Abstract
Background
It has been demonstrated that medical students are capable of learning microsurgical techniques. We hypothesize that microsurgical training might give insight into the importance of delicate tissue handling and correct knot tying that could have a positive influence on macrosurgical skills. The primary aim of this study was to evaluate the effect of microsurgical training on macrosurgical suturing skills in novice medical students.
Subjects and methods
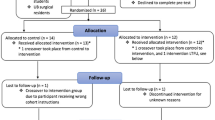
In 2018, 46 novice medical students were enrolled and randomized into two groups. The intervention group received both macro- and microsurgical training and the control group received only microsurgical training. Both groups underwent an assessment test that consisted of macrosurgical tasks of three simple interrupted sutures with a square knot and continuous three-stitch long over-and-over sutures. These tests were individually filmed and assessed using the University of Bergen suturing skills assessment tool (UBAT) and the Objective Structured Assessment of Technical Skill global rating scale (OSATS). Questionnaires regarding future career ambitions and attitudes towards plastic surgery were also completed both prior to and following the tests.
Results
The intervention group needed a longer time to complete the tasks than the control group (12.2 min vs. 9.6 min, p > 0.001), and scored lower on both the UBAT (5.6 vs. 9.0, p > 0.001) and the OSATS (11.1 vs. 13.1, p > 0.001) assessments. The microsurgery course tended to positively influence the students’ attitudes towards a career in plastic surgery (p = 0.002). This study demonstrates poorer macrosurgical skills in the medical students group exposed to microsurgical training. The true effect of microsurgical training warrants further investigation.
Level of evidence: Level I, diagnostic study.
Similar content being viewed by others
Introduction
In modern medical training, a greater focus is placed on patient safety and the mastering of prepractice/preregistration core procedures by medical students, such as basic suturing skills. Such skills are also included in the Scandinavian core undergraduate curriculum in plastic surgery [1]. One way to learn suturing skills is to use simulation [2]. In brief, simulation refers to the teaching and training of skills in a context that resembles an authentic clinical situation as closely as possible [2, 3], without jeopardizing the safety of patients. Despite this development, relatively little attention has been given to the teaching, training, and evaluation of basic surgical skills, such as suturing, in undergraduate medical training [4,5,6,7]. Specifically, there are few studies on the efficacy of different simulation models in an undergraduate setting [8,9,10,11,12,13,14,15].
Microsurgical technique was developed principally in the 1970s, matured into a commonly used plastic surgical technique during the 1980s and 1990s, and has now become an integrated part of many specialties [16]. Even though microsurgery is a highly specialized technique, and not used by all surgeons, it has been hypothesized that microsurgical training might be of benefit for most surgeons in training [17, 18]. Specifically, such training could lead to more delicate tissue handling and improved control of instruments and suture placing [17]. However, this has never been confirmed in randomized controlled trials. In addition, training in suturing technique and microsurgery might influence students’ attitude to surgery as a potential career choice in general [19], and plastic and reconstructive surgery in particular [20,21,22].
It has been demonstrated that medical students are capable of learning microsurgical techniques [20,21,22,23,24,25]. One study [20] gave novice medical students and surgeons with little experience in microsurgery the same theoretical and practical course and compared the end results. In fact, the students achieved a higher mean score than the surgeons in both the practical (13.71 vs. 11.73 out of 16, p < 0.0001) and theoretical exam (15.27 vs. 13.50, p = 0.009) [20]. Another study demonstrated that the training result of novice medical students and experienced surgeons is similar as regards to average time to perform a patent vascular anastomosis (52 min ± 2 (SD) vs. 53 min ± 4 (SD)) [21]. Nonetheless, the effect on macrosurgical skills of microsurgical training has never been studied in undergraduate medical students. In Norway, microsurgical training is not normally included in the undergraduate curriculum. It is taught to plastic surgeons in training through rat models and clinical practice under supervision.
We hypothesize that microsurgical training might give insight into the importance of delicate tissue handling and correct knot tying that could have a positive influence on macrosurgical skills. The primary aim of this study was to evaluate the effect of microsurgical training on macrosurgical suturing skills in novice medical students. The secondary aim was to investigate the effect of microsurgical training on students’ attitudes to plastic surgery as a career choice.
