Abstract
Purpose
MELAS syndrome is a genetic disorder caused by mitochondrial DNA mutations. We previously described that MELAS patients had increased CSF glutamate and decreased CSF glutamine levels and that oral glutamine supplementation restores these values. Proton magnetic resonance spectroscopy (1H-MRS) allows the in vivo evaluation of brain metabolism. We aimed to compare 1H-MRS of MELAS patients with controls, the 1H-MRS after glutamine supplementation in the MELAS group, and investigate the association between 1H-MRS and CSF lactate, glutamate, and glutamine levels.
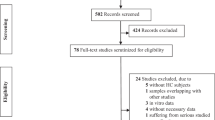
Methods
We conducted an observational case–control study and an open-label, single-cohort study with single-voxel MRS (TE 144/35 ms). We assessed the brain metabolism changes in the prefrontal (PFC) and parieto-occipital) cortex (POC) after oral glutamine supplementation in MELAS patients. MR spectra were analyzed with jMRUI software.
Results
Nine patients with MELAS syndrome (35.8 ± 3.2 years) and nine sex- and age-matched controls were recruited. Lactate/creatine levels were increased in MELAS patients in both PFC and POC (0.40 ± 0.05 vs. 0, p < 0.001; 0.32 ± 0.03 vs. 0, p < 0.001, respectively). No differences were observed between groups in glutamate and glutamine (Glx/creatine), either in PFC (p = 0.930) or POC (p = 0.310). No differences were observed after glutamine supplementation. A positive correlation was found between CSF lactate and lactate/creatine only in POC (0.85, p = 0.003).
Conclusion
No significant metabolite changes were observed in the brains of MELAS patients after glutamine supplementation. While we found a positive correlation between lactate levels in CSF and 1H-MRS in MELAS patients, we could not monitor treatment response over short periods with this tool.
Trial registration
ClinicalTrials.gov Identifier: NCT04948138; initial release 24/06/2021; first patient enrolled on 1/07/2021. https://clinicaltrials.gov/ct2/show/NCT04948138


Similar content being viewed by others
Data availability
Data available on request from the authors.
References
Hirano M, Ricci E, Koenigsberger MR, Defendini R, Pavlakis SG, DeVivo DC, DiMauro S, Rowland LP (1992) Melas: an original case and clinical criteria for diagnosis. Neuromuscul Disord 2:125–135
El-Hattab AW, Adesina AM, Jones J, Scaglia F (2015) MELAS syndrome: clinical manifestations, pathogenesis, and treatment options. Mol Genet Metab 116(1–2):4–12. https://doi.org/10.1016/j.ymgme.2015.06.004
Cheng W, Zhang Y, He L (2022) MRI Features of stroke-like episodes in mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes. Front Neurol 9(13):843386. https://doi.org/10.3389/fneur.2022.843386
Guerrero-Molina MP, Morales-Conejo M, Delmiro A et al (2022) Elevated glutamate and decreased glutamine levels in the cerebrospinal fluid of patients with MELAS syndrome. J Neurol 269(6):3238–3248. https://doi.org/10.1007/s00415-021-10942-7
Ankarcrona M, Dypbukt JM, Bonfoco E, Zhivotovsky B, Orrenius S, Lipton SA, Nicotera P (1995) Glutamate-induced neuronal death: a succession of necrosis or apoptosis depending on mitochondrial function. Neuron 15(4):961–973. https://doi.org/10.1016/0896-6273(95)90186-8
Moore HL, Blain AP, Turnbull DM, Gorman GS (2020) Systematic review of cognitive deficits in adult mitochondrial disease. Eur J Neurol 27(1):3–17. https://doi.org/10.1111/ene.14068
Finsterer J (2008) Cognitive decline as a manifestation of mitochondrial disorders (mitochondrial dementia). J Neurol Sci 272(1–2):20–33. https://doi.org/10.1016/j.jns.2008.05.011
González de la Aleja J, Ramos A, Mato-Abad V, Martínez-Salio A, Hernández-Tamames JA, Molina JA, Hernández-Gallego J, Alvarez-Linera J (2013) Higher glutamate to glutamine ratios in occipital regions in women with migraine during the interictal state. Headache. 53(2):365–75. https://doi.org/10.1111/head.12030
Zielman R, Wijnen JP, Webb A et al (2017) Cortical glutamate in migraine. Brain 140(7):1859–1871. https://doi.org/10.1093/brain/awx130
Çavus I, Romanyshyn JC, Kennard JT et al (2016) Elevated basal glutamate and unchanged glutamine and GABA in refractory epilepsy: microdialysis study of 79 patients at the yale epilepsy surgery program. Ann Neurol 80(1):35–45. https://doi.org/10.1002/ana.24673
Chan F, Lax NZ, Voss CM et al (2019) The role of astrocytes in seizure generation: insights from a novel in vitro seizure model based on mitochondrial dysfunction. Brain 142(2):391–411. https://doi.org/10.1093/brain/awy320
