Abstract
Background
Post-operative monitoring of flap is equally important as harvesting of a flap. Early diagnosis of flap failure can salvage the flap by appropriate intervention. The monitoring methods used should be rapid, inexpensive, and accurate. The purpose of this study is to evaluate the usefulness of blood glucose monitoring (BGM) of the flap as our monitoring modality.
Methods
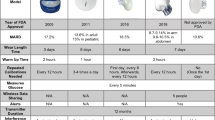
This study includes 60 flaps which were monitored by measuring their capillary glucose level by pricking the distal end of the flap. Out of the 60 flaps, 18 were free flaps, 23 were pedicled, and 19 were of the random variety. Quantitative data was expressed in frequency, percentage, mean value, and standard deviation for capillary glucose levels of the flap.
Result
Out of the 60 flaps, 44 survived well, 10 flaps were having minor distal necrosis (< 10% of flap area), major flap necrosis occurred in 3 flaps while 3 flaps failed completely. Failed flaps have shown lower glucose levels. Using the receiver operating characteristic curve (ROC), the cutoff value for BGM was 61 mg/dl, with a sensitivity of 93% and a specificity of 80%.
Conclusion
Blood glucose monitoring reveals the state of perfusion of the flap in the postoperative period. Flap capillary glucose levels less than 61 mg/dl is suggestive of ischemia of the flap with a sensitivity and a specificity of 93% and 80%, respectively. It has prognostic value as it allows early detection of vascular compromise and also defines the forthcoming line of demarcation in partial necrosis.
Level of Evidence: Type IV, diagnostic study.




Similar content being viewed by others
References
Biemer E (1981) Salvage operations for complication following replantation and free tissue transfer. Int Surg 66(1):37–38
Genden EM, Rinaldo A, Suárez C, Wei WI, Bradley PJ, Ferlito A (2004) Complications of free flap transfers for head and neck reconstruction following cancer resection. Oral Oncol 40(10):979–984
Neligan PC (1993) Monitoring techniques for the detection of flow failure in the postoperative period. Microsurgery 14(3):162–164
Rodjmark J et al (2000) Comparison of flap ischaemia induced by arterial or venous occlusion in pigs with aid of microdialysis. Eur J Plast Surg 23(5):278–282
Hutchinson DT (1993) Color duplex imaging. Applications to upper-extremity and microvascular surgery. Hand Clin 9(1):47–57
Thorniley MS, Sinclair JS, Barnett NJ, Shurey CB, Green CJ (1998) The use of near-infrared spectroscopy for assessing flap viability during reconstructive surgery. Br J Plast Surg 51(3):218–226
Yuen JC, Feng Z (2000) Monitoring free flaps using the laser Doppler flowmeter: five-year experience. Plast Reconstr Surg 105(1):55–61
Sitzman TJ, Hanson SE, King TW, Gutowski KA (2010) Detection of flap venous and arterial occlusion using interstitial glucose monitoring in a rodent model. Plast Reconstr Surg 126(1):71–79
Sakakibara S, Hashikawa K, Omori M, Terashi H, Tahara S (2010) A simplest method of flap monitoring. J Reconstr Microsurg 26(07):433–434
Tonyushkina K, Nichols JH (2009) Glucose meters: a review of technical challenges to obtaining accurate results. J Diabetes Sci Technol Online 3(4):971–980
Mathes. Plastic surgery, general principal. Vol. 1. Saunders; 496–497 p
Hara H, Mihara M, Iida T, Narushima M, Todokoro T, Yamamoto T, Koshima I (2012) Blood glucose measurement for flap monitoring to salvage flaps from venous thrombosis. J Plast Reconstr Aesthet Surg 65(5):616–619
Setälä LP, Korvenoja EM-L, Härmä MA, Alhava EM, Uusaro AV, Tenhunen JJ (2004) Glucose, lactate, and pyruvate response in an experimental model of microvascular flap ischemia and reperfusion: a microdialysis study. Microsurgery 24(3):223–231
Jyranki J et al (2006) Microdialysis in clinical practice: monitoring intraoral free flaps. Ann Plastic Surg 56(4):387–393
Wax MK (2014) The role of the implantable Doppler probe in free flap surgery: Doppler use in monitoring of free flaps. Laryngoscope 124(S1):S1–S12
Frost et al (2015) Direct comparison of postoperative monitoring of free flaps with microdialysis, implantable cook-Swartz Doppler probe, and clinical monitoring in 20 consecutive patients: postoperative monitoring in 20 consecutive patients. Microsurgery 35(4):262–271
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study is funded by Institutional Review Board, Christian Medical College, Vellore Tamil Nadu (India).
Conflict of interest
Mukesh Kumar Sharma, Geley Ete, Gaurav Chaturvedi, Elvino Barreto, and Kingsly Paul Meetper Doss declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Patients consent
Patients provided written consent for the use of their images.
Rights and permissions
About this article
Cite this article
Sharma, M.K., Ete, G., Chaturvedi, G. et al. Prospective analysis of flap perfusion by measuring capillary glucose level in flaps. Eur J Plast Surg 42, 119–124 (2019). https://doi.org/10.1007/s00238-018-1464-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-018-1464-6