Abstract
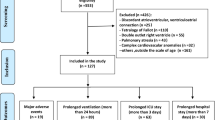
In complete atrioventricular canal defect (CAVC), there are limited data on preoperative clinical and echocardiographic predictors of operative timing and postoperative outcomes. A retrospective, single-center analysis of all patients who underwent primary biventricular repair of CAVC between 2006 and 2015 was performed. Associated cardiac anomalies (tetralogy of Fallot, double outlet right ventricle) and arch operation were excluded. Echocardiographic findings on first postnatal echocardiogram were correlated with surgical timing and postoperative outcomes using bivariate descriptive statistics and multivariable logistic regression. 153 subjects (40% male, 84% Down syndrome) underwent primary CAVC repair at a median age of 3.3 (IQR 2.5–4.2) months. Median postoperative length of stay (LOS) was 7 (IQR 5–15) days. Eight patients (5%) died postoperatively and 24 (16%) required reoperation within 1 year. On multivariable analysis, small aortic isthmus (z score < − 2) was associated with early primary repair at < 3 months (OR 2.75, 95% CI 1.283–5.91) and need for early reoperation (OR 3.79, 95% CI 1.27–11.34). Preoperative ventricular dysfunction was associated with higher postoperative mortality (OR 7.71, 95% CI 1.76–33.69). Other factors associated with mortality and longer postoperative LOS were prematurity (OR 5.30, 95% CI 1.24–22.47 and OR 5.50, 95% CI 2.07–14.59, respectively) and lower weight at surgery (OR 0.17, 95% CI 0.04–0.75 and OR 0.55, 95% CI 0.35–0.85, respectively). Notably, preoperative atrioventricular valve regurgitation and Down syndrome were not associated with surgical timing, postoperative outcomes or reoperation, and there were no echocardiographic characteristics associated with late reoperation beyond 1 year after repair. Key preoperative echocardiographic parameters helped predict operative timing and postoperative outcomes in infants undergoing primary CAVC repair. Aortic isthmus z score < − 2 was associated with early surgical repair and need for reoperation, while preoperative ventricular dysfunction was associated with increased mortality. These echocardiographic findings may help risk-stratified patients undergoing CAVC repair and improve preoperative counseling and surgical planning.
Similar content being viewed by others
References
Suzuki T et al (2008) Results of definitive repair of complete atrioventricular septal defect in neonates and infants. Ann Thorac Surg 86(2):596–602
Atz AM et al (2011) Surgical management of complete atrioventricular septal defect: associations with surgical technique, age, and trisomy 21. J Thorac Cardiovasc Surg 141(6):1371–1379
Xie O et al (2014) Outcomes of repair of complete atrioventricular septal defect in the current era. Eur J Cardiothorac Surg 45(4):610–617
St Louis JD et al (2014) Contemporary outcomes of complete atrioventricular septal defect repair: analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. J Thorac Cardiovasc Surg 148(6):2526–2531
Hraska V, Walters HL 3rd (2010) Management of complete atrioventricular canal defect with aortic arch obstruction: an unresolved debate. World J Pediatr Congenit Heart Surg 1(2):199–205
Redmond JM et al (1996) Complete atrioventricular septal defects: the influence of associated cardiac anomalies on surgical management and outcome. Eur J Cardiothorac Surg 10(11):991–995
Gow RM et al (1984) Coarctation of the aorta or subaortic stenosis with atrioventricular septal defect. Am J Cardiol 53(10):1421–1428
Cohen MS et al (1996) Morphometric analysis of unbalanced common atrioventricular canal using two-dimensional echocardiography. J Am Coll Cardiol 28(4):1017–1023
Szwast AL et al (2011) Usefulness of left ventricular inflow index to predict successful biventricular repair in right-dominant unbalanced atrioventricular canal. Am J Cardiol 107(1):103–109
Reddy VM et al (1998) Atrioventricular valve function after single patch repair of complete atrioventricular septal defect in infancy: how early should repair be attempted? J Thorac Cardiovasc Surg 115(5):1032–1040
Stellin G et al (2003) Surgical treatment of complete A-V canal defects in children before 3 months of age. Eur J Cardiothorac Surg 23(2):187–193
Stulak JM et al (2009) Reoperations after initial repair of complete atrioventricular septal defect. Ann Thorac Surg 87(6):1872–1877; discussion 1877-8.
Ginde S et al (2015) Long-term outcomes after surgical repair of complete atrioventricular septal defect. J Thorac Cardiovasc Surg 150(2):369–374
Myers PO et al (2012) Improving left ventricular outflow tract obstruction repair in common atrioventricular canal defects. Ann Thorac Surg 94(2):599–605; discussion 605
Michielon G et al (1995) Left atrioventricular valve incompetence after repair of common atrioventricular canal defects. Ann Thorac Surg 60(6 Suppl):S604–S609
Prifti E et al (2004) Repair of complete atrioventricular septal defects in patients weighing less than 5 kg. Ann Thorac Surg 77(5):1717–1726
Kaza AK et al (2011) Surgical interventions for atrioventricular septal defect subtypes: the pediatric heart network experience. Ann Thorac Surg 92(4):1468–1475; discussion 1475
Malhotra SP et al (2008) Reoperation for left atrioventricular valve regurgitation after atrioventricular septal defect repair. Ann Thorac Surg 86(1):147–151; discussion 151–2.
Acknowledgement
This work was supported in part by the Cardiac Center Clinical Research Core at the Children’s Hospital of Philadelphia.
Funding
This work did not receive funding support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have reported that they have no relationships relevant to the contents of this paper to disclose. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Burstein, D.S., Gray, P.E., Griffis, H.M. et al. Preoperative Clinical and Echocardiographic Factors Associated with Surgical Timing and Outcomes in Primary Repair of Common Atrioventricular Canal Defect. Pediatr Cardiol 40, 1057–1063 (2019). https://doi.org/10.1007/s00246-019-02116-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02116-0