Guerrero-Molina MP, Morales-Conejo M, Delmiro A, et al (2022) High-dose oral glutamine supplementation reduces elevated glutamate levels in cerebrospinal fluid in patients with mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes syndrome [published online ahead of print, 2022 Nov 5]. Eur J Neurol. https://doi.org/10.1111/ene.15626. https://doi.org/10.1111/ene.15626
Ito H, Mori K, Harada M et al (2008) Serial brain imaging analysis of stroke-like episodes in MELAS. Brain Dev 30(7):483–488. https://doi.org/10.1016/j.braindev.2008.01.003
Weiduschat N, Kaufmann P, Mao X, Engelstad KM, Hinton V, DiMauro S et al (2014) Cerebral metabolic abnormalities in A3243G mitochondrial DNA mutation carriers. Neurology 82:798–805. https://doi.org/10.1212/WNL.0000000000000169
Lee HN, Yoon CS, Lee YM (2018) Correlation of serum biomarkers and magnetic resonance spectroscopy in monitoring disease progression in patients with mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes due to mtDNA A3243G mutation. Front Neurol 27(9):621. https://doi.org/10.3389/fneur.2018.00621
Hovsepian DA, Galati A, Chong RA, Mazumder R, DeGiorgio CM, Mishra S, Yim C (2019) MELAS: Monitoring treatment with magnetic resonance spectroscopy. Acta Neurol Scand 139(1):82–85. https://doi.org/10.1111/ane.13027
Pavlakis SG, Phillips PC, DiMauro S, De Vivo DC, Rowland LP (1984) Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes: a distinctive clinical syndrome. Ann Neurol 16(4):481–488. https://doi.org/10.1002/ana.410160409
Naressi A, Couturier C, Devos JM et al (2001) Java-based graphical user interface for the MRUI quantitation package. MAGMA 12(2–3):141–152. https://doi.org/10.1007/BF02668096
Stefan D, Cesare FD, Andrasescu A, Popa E, Lazariev A, Vescovo E et al (2009) Quantitation of magnetic resonance spectroscopy signals: the jMRUI software package. Meas Sci Technol 20:104035
Vanhamme L, van den Boogaart A, Van Huffel S (1997) Improved method for accurate and efficient quantification of MRS data with use of prior knowledge. J Magn Reson 129(1):35–43. https://doi.org/10.1006/jmre.1997.1244
Bernabeu A, Alfaro A, García M, Fernández E (2009) Proton magnetic resonance spectroscopy (1H-MRS) reveals the presence of elevated myo-inositol in the occipital cortex of blind subjects. Neuroimage 47(4):1172–1176. https://doi.org/10.1016/j.neuroimage.2009.04.080
Curi R, Lagranha CJ, Doi SQ et al (2005) Molecular mechanisms of glutamine action. J Cell Physiol. 204(2):392–401. https://doi.org/10.1002/jcp.20339
Chen Q, Kirk K, Shurubor YI et al (2018) Rewiring of glutamine metabolism is a bioenergetic adaptation of human cells with mitochondrial DNA mutations. Cell Metab 27(5):1007-1025.e5. https://doi.org/10.1016/j.cmet.2018.03.002
McKenna MC (2007) The glutamate-glutamine cycle is not stoichiometric: fates of glutamate in brain. J Neurosci Res 85(15):3347–3358. https://doi.org/10.1002/jnr.21444
Takado Y, Sato N, Kanbe Y et al (2019) Association between brain and plasma glutamine levels in healthy young subjects investigated by MRS and LC/MS. Nutrients. 11(7):1649. https://doi.org/10.3390/nu11071649. (Published 2019 Jul 19)
Wilichowski E, Pouwels PJ, Frahm J, Hanefeld F (1999) Quantitative proton magnetic resonance spectroscopy of cerebral metabolic disturbances in patients with MELAS. Neuropediatrics 30(5):256–263. https://doi.org/10.1055/s-2007-973500
Möller HE, Kurlemann G, Pützler M, Wiedermann D, Hilbich T, Fiedler B (2005) Magnetic resonance spectroscopy in patients with MELAS. J Neurol Sci 229–230:131–139. https://doi.org/10.1016/j.jns.2004.11.014
Wang R, Hu B, Sun C, Geng D, Lin J, Li Y (2021) Metabolic abnormality in acute stroke-like lesion and its relationship with focal cerebral blood flow in patients with MELAS: evidence from proton MR spectroscopy and arterial spin labeling. Mitochondrion 59:276–282. https://doi.org/10.1016/j.mito.2021.06.012
Kamada K, Takeuchi F, Houkin K et al (2001) Reversible brain dysfunction in MELAS: MEG, and (1)H MRS analysis. J Neurol Neurosurg Psychiatry 70(5):675–678. https://doi.org/10.1136/jnnp.70.5.675
Bianchi MC, Tosetti M, Battini R et al (2003) Proton MR spectroscopy of mitochondrial diseases: analysis of brain metabolic abnormalities and their possible diagnostic relevance. AJNR Am J Neuroradiol 24(10):1958–1966
