbury SR, Racadio JM, et al. T2 relaxation time changes in distal femoral articular cartilage in children with juvenile idiopathic arthritis: a 3-year longitudinal study. AJR Am J Roentgenol. 2010;195(4):1021–5.
Kang CH, Kim HK, Shiraj S, Anton C, Kim DH, Horn PS. Patellofemoral instability in children: T2 relaxation times of the patellar cartilage in patients with and without patellofemoral instability and correlation with morphological grading of cartilage damage. Pediatr Radiol. 2016;46(8):1134–41.
Nguyen JC, Liu F, Blankenbaker DG, Woo KM, Kijowski R. Juvenile osteochondritis dissecans: cartilage T2 mapping of stable medial femoral condyle lesions. Radiology. 2018;288(2):536–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not required for this retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, M., Francavilla, M.L., Lawrence, J.T.R. et al. Osteochondral lesion of the talus in children: Are there MRI findings of instability?. Skeletal Radiol 49, 1305–1311 (2020). https://doi.org/10.1007/s00256-020-03436-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03436-6