Abstract
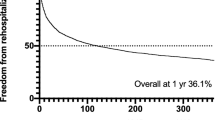
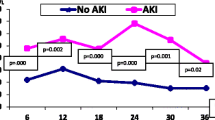
The utility of troponin levels, including high sensitivity troponin T (hs-TnT), after orthotopic heart transplant (OHT) is controversial. Conflicting data exist regarding its use as a marker of acute rejection. Few studies have examined possible associations of hs-TnT levels immediately after OHT with metrics of intensive care unit (ICU) resource utilization or risk of acute rejection. We performed a retrospective cohort chart review including all OHT recipients < 20 years of age at our center between June 2019 and December 2022. Patients were divided into two groups based on supra- or sub-median initial hs-TnT levels (median 3462.5 ng/L). Primary outcome was days requiring ICU-level care, secondary outcomes included days intubated, days requiring positive pressure ventilation (PPV), days on inotropic medications, actual ICU length of stay, Vasoactive Inotrope Scores (VIS) on postoperative days (POD) 0 through 7, and acute rejection at 30 days and one year after OHT. Patients with higher hs-TnT required ICU level care for longer [13.5 (10–17.5) vs. 9.5 (8–12) days, p = 0.01] and spent more days intubated [6 (4–7) vs. 3 (3–5) days, p < 0.001], on PPV [9 (6–15) vs. 6 (5–8.5) days, p = 0.02], and on inotropes [11 (9–14) vs. 8 (7–11) days, p = 0.025]. VIS was only different between groups on POD7 [5 (3–7) vs. 3 (0–5), p = 0.04]. There was no difference in rejection between the groups. Higher hs-TnT immediately following pediatric OHT may predict higher ICU resource utilization, despite no difference in VIS, although it does not predict acute rejection in the first year after OHT.


Similar content being viewed by others
References
Rossano JW, Cherikh WS, Chambers DC et al (2018) The international thoracic organ transplant registry of the international society for heart and lung transplantation: twenty-first pediatric heart trans-plantation report—2018; focus theme: multiorgan transplantation. J Heart Lung Transplant 37(10):1184–1195
McCulloch MA, Zuckerman WA, Möller T et al (2020) Effects of donor cause of death, ischemia time, inotrope exposure, troponin values, cardiopulmonary resuscitation, electrocardiographic and echocardiographic data on recipient outcomes: a review of the literature. Pediatr Transplant 24(3):e13676. https://doi.org/10.1111/petr.13676
Tallaj JA, Pamboukian SV, George JF et al (2014) Have risk factors for mortality after heart transplantation changed over time? Insights from 19 years of cardiac transplant research database study. J Heart Lung Transplant 33(12):1304–1311. https://doi.org/10.1016/j.healun.2014.08.014
Hong KN, Iribarne A, Worku B et al (2011) Who is the high-risk recipient? Predicting mortality after heart transplant using pretransplant donor and recipient risk factors. Ann Thorac Surg 92(2):520–527. https://doi.org/10.1016/j.athoracsur.2011.02.086
Kanaan UB, Chiang VW (2004) Cardiac troponins in pediatrics. Pediatr Emerg Care 20(5):323–329. https://doi.org/10.1097/01.pec.0000125664.35690.51
Jaffe AS, Ravkilde J, Roberts R et al (2000) It’s time for a change to a troponin standard. Circulation 102:1216
Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction [published correction appears in J Am Coll Cardiol 2001 Mar 1;37(3):973]. J Am Coll Cardiol 36(3):959–969. https://doi.org/10.1016/s0735-1097(00)00804-4
Garg P, Morris P, Fazlanie AL et al (2017) Cardiac biomarkers of acute coronary syndrome: from history to high-sensitivity cardiac troponin. Intern Emerg Med 12(2):147–155. https://doi.org/10.1007/s11739-017-1612-1
Clerico A, Aimo A, Cantinotti M (2021) High-sensitivity cardiac troponins in pediatric population. Clin Chem Lab Med. 60(1):18–32. https://doi.org/10.1515/cclm-2021-0976
Wang AP, Homme JL, Qureshi MY, Sandoval Y, Jaffe AS (2022) High-sensitivity troponin T testing for pediatric patients in the emergency department. Pediatr Cardiol 43(2):350–359. https://doi.org/10.1007/s00246-021-02726-7
Boroński B, Piotrowski A, Pągowska-Klimek I (2022) Value of troponin T measurements for prediction of postoperative course and length of ICU stay of children after surgical correction of congenital heart disease. Anaesthesiol Intensive Ther 54(2):114–119. https://doi.org/10.5114/ait.2022.114488
Mori Y, Nakashima Y, Kaneko S, Inoue N, Murakami T (2020) Risk factors for cardiac adverse events in infants and children with complex heart disease scheduled for bi-ventricular repair: prognostic value of pre-operative B-type natriuretic peptide and high-sensitivity Troponin T. Pediatr Cardiol 41(8):1756–1765. https://doi.org/10.1007/s00246-020-02437-5