Methods and subjects
Subjects
The subjects were recruited to the study in January 2018. Inclusion criteria consisted of preclinical medical students with no prior suturing experience of any form. Exclusion criteria consisted of the inability to give informed consent or understand Norwegian. An e-mail containing information on the study and an invitation to participate was sent to all first- and second-year medical students at the University of Bergen. The first 46 students who wanted to participate and met the inclusion criteria were enrolled in the study.
Interventions
Prior to randomization, all participants were taught macrosurgical suturing skills in a pretrial course. The training was set up as a 45-min lecture covering the basics of suturing. This was then followed by a plastic surgeon demonstrating the correct suturing technique. All subjects were allocated 60 min to practice under supervision.
The intervention group received an additional 45-min lecture and demonstration of microsurgical suturing technique and instrument handling. The lecture was followed by a supervised practice session of 120 min duration, comprising a latex model and a silicone tube anastomosis (Fig. 1). Simple microsurgical sutures in rubber [26] and silicone tube anastomoses [27] have been validated as valuable training models for microsurgery, confirmed by a recent systematic review [28], and are typically the first step in microsurgery courses [21]. In the latex model, four pieces of 3 by 3 cm squares cut from operating gloves were mounted onto a stable surface. The latex squares had one centrally placed cut, and each square had the cut placed in a different direction, to enable practice of adaptation of the edges in different angles [29]. The silicone tube had a diameter of 1.85 mm and a wall thickness of 0.30 mm (Fig. 1). The microsurgical suturing was performed using stereo surgical lab microscopes, Zeiss OPMI® pico (Carl Zeiss AG, Oberkochen, Germany) and AmScope 3.5X-45X Simul-Focal Trinocular Zoom Stereo Microscope (AmScope, Irvine, CA, USA). The control group concurrently received an additional 60 min supervised macrosurgical training time to compensate for the lack of microsurgical practice. All the subjects wore surgical gloves when practicing and during the examination.
Assessment test
Both groups were filmed performing the same macrosurgical tasks of three simple cutaneous interrupted sutures with a square knot and a continuous cutaneous three-stitch long over-and-over suture. The intervention group and controls used the same types of needle holders, forceps, scissors, and 3-0 Nylon sutures. The maximum time allowed to complete the task was 15 min.
The intervention group also performed a microsurgical skills test consisting of a latex-cut adaptation by three interrupted sutures and a silicone tube anastomosis (Fig. 1). The test was performed using a standard set of microsurgical instruments and a 9-0 Nylon suture. If the subject was able to perform the test in 45 min or less, it was considered successful.
Filming process
Both the intervention group and the controls were filmed individually performing the macrosuturing tasks in a separate room. All tasks were filmed after the above-described training and practice, in a standardized fashion, and the video of each student included the full length of the assessment test. The field of view was the simulated operating table and the subjects’ gloved hands.
Assessment of suturing skills
Four independent assessors, three experienced specialists in plastic surgery and one newly graduated doctor, rated the macrosurgery video recordings independently. All assessors were sent the video clips with muted sound, and each video showed a student from the intervention group or the control group performing the task. The assessors were blinded to the subjects’ identity and to whether they were intervention group or controls.
The calculated time for the macrosurgical test was the total time incurred for each task (completion time simple suture + completion time continuous suture). Total cutoff times for both tasks were calculated so that 2/3 of the post-course subjects fell within it. Two assessment tools were used to assess macrosurgical performances: the University of Bergen suturing skills assessment tool (UBAT) and the Objective Structured Assessment of Technical Skill global rating scale (OSATS).
The UBAT (Table 1) has been validated [30] and includes both macrosurgical and microsurgical quality indicators. The instrument includes eight yes or no questions: whether the subject grabs the needle with the instruments (and not with the fingers), holds the forceps correctly, penetrates the tissue with a 90° angle (penetrates and pulls needle out on the curve), grabs the suture (thread) in a correct fashion (not in a way that potentially could lead to suture breakage), manages the suture without tangling the ends in the knot, ties a correct square knot, makes parallel sutures (equal length from the wound edge and equal depth on both sides) and gentle tissue handling. The total time to complete the two tasks was recorded in seconds. A total score was calculated as cutoff time (min) − completion time (min) + (8 − number of errors). Higher scores indicate better performance.
