Abstract
Background
Pressure ulcers are frequent complications for spinal-cord-injured patients and, trochanteric pressure sores, are quite difficult to treat. This site requires to consider some aspects, such as wound dimension, surgical timing, and reconstructive flap choice.
Methods
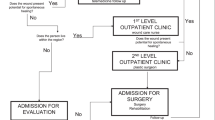
We report our experience from 2011 to 2016 on 82 trochanteric sores in 68 spinal-cord-injured patients. All the cases were treated with two-time procedures. Firstly, we performed the surgical toilette of the wound, and in the second procedure, the reconstruction with a muscle or musculocutaneous flap.
Results
Using the two-time procedure, we report no recurrences after a mean follow-up of 3 years. The main complication reported was a seroma that undergo to a spontaneous resolution. Conclusions
Conclusions
We believe that the described approach can be useful to treat trochanteric sores and to reduce the recurrence rate. Muscle flaps seem to be superior to fasciocutaneous or perforator flaps in this site.
Level of evidence: Level III, therapeutic study.




Similar content being viewed by others
References
Gélis A, Dupeyron A, Legros P et al (2009) Pressure ulcer risk factors in persons with spinal cord injury Part 2: the chronic stage. Spinal Cord 47:651–661. https://doi.org/10.1038/sc.2009.32
Cowan LJ, Ahn H, Flores M et al (2019) Pressure ulcer prevalence by level of paralysis in patients with spinal cord injury in long-term care. Adv Ski Wound Care 32:122–130
Shi X, Zhou Z, Shen B et al (2019) The use of extended trochanteric osteotomy in 2-stage reconstruction of the hip for infection. J Arthroplasty 34(7):1470–1475. https://doi.org/10.1016/j.arth.2019.02.054
Bhagwat BM, Pearl RM, Laub DR (1978) Uses of the rectus femoris myocutaneous flap. Plast Reconstr Surg 62:698
Dowden RV, McCraw JB (1980) The vastus lateralis muscle flap: technique and applications. Ann Plast Surg 4(5):396–404
Negosanti L, Tedeschi S, Trapani FF et al (2020) Multiple flaps for trochanteric pressure sore reconstruction: a case series. Cureus 12(7):e9369. https://doi.org/10.7759/cureus.9369
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Sameem M, Au M, Wood T et al (2012) A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg 130:67e–77e
Schryvers OI, Stranc MF, Nance PW (2000) Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil 81:1556–1562
Foster RD, Anthony JP, Mathes SJ et al (1997) Flap selection as a determinant of success in pressure sore coverage. Arch Surg 132:868–873
Song YP, Wang L, Yuan BF et al (2021) Negative-pressure wound therapy for III/IV pressure injuries: a meta-analysis. Wound Repair Regen 29(1):20–33. https://doi.org/10.1111/wrr.12863
Jósvay J, Sashegyi M, Kelemen P, Donáth A (2006) Modified tensor fascia lata musculofasciocutaneous flap for the coverage of trochanteric pressure sores. J Plast Reconstr Aesthet Surg 59(2):137–141. https://doi.org/10.1016/j.bjps.2005.07.009
Kumar P, Bhaskara KG, Bharadwaj S (2003) Management of pressure ulcers. Plast Reconstr Surg 111(7):2480–2481. https://doi.org/10.1097/01.PRS.0000063129.41508.C9
Huang KC, Peng KT, Li YY et al (2005) Modified vastus lateralis flap in treating a difficult hip infection. J Trauma 59(3):665–671
Ishida LH, Munhoz AM, Montag E et al (2005) Tensor fasciae latae perforator flap: minimizing donor-site morbidity in the treatment of trochanteric pressure sores. Plast Reconstr Surg 116(5):1346–1352. https://doi.org/10.1097/01.prs.0000182222.66591.06
Greco M, Marchetti F, Tempesta M et al (2013) Cutaneous flaps in the treatment of 338 pressure sores: a better choice. Ann Ital Chir 84(6):655–9
Wang CH, Chen SY, Fu JP, Dai NT et al (2011) Reconstruction of trochanteric pressure sores with pedicled anterolateral thigh myocutaneous flaps. J Plast Reconstr Aesthet Surg 64(5):671–6. https://doi.org/10.1016/j.bjps.2010.08.042
Hallock GG (2005) The proximal pedicled anterolateral thigh flap for lower limb coverage. Ann Plast Surg 55(5):466–469. https://doi.org/10.1097/01.sap.0000184462.04343.e6
Kim YH, Kim SW, Kim JT, Kim CY (2013) Tensor fascia lata flap versus tensor fascia lata perforator-based island flap for the coverage of extensive trochanteric pressure sores. Ann Plast Surg 70(6):684–690. https://doi.org/10.1097/SAP.0b013e31823dcec2
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institutional Ethical Committee AVEC with the reference number 1000–2020-OSS-AUSLIM on 19th November 2020. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
The authors affirm that human research participants provided informed consent for sharing their data and publication of their images.
Conflict of interest
Luca Negosanti, Siriana Landi, Luca Gaiani, Rita Capirossi, Micaela Battilana, and Rossella Sgarzani declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Negosanti, L., Landi, S., Gaiani, L. et al. Reconstructive procedure for treatment of trochanteric pressure ulcers in spinal-cord-injured patients. Eur J Plast Surg 46, 1213–1217 (2023). https://doi.org/10.1007/s00238-023-02086-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02086-w