Immer FF, Stocker F, Seiler AM et al (1999) Troponin-I for prediction of early postoperative course after pediatric cardiac surgery. J Am Coll Cardiol 33(6):1719–1723. https://doi.org/10.1016/s0735-1097(99)00061-3
Kojima T, Toda K, Oyanagi T, Yoshiba S, Kobayashi T, Sumitomo N (2020) Early assessment of cardiac Troponin I predicts the postoperative cardiac status and clinical course after congenital heart disease surgery. Heart Vessels 35(3):417–421. https://doi.org/10.1007/s00380-019-01497-9
Mildh LH, Pettilä V, Sairanen HI, Rautiainen PH (2006) Cardiac Troponin T levels for risk stratification in pediatric open heart surgery. Ann Thorac Surg 82(5):1643–1648. https://doi.org/10.1016/j.athoracsur.2006.05.014
Momeni M, Poncelet A, Rubay J et al (2017) Does postoperative cardiac troponin-I have any prognostic value in predicting midterm mortality after congenital cardiac surgery? J Cardiothorac Vasc Anesth 31(1):122–127. https://doi.org/10.1053/j.jvca.2016.02.018
Bottio T, Vida V, Padalino M, Gerosa G, Stellin G (2006) Early and long-term prognostic value of Troponin-I after cardiac surgery in newborns and children. Eur J Cardiothorac Surg 30(2):250–255. https://doi.org/10.1016/j.ejcts.2006.05.001
Coric D, Smith NA (2017) Postoperative troponin measurement as a screening tool for adverse cardiac events in adult patients undergoing moderate or major non-cardiac surgery. Anaesth Intensive Care 45(6):683–687. https://doi.org/10.1177/0310057X1704500606
Writing Committee for the VISION Study Investigators, Devereaux PJ, Biccard BM et al (2017) Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 317(16):1642–1651. https://doi.org/10.1001/jama.2017.4360
Giannitsis E, Kurz K, Hallermayer K et al (2009) Analytical validation of a high-sensitivity cardiac Troponin T assay. Clin Chem 56:254
Sherwood MW, Kristin NL (2014) High-sensitivity troponin assays: evidence, indications, and reasonable use. J Am Heart Assoc. 3(1):e000403. https://doi.org/10.1161/JAHA.113.000403
Zimmermann R, Baki S, Dengler TJ et al (1993) Troponin T release after heart transplantation. Br Heart J 69(5):395–398. https://doi.org/10.1136/hrt.69.5.395
Ambrosi P, Kreitmann B, Fromonot J, Habib G, Guieu R (2015) Plasma ultrasensitive cardiac troponin during long-term follow-up of heart transplant recipients. J Card Fail 21(2):103–107. https://doi.org/10.1016/j.cardfail.2014.10.015. (Epub 2014 Nov 3 PMID: 25451703)
Erbel C, Taskin R, Doesch A et al (2013) High-sensitive Troponin T measurements early after heart transplantation predict short- and long-term survival. Transpl Int 26(3):267–272. https://doi.org/10.1111/tri.12024
Fitzsimons SJ, Evans JDW, Rassl DM et al (2021) High-sensitivity cardiac troponin is not associated with acute cellular rejection after heart transplantation [published online ahead of print, 2021 Jun 29]. Transplantation. https://doi.org/10.1097/TP.0000000000003876
Fitzsimons S, Evans J, Parameshwar J, Pettit SJ (2018) Utility of troponin assays for exclusion of acute cellular rejection after heart transplantation: a systematic review. J Heart Lung Transplant 37(5):631–638. https://doi.org/10.1016/j.healun.2017.12.008
McCartney SL, Patel C, Del Rio JM (2017) Long-term outcomes and management of the heart transplant recipient. Best Pract Res Clin Anaesthesiol 31(2):237–248. https://doi.org/10.1016/j.bpa.2017.06.003
Wilhelm MJ (2015) Long-term outcome following heart transplantation: current perspective. J Thorac Dis 7(3):549–551. https://doi.org/10.3978/j.issn.2072-1439.2015.01.46
Colvin MM, Cook JL, Chang P et al (2015) Antibody-mediated rejection in cardiac transplantation: emerging knowledge in diagnosis and management: a scientific statement from the American Heart Association. Circulation 131(18):1608–1639. https://doi.org/10.1161/CIR.0000000000000093
Hollander SA, Peng DM, Mills M et al (2018) Pathological antibody-mediated rejection in pediatric heart transplant recipients: Immunologic risk factors, hemodynamic significance, and outcomes. Pediatr Transplant 22(5):e13197. https://doi.org/10.1111/petr.13197
Webber SA, Naftel DC, Parker J et al (2003) Late rejection episodes more than 1 year after pediatric heart transplantation: risk factors and outcomes. J Heart Lung Transplant 22(8):869–875. https://doi.org/10.1016/s1053-2498(02)00819-7