The OSATS [3, 31, 32] evaluates macroscopic suturing qualities in seven domains: respect for tissue, time and motion, instrument handling, knowledge of instruments, flow of operation, use of assistants, and knowledge of specific procedure. A score on a 5-point scale is given for each domain, and a total score from a maximum of 35 (7 × 5) is awarded [3, 31]. For the purpose of video assessment, only the four domains applicable to a controlled lab setting were used: respect for tissue, time and motion, instrument handling, knowledge of instruments. Hence, the maximum achievable score was 20.
The microsurgical tasks were assessed using the University of Western Ontario Microsurgery Skills Acquisition/Assessment instrument (UWOMSA) that evaluates microsurgical suturing technique. It has three individually scored categories: quality of knot, efficiency, and handling. Each category can be awarded a maximum of 5 points, and a global score, with a maximum of 15, is calculated. Higher scores indicate better performance [33, 34]. Only the “Knot tying module” was used in this study. The scoring was performed in real-time by two microsurgeons. The real-time approach was chosen to limit the number of films the experts had to view and thereby prevent assessors’ fatigue.
Questionnaires
Prior to the randomization process, and then following the tests, each participant was asked to fill out a questionnaire containing questions on future specialty ambitions and attitude to plastic surgery. The questionnaire was an abbreviated version of a previously used questionnaire [35].
Statistics
The number of subjects included in the study was based on a power analysis of the UBAT total score [30]. Assuming a target difference between the groups of at least 2.3 (SD 2.7), 46 subjects (23 in each group) would be needed to give the study 81% power (for a type I error rate of 5%).
The subjects were randomized into two equal groups using R version 3.4.1 [36], an intervention group that received both macro- and microsurgical training and a control group that received macrosurgical training only.
We report categorical data as counts and percentages, and continuous data as means and differences of means, along with confidence intervals and dot plots of the individual values. To compare proportions between the intervention and control groups, we used Fisher’s mid-P test, and to compare continuous data, we used Welch’s t test (a t test that does not assume equal variances between groups).
For students who did not finish the macrosurgical test within the allotted 15 min, the time used in the analyses was set to 15 min. All UBAT total scores, individual quality variables, and the OSATS scores were averaged over the four raters before analysis. We also present the ICC(A,1) value for the UBAT scores (two-way random effects model for absolute agreement). This measures agreement across raters (compared the variation between students).
The data were stored in Stata version 15.1 [37] data files and analyzed using R version 3.4.1 [36]. All reported confidence intervals are 95% confidence intervals, and p values ≤ 0.05 are considered statistically significant.
Ethics
The Regional Committee for Medical and Health Research Ethics reviewed the study protocol, and it was concluded that Norwegian law on research ethics and medical research does not require an ethical permit for this type of study (2017/1098, REK-nord). The notification test of the Norwegian Centre for Research Data (NSD) [38] was performed and concluded that the projects were not subject to notification. The Declaration of Helsinki was followed, and all participants gave their written informed consent to participate.
Results
One of the controls did not show up, and hence 23 intervention group subjects and 22 control subjects were filmed and evaluated. Seventy-four percent (17/23) of the intervention group were able to complete the microsurgical skills test adequately, and 82% (19/23) were able to complete the macrosurgical task within the time limit. Ninety-five percent (21/22) of controls completed the macrosurgical task in within the time limit. There was a median of 3 days (range 1–4) between training and test (mean 3.1, SD 1.3).