Gramegna LL, Evangelisti S, Di Vito L et al (2021) Brain MRS correlates with mitochondrial dysfunction biomarkers in MELAS-associated mtDNA mutations. Ann Clin Transl Neurol 8(6):1200–1211. https://doi.org/10.1002/acn3.51329
Arun P, Moffett JR, Namboodiri AM (2009) Evidence for mitochondrial and cytoplasmic N-acetylaspartate synthesis in SH-SY5Y neuroblastoma cells. Neurochem Int 55(4):219–225. https://doi.org/10.1016/j.neuint.2009.03.003
Clark JB (1998) N-Acetyl Aspartate: a marker for neuronal loss or mitochondrial dysfunction. Dev Neurosci 20:271–276. https://doi.org/10.1159/000017321
Liu Z, Zheng D, Wang X et al (2011) Apparent diffusion coefficients of metabolites in patients with MELAS using diffusion-weighted MR spectroscopy. AJNR Am J Neuroradiol 32(5):898–902. https://doi.org/10.3174/ajnr.A2395
Castillo M, Kwock L, Green C (1995) MELAS syndrome: imaging and proton MR spectroscopic findings. AJNR Am J Neuroradiol 16(2):233–239
Clark JM, Marks MP, Adalsteinsson E et al (1996) MELAS: clinical and pathologic correlations with MRI, xenon/CT, and MR spectroscopy. Neurology 46(1):223–227. https://doi.org/10.1212/wnl.46.1.223
Kaufmann P, Shungu DC, Sano MC, Jhung S, Engelstad K, Mitsis E, Mao X, Shanske S, Hirano M, DiMauro S, De Vivo DC (2004) Cerebral lactic acidosis correlates with neurological impairment in MELAS. Neurology 62(8):1297–1302. https://doi.org/10.1212/01.wnl.0000120557.83907.a8
Magistretti PJ, Allaman I (2018) Lactate in the brain: from metabolic end-product to signalling molecule. Nat Rev Neurosci 19(4):235–249. https://doi.org/10.1038/nrn.2018.19
Vohra R, Kolko M (2020) Lactate: more than merely a metabolic waste product in the inner retina. Mol Neurobiol 57:2021–2037. https://doi.org/10.1007/s12035-019-01863-8
Benarroch EE (2016) Astrocyte signaling and synaptic homeostasis: II: astrocyte-neuron interactions and clinical correlations. Neurology 87(7):726–735. https://doi.org/10.1212/WNL.0000000000003019
Chen C, Xiong N, Wang Y et al (2012) A study of familial MELAS: evaluation of A3243G mutation, clinical phenotype, and magnetic resonance spectroscopy-monitored progression. Neurol India 60(1):86–89. https://doi.org/10.4103/0028-3886.93609
Boulanger Y, Labelle M, Khiat A (2000) Role of phospholipase A(2) on the variations of the choline signal intensity observed by 1H magnetic resonance spectroscopy in brain diseases. Brain Res Brain Res Rev 33(2–3):380–389. https://doi.org/10.1016/s0165-0173(00)00037-0
Iizuka T, Sakai F (2005) Pathogenesis of stroke-like episodes in MELAS: analysis of neurovascular cellular mechanisms. Curr Neurovasc Res 2(1):29–45. https://doi.org/10.2174/1567202052773544
Tetsuka S, Ogawa T, Hashimoto R, Kato H (2021) Clinical features, pathogenesis, and management of stroke-like episodes due to MELAS. Metab Brain Dis 36(8):2181–2193. https://doi.org/10.1007/s11011-021-00772-x
Ross BD (1991) Biochemical considerations in 1H spectroscopy. Glutamate and glutamine; myo-inositol and related metabolites. NMR Biomed. 4(2):59–63. https://doi.org/10.1002/nbm.1940040205
Mandal PK, Guha Roy R, Samkaria A, Maroon JC, Arora Y (2022) In vivo 13C magnetic resonance spectroscopy for assessing brain biochemistry in health and disease. Neurochem Res 47(5):1183–1201. https://doi.org/10.1007/s11064-022-03538-8
Pavlakis SG, Kingsley PB, Kaplan GP, Stacpoole PW, O’Shea M, Lustbader D (1998) Magnetic resonance spectroscopy: use in monitoring MELAS treatment. Arch Neurol 55(6):849–852. https://doi.org/10.1001/archneur.55.6.849
Niu FN, Meng HL, Chang LL et al (2017) Mitochondrial dysfunction and cerebral metabolic abnormalities in patients with mitochondrial encephalomyopathy subtypes: evidence from proton MR spectroscopy and muscle biopsy. CNS Neurosci Ther 23(8):686–697. https://doi.org/10.1111/cns.12714
Lee HN, Yoon CS, Lee YM (2018) Correlation of serum biomarkers and magnetic resonance spectroscopy in monitoring disease progression in patients with mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes due to mtDNA A3243G Mutation. Front Neurol. 9:621. https://doi.org/10.3389/fneur.2018.00621. (Published 2018 Jul 27)
Li Y, Lafontaine M, Chang S, Nelson SJ (2018) Comparison between short and long echo time magnetic resonance spectroscopic imaging at 3T and 7T for evaluating brain metabolites in patients with glioma. ACS Chem Neurosci 9(1):130–137. https://doi.org/10.1021/acschemneuro.7b00286
Lange T, Dydak U, Roberts TