Abstract
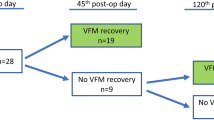
Vocal fold (VF) immobility is a common complication after pediatric cardiothoracic surgeries involving the aortic arch and conotruncal region. Nasolaryngoscopy is considered the standard for diagnosis but is invasive and requires expertise and special resources. VF ultrasound (VF US) is an efficient, non-invasive alternative for VF evaluation in the post-cardiac surgical setting. Our aim was to improve screening rates for vocal fold motion impairment (VFMI) by implementing VF US in a group of pre-identified high-risk patients after index cardiac surgeries using Quality Improvement (QI) methodology. The QI project included formation of a widely representative stakeholder team, collaborative development of a screening protocol for the cohort of patients in our tertiary center. Baseline data were derived by retrospective review of screening and incidence of VFMI in a similar post-surgical cohort in 2 years prior to this intervention. We implemented an US screening algorithm with multidisciplinary care coordination. We evaluated feeding practices and length of stay (LOS) related to our screening interventions and documented follow up practices. Screening for VFMI by ultrasound increased from 59 to 92% after implementation of the VF screening protocol. Additionally, time between extubation and VF US decreased from 7.7 to 2.3 days. The positive predictive value of VF US was 96%. Patients with VFMI had a longer LOS and greater dependence on tube feeds at discharge after index surgery. We successfully implemented an ultrasound-based screening protocol for VFMI and demonstrated improved screening, timeliness and high positive predictive value of ultrasound.





Similar content being viewed by others
References
Lambert A, Winlaw DS, Deacon V et al (2020) Routine vocal cord mobility assessment post cardiac surgery via median sternotomy approach. Int J Pediatr Otorhinolaryngol. https://doi.org/10.1016/j.ijporl.2020.110331
Garcia-Torres E, Anton-Pacheco JL, Carmen Luna-Paredes M et al (2020) Vocal cord paralysis after cardiovascular surgery in children: incidence, risk factors and diagnostic options. Eur J Cardiothorac Surg 57(2):359–365. https://doi.org/10.1093/ejcts/ezz190
Gorantla SC, Chan T, Shen I, Wilkes J, Bratton SL (2019) Current epidemiology of vocal cord dysfunction after congenital heart surgery in young infants. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 20(9):817–825. https://doi.org/10.1097/PCC.0000000000002010
Averin K, Uzark K, Beekman RH, Willging JP, Pratt J, Manning PB (2012) Postoperative assessment of laryngopharyngeal dysfunction in neonates after Norwood operation. Ann Thorac Surg 94(4):1257–1261. https://doi.org/10.1016/j.athoracsur.2012.01.009
Lee MGY, Millar J, Rose E et al (2018) Laryngeal ultrasound detects a high incidence of vocal cord paresis after aortic arch repair in neonates and young children. J Thorac Cardiovasc Surg 155(6):2579–2587. https://doi.org/10.1016/j.jtcvs.2017.12.133
Narawane (2022) Vocal fold movement and silent aspiration after congenital heart surgery. The Laryngoscope - Wiley Online Library. Accessed 25 July 2022. https://onlinelibrary.wiley.com/doi/full/https://doi.org/10.1002/lary.29817
Sanchez-Jacob R, Cielma TK, Mudd PA (2021) Ultrasound of the vocal cords in infants. Pediatr Radiol. https://doi.org/10.1007/s00247-021-05235-0
Ongkasuwan J, Ocampo E, Tran B (2017) Laryngeal ultrasound and vocal fold movement in the pediatric cardiovascular intensive care unit. Laryngoscope 127(1):167–172. https://doi.org/10.1002/lary.26051
Hamilton CE, Su E, Tawfik D et al (2021) Assessment of vocal cord motion using laryngeal ultrasound in children: a systematic review and meta-analysis. Pediatr Crit Care Med 22(10):e532. https://doi.org/10.1097/PCC.0000000000002734
Sayyid Z, Vendra V, Meister KD, Krawczeski CD, Speiser NJ, Sidell DR (2019) Application-based translaryngeal ultrasound for the assessment of vocal fold mobility in children. Otolaryngol Head Neck Surg 161(6):1031–1035
Raulston JEB, Smood B, Moellinger A et al (2019) Aspiration after congenital heart surgery. Pediatr Cardiol 40(6):1296–1303. https://doi.org/10.1007/s00246-019-02153-9
Ryan MA, Upchurch PA, Senekki-Florent P (2020) Neonatal vocal fold paralysis. NeoReviews 21(5):e308–e322. https://doi.org/10.1542/neo.21-5-e308
Barr JM, Bowman K, Deshpande M et al (2021) Incidence and recovery of vocal fold immobility following pediatric cardiac operations. World J Pediatr Congenit Heart Surg 12(4):535–541. https://doi.org/10.1177/21501351211015922
Author information
Authors and Affiliations
Contributions
CH and CY: collected the data and organized it. CH and JC: wrote the main manuscript. JF: collected the feeding data. SP and KJ: developed the screening protocol and assessment of vocal fold injury. AB and KR: developed the process and outcome measures, guided and created the tables and figures. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Horner, C., Chan, T., Yip, C. et al. Improving Timeliness of Vocal Fold Mechanical Injury Screening Following Norwood or Arch Reconstruction: A Quality Improvement Initiative at a Single Center. Pediatr Cardiol 44, 388–395 (2023). https://doi.org/10.1007/s00246-022-03064-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-03064-y