The cutoff time to complete the two macrotasks (calculated so that 67% of all the subjects fell within in it), was 718 s. The intervention group needed a longer time to complete the tasks (mean 733 s) than the controls (mean 574 s) (CI for the difference 79–238, p < 0.001) (Fig. 2a). The mean number of correct UBAT quality variables (8—number of errors) was slightly lower in the intervention group (5.9) than in the controls (6.6) (CI for difference 0.2–1.4, p = 0.015) (Fig. 2b, Table 2). The largest difference was found for the variable “grabs the suture using the instruments (in a way that potentially could lead to suture breakage).” There was also a tendency to hold the macroinstruments in the same way as microinstruments are held (Fig. 3). None of the controls held the instruments in this fashion. Participants who needed more time to complete the tasks made more mistakes, as measured with UBAT, than faster participants (Pearson correlation 0.54, CI 0.25–0.70, p < 0.001). The controls achieved a higher total score than the intervention group (9.0 vs. 5.6, p < 0.001) (Fig. 2c, Table 3). The same could be seen for the total OSATS score, as the intervention group achieved a mean score of 11.1 and the controls 13.1 (p < 0.001) (Table 3). The ICC total score showed good agreement between the raters, ICC(A,1) = 0.84 (CI 0.72–0.91). The different time intervals between the macrosurgical training and skills test were not associated with score differences (Pearson correlation − 0.06, p = 0.87).
No correlation was found between the performances in the microsurgical skills test (UWOMSA score) and the macrosurgical skills test (UBAT, p = 0.44), though there was a moderate, but not statistically significant, correlation between the microsurgical UWOMSA score and the macrosurgical OSATS score (0.4, CI 0.0–0.7, p = 0.05). Time spent to complete the microsurgical task did not predict time needed to complete the macrosurgical task (p = 0.38).
The preintervention questionnaire revealed that 30% of the participants wish to pursue a surgical career in the future (Fig. 4). When explicitly asked about plastic surgery, 18 (18/46, 39%) stated that they are considering it as a future career. As regards to their most important source of knowledge of plastic surgery, 24 participants (24/46, 52%) stated the media, 14 (14/46, 30%) stated medical school, and the rest claimed “other sources.” When the participants rated their knowledge in plastic surgery on a 1–5 scale, with 5 being the top score, 23 rated their knowledge “1” (50%), 19 “2” (41%), 2 “3” (4%), 2 “4” (4%), and none “5.”
After the course, 21/23 in the intervention group (91%) and 11/22 controls (50%) stated that the course had made them more interested in plastic surgery, while the remaining subjects had not changed their opinion of the specialty. Hence, the microcourse tended to influence the students towards a wish to become plastic surgeons more than the macrocourse did (p = 0.002). In addition, the intervention group was slightly happier with the training received compared with the controls (4.7 vs. 4.4 on a 1–5 scale, p = 0.02).
Discussion
This is the first study on the effect of microsurgical training on macrosurgical skills in undergraduate medical students. It has been hypothesized that microsurgical training might be beneficial for most surgeons [17, 18], as it could lead to a more skillful tissue handling and improved control of instruments and suture placing [17]. Nonetheless, there are no studies on transferability of microsurgical skills to a macrosurgical setting. However, our randomized controlled study unexpectedly demonstrated poorer macrosurgical skills in the group of medical students exposed to microsurgical training.
A previous study has estimated that a medical student requires about 15 days of 7 to 8 h daily training to fully master microsurgical suturing technique [21]. Other studies that have taught microsurgery to medical students have also exposed the students to several regular training sessions [20, 23]. In this study, the intervention group was given a total of 120 min to practice microsurgical suturing. Hence, even though the subjects were able to perform the given tasks, they still have to be considered as novices after the training. There are many conditions that novice subjects have to adjust to before actually learning to suture, such as visuospatial orientation and loss of depth perception and dexterity when using the microscope. The intervention group might have been fatigued by all these other aspects they had to master, so that, ultimately, the actual suturing skills suffered and became secondary. It might also be that the intervention group had reached their maximum learning threshold for one given simulation [39]. The fact that the intervention group needed longer time and committed more errors than the controls could be an indication of this.
On the other hand, the intervention group’s time consumption could also indicate that these subjects had acquired a greater respect for tissue handling, a quality that is difficult to measure in non-live models. The most common error committed by the intervention group was in the indicator “grabs the suture (thread) in a correct fashion,” where they tended to grab both ends of the suture using the instruments, something that is actually “acceptable” in microsurgical practice. There was also a tendency to hold the macroinstruments in the same way that microinstruments are held. This could suggest that the novice subjects transfer some of the microsurgical skills they have learned to the macrosurgical setting. In summary, the effect of microsurgery on macrosurgical skills might be underestimated in this short-time exposure study. More exposure and more training are necessary to evaluate the true effect of microsurgical training on macrosurgical suturing. In skill teaching in general, several short sessions are known to improve skill retention when compared to a long single session [40]. In addition, regular reinforcements are necessary to retain the knowledge and skills achieved [11].