Chin C, Naftel DC, Singh TP et al (2004) Risk factors for recurrent rejection in pediatric heart transplantation: a multicenter experience. J Heart Lung Transplant 23(2):178–185. https://doi.org/10.1016/S1053-2498(03)00059-7
Austin BA, Taylor DO (2010) Surrogate markers of rejection. Curr Opin Organ Transplant 15(5):645–649. https://doi.org/10.1097/MOT.0b013e32833d7e31
Chance JJ, Segal JB, Wallerson G, Kasper E, Hruban RH, Kickler TS, Chan DW (2001) Cardiac Troponin T and C-reactive protein as markers of acute cardiac allograft rejection. Clin Chim Acta 312(1–2):31–39
Wåhlander H, Kjellström C, Holmgren D (2002) Sustained elevated concentrations of cardiac Troponin T during acute allograft rejection after heart transplantation in children. Transplantation 74(8):1130–1135
Amarelli C, De Santo LS, Marra C et al (2012) Early graft failure after heart transplant: risk factors and implications for improved donor-recipient matching. Interact Cardiovasc Thorac Surg 15(1):57–62. https://doi.org/10.1093/icvts/ivs113
Mullen JC, Bentley MJ, Scherr KD, Chorney SG, Burton NI, Tymchak WJ, Koshal A, Modry DL (2002) Troponin T and I are not reliable markers of cardiac transplant rejection. Eur J Cardiothorac Surg 22(2):233–237. https://doi.org/10.1016/s1010-7940(02)00293-2. (PMID: 12142191)
Wang CW, Steinhubl SR, Castellani WJ et al (1996) Inability of serum myocyte death markers to predict acute cardiac allograft rejection. Transplantation 62(12):1938–1941. https://doi.org/10.1097/00007890-199612270-00046
Walpoth BH, Celik B, Printzen G, Peheim E, Colombo JP, Schaffner T, Althaus U, Carrel T, Reichenspurner H, Reitz B (1998) Assessment of troponin-T for detection of clinical cardiac rejection. Transpl Int 11(Suppl 1):S502–S507. https://doi.org/10.1007/s001470050528. (PMID: 9665046)
Patel PC, Hill DA, Ayers CR, Lavingia B, Kaiser P, Dyer AK, Barnes AP, Thibodeau JT, Mishkin JD, Mammen PP, Markham DW, Stastny P, Ring WS, de Lemos JA, Drazner MH (2014) High-sensitivity cardiac troponin I assay to screen for acute rejection in patients with heart transplant. Circ Heart Fail 7(3):463–469. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000697. (Epub 2014 Apr 14 PMID: 24733367)
Wierzbicki K, Bochenek M, Kędziora A et al (2014) Does the postoperative Troponin I blood concentration measured in the perioperative period influence hemodynamic function of a transplanted heart? Kardiochir Torakochirurgia Pol 11(3):289–293. https://doi.org/10.5114/kitp.2014.45679
Su JA, Kumar SR, Mahmoud H et al (2019) Postoperative serum troponin trends in infants undergoing cardiac surgery. Semin Thorac Cardiovasc Surg 31(2):244–251. https://doi.org/10.1053/j.semtcvs.2018.08.010
Hirsch R, Dent CL, Wood MK et al (1998) Patterns and potential value of cardiac troponin I elevations after pediatric cardiac operations. Ann Thorac Surg 65(5):1394–1399. https://doi.org/10.1016/s0003-4975(98)00228-8
Saraiya NR, Sun LS, Jonassen AE, Pesce MA, Queagebeur JM (2005) Serum cardiac Troponin-I elevation in neonatal cardiac surgery is lesion-dependent. J Cardiothorac Vasc Anesth 19(5):620–625. https://doi.org/10.1053/j.jvca.2005.07.004
Tárnok A, Bocsi J, Osmancik P, Häusler HJ, Schneider P, Dähnert I (2005) Cardiac Troponin I release after transcatheter atrial septal defect closure depends on occluder size but not on patient’s age. Heart 91(2):219–222. https://doi.org/10.1136/hrt.2003.029884
Acknowledgements
We thank perfusionist Michael Brewer for his help obtaining data informing cardiopulmonary bypass and aortic cross-clamp times, Dr. Tania Gennell for her help obtaining exact times for ECMO cannulation and flow for relevant patients, and Dr. Arthur Smerling for his insight.
Funding
Funding for this project was received through grants from Colin’s Kids Foundation and Matthew’s Hearts of Hope, Inc.
Author information
Authors and Affiliations
Contributions
A.B. Performed data analysis, wrote the main manuscript text, and prepared all figures and tables. S.D. Performed patient chart review and data entry. M.D., I.L., B.M., and T.C. assisted with research methodology. I.L. and B.M. provided insight as transplant specialists. Y.Z. assisted with data analysis, statistics consultation, and table preparation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Butensky, A.M., Desai, S., Dilorenzo, M. et al. Association Between High Sensitivity Troponin Levels Following Pediatric Orthotopic Heart Transplantation and Intensive Care Unit Resource Utilization. Pediatr Cardiol 45, 829–839 (2024). https://doi.org/10.1007/s00246-024-03424-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-024-03424-w