Another possible explanation of the worse scores amongst the intervention group might be the fact that the control group received an additional 60 min supervised macrosurgical training time whilst the former group was undertaking their microsurgical training. Thus, it is feasible that the more prolonged exposure to macrosurgical training was significant and highlights a slight limitation to the current study. Furthermore, the lack of a statistical relationship between the microsurgical and macrosurgical performances within the intervention group lends support to this theory. The order in which the subjects received macro- and microsurgical training could also have affected the results. In addition, another possible explanation for these results could be differences in technical aptitude amongst the subjects in the two groups. The inclusion of clinical students, who have already completed certain aptitude tests as a prerequisite for inclusion, could have compensated for this. A future study should comprise of identical macrosurgical training times prior to testing, or students in their clinical years who are already familiar with macrosurgical suturing.
Previous studies have demonstrated that encounters with microsurgery in medical school can motivate the students to want to become plastic surgeons [20,21,22]. The same effect was observed in this study. Nonetheless, students’ career aspirations tend to vary with time [41, 42]. It has to be kept in mind that the students in this study are preclinical students who have not yet been exposed to clinical rotations [43]. More students in this study wanted to become surgeons (30%) than amongst clinical Norwegian medical students in general (17%) [35]. Nonetheless, in preclinical students, future career wishes are based principally on preconceived assumptions and not by exposure to and actual knowledge about what the different specialties entail [41, 42]. Hence, the figure of 30% has to be interpreted with some caution, even though a selection bias could have existed in which students with an interest in surgery self-selected for participation in this study. To evaluate the effect of microsurgical training on students’ career aspirations and actual specialty choice a longer follow-up is necessary. This could also be tested for by providing the microsurgical and macrosurgical training to all students in a class and then determine if more students ultimately apply to surgical fields than the average from our medical school.
In conclusion, more prolonged exposure and more frequent training than one session of 120 min are necessary to evaluate the true effect of microsurgical training on macrosurgical suturing skills. In addition, a future study should include two groups receiving the same length of macrosurgical training. Nonetheless, there are indications that novice students may transfer some microsurgical skills to the macrosurgical setting when they receive microsurgery practice. Microsurgical training could positively influence students towards a surgical career. The benefit of microsurgical training in medical students needs to be further investigated.
References
Almeland SK, Lindford A, Berg JO, Hansson E (2018) A core undergraduate curriculum in plastic surgery - a Delphi consensus study in Scandinavia. J Plastic Surg Hand Surg 52(2):97–105 Epub 2017/07/09
Tan SS, Sarker SK (2011) Simulation in surgery: a review. Scott Med J 56(2):104–109 Epub 2011/06/15
Ahmed K, Miskovic D, Darzi A, Athanasiou T, Hanna GB (2011) Observational tools for assessment of procedural skills: a systematic review. Am J Surg 202(4):469–480 e6
Rufai SR, Holland LC, Dimovska EO, Bing Chuo C, Tilley S, Ellis H (2016) A national survey of undergraduate suture and local anesthetic training in the United Kingdom. Journal of surgical education 73(2):181–184 Epub 2016/02/13
Morris MC, Gallagher TK, Ridgway PF (2012) Tools used to assess medical students competence in procedural skills at the end of a primary medical degree: a systematic review. Medical Education online 17 Epub 2012/08/29
Davis CR, Toll EC, Bates AS, Cole MD, Smith FCT (2014) Surgical and procedural skills training at medical school – a national review. Int J Surg 12(8):877–882
Hanson C, Mossey P, Macluskey M (2010) The assessment of suturing skills of dental undergraduates. Eur J Dental Educ : Off J Assoc Dental Educ Eur 14(2):113–117 Epub 2010/06/05
Pender C, Kiselov V, Yu Q, Mooney J, Greiffenstein P, Paige JT (2017) All for knots: evaluating the effectiveness of a proficiency-driven, simulation-based knot tying and suturing curriculum for medical students during their third-year surgery clerkship. Am J Surg 213(2):362–370 Epub 2016/09/20
Yap R, Moreira A, Wilkins S, Reeves F, Levinson M, McMurrick P (2016) Suturing in small group teaching settings: a modification to Peyton’s four-step approach. Med Sci Educ 26(4):575–580
Macluskey M, Durham J, Balmer C, Bell A, Cowpe J, Dawson L et al (2011) Dental student suturing skills: a multicentre trial of a checklist-based assessment. Eur J Dental Educ : Off J Assoc Dental Educ Eur 15(4):244–249 Epub 2011/10/12
Macluskey M, Hanson C (2011) The retention of suturing skills in dental undergraduates. Eur J Dental Educ : Off J Assoc Dental Educ Eur 15(1):42–46 Epub 2011/01/14
Nousiainen M, Brydges R, Backstein D, Dubrowski A (2008) Comparison of expert instruction and computer-based video training in teaching fundamental surgical skills to medical students. Surgery. 143(4):539–544 Epub 2008/04/01
Liddell MJ, Davidson SK, Taub H, Whitecross LE (2002) Evaluation of procedural skills training in an undergraduate curriculum. Med Educ 36(11):1035–1041 Epub 2002/10/31
Gershuni V, Woodhouse J, Brunt LM (2013) Retention of suturing and knot-tying skills in senior medical students after proficiency-based training: results of a prospective, randomized trial. Surgery. 154(4):823–829 discussion 9-30
Brunt LM, Halpin VJ, Klingensmith ME, Tiemann D, Matthews BD, Spitler JA et al (2008) Accelerated skills preparation and assessment for senior medical students entering surgical internship. J Am Coll Surg 206(5):897–904 discussion −7
Tamai S (2009) History of microsurgery. Plast Reconstr Surg 124(6 Suppl):e282–e294 Epub 2010/01/09
Di Cataldo A, Li Destri G, Trombatore G, Papillo B, Racalbuto A, Puleo S (1998) Usefulness of microsurgery in the training of the general surgeon. Microsurgery. 18(8):446–448
Ko JW, Lorzano A, Mirarchi AJ (2015) Effectiveness of a microvascular surgery training curriculum for orthopaedic surgery residents. J Bone Joint Surg Am 97(11):950–955 Epub 2015/06/05
McAnena PF, O'Halloran N, Moloney BM, Courtney D, Waldron RM, Flaherty G, Kerin MJ (2018) Undergraduate basic surgical skills education: impact on attitudes to a career in surgery and surgical skills acquisition. Ir J Med Sci 187(2):479–484 Epub 2017/10/19
Mucke T, Borgmann A, Ritschl LM, Kesting MR, Loeffelbein DJ, Wolff KD (2013) Microvascular training of medical students and surgeons - a comparative prospective study. J Craniomaxillofac Surg 41(8):e187–e190
Onoda S, Kimata Y, Sugiyama N, Tokuyama E, Matsumoto K, Ota T, Thuzar M (2016) Analysis of 10-year training results of medical students using the microvascular research center training program. J Reconstr Microsurg 32(5):336–341 Epub 2015/12/05
Beier JP, Horch RE, Boos AM, Taeger CD, Breuer G, Arkudas A. [Establishment and evaluation of a microsurgery course for medical students]. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse 2015;47(6):400-7. Epub 2015/12/18. Etablierung und Evaluation eines Mikrochirurgie - Kurses fur Medizinstudierende
Scholz M, Mucke T, Holzle F, Schmieder K, Engelhardt M, Pechlivanis I et al (2006) A program of microsurgical training for young medical students: are younger students better? Microsurgery. 26(6):450–455 Epub 2006/08/23
Sudario-Lumague R, Chiang YC, Lin TS (2018) Gender comparison of medical student microsurgical skills in a laboratory model. J Reconstr Microsurg 34(5):359–362 Epub 2018/02/17
Zhang F, Dorsett-Martin W, Fischer K, Angel M, Buncke HJ, Lineaweaver WC (2001) Role of medical students in microsurgery research. J Reconstr Microsurg 17(2):89–93 Epub 2001/04/20
Furka I, Brath E, Nemeth N, Miko I (2006) Learning microsurgical suturing and knotting techniques: comparative data. Microsurgery. 26(1):4–7 Epub 2006/01/31
Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, Jarvi KA (2004) The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg 240(2):374–381 Epub 2004/07/27
Dumestre D, Yeung JK, Temple-Oberle C (2014) Evidence-based microsurgical skill-acquisition series part 1: validated microsurgical models--a systematic review. J Surg Educ 71(3):329–338
Acland RD, Sabapathy SR. Practice manual for microvascular surgery: Indian Society for Surgery of the Hand; 2008
Sundhagen HP, Almeland SK, Hansson E (2018) Development and validation of a new assessment tool for suturing skills in medical students. Eur J Plast Surg 41(2):207–216 Epub 2018/04/03
Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, Brown M (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84(2):273–278
Faulkner H, Regehr G, Martin J, Reznick R (1996) Validation of an objective structured assessment of technical skill for surgical residents. Acad Med : J Assoc Am Med Coll 71(12):1363–1365
Temple CL, Ross DC (2011) A new, validated instrument to evaluate competency in microsurgery: the University of Western Ontario Microsurgical Skills Acquisition/Assessment instrument [outcomes article]. Plast Reconstr Surg 127(1):215–222
Dumestre D, Yeung JK, Temple-Oberle C (2015) Evidence-based microsurgical skills acquisition series part 2: validated assessment instruments--a systematic review. J Surg Educ 72(1):80–89
Almeland SK, Guttormsen AB, de Weerd L, Nordgaard HB, Freccero C, Hansson E (2017) Plastic surgery in the Norwegian undergraduate medical curriculum: students’ knowledge and attitudes. A nationwide case-control study. J Plastic Surg Hand Surg 51(2):136–142 Epub 2016/07/09
R Core Team (2017). R: a language and environment for statistical computing. R Foundation for statistical computing, Vienna, Austria. URL https://www.R-project.org/
StataCorp. Stata Statistical Software: Release 15. . College Station, TX: StataCorp LLC 2017
Norsk senter for forskningsdata (NSD). Do I have to notify my project? URL http://www.nsd.uib.no/personvernombud/en/notify. [cited 2018 Jan 20]; Available from: http://www.nsd.uib.no/personvernombud/en/notify
Guadagnoli MA, Lee TD (2004) Challenge point: a framework for conceptualizing the effects of various practice conditions in motor learning. J Mot Behav 36(2):212–224 Epub 2004/05/08
Moulton CA, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R (2006) Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg 244(3):400–409
Aasland OG, Rovik JO, Wiers-Jenssen J. [Motives for choice of specialty during and after medical school]. Tidsskr Nor Laegeforen. 2008;128(16):1833-7. Epub 2008/09/13. Legers Motiver for valg av spesialitet under og etter studiet
Wiers-Jenssen J, Aasland OG. [Changes in career plans of medical students during the first half of medical school]. Tidsskr Nor Laegeforen. 1999;119(19):2858-64. Epub 1999/09/24. Endring i medisinstudenters karrierepreferanser under forste del av studiet
Grigg M, Arora M, Diwan AD (2014) Australian medical students and their choice of surgery as a career: a review. ANZ J Surg 84(9):653–655 Epub 2013/10/10
Acknowledgments
We would like to thank the volunteering medical students at the University of Bergen.
Funding
Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stian Kreken Almeland, Andrew Lindford, Henriette Pisani Sundhagen, Karl Ove Hufthammer, Eivind Strandenes, Henrik Løvendahl Svendsen, Anne Berit Guttormsen, and Emma Hansson declare that they have no conflict of interest.
Ethical approval
The Regional Committee for Medical and Health Research Ethics reviewed the study protocol, and it was concluded that Norwegian law on research ethics and medical research does not require an ethical permit for this type of study (2017/1098, REK-nord).
Informed consent
All participants gave their written informed consent to participate.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Almeland, S.K., Lindford, A., Sundhagen, H.P. et al. The effect of microsurgical training on novice medical students’ basic surgical skills—a randomized controlled trial. Eur J Plast Surg 43, 459–466 (2020). https://doi.org/10.1007/s00238-019-01615-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-019-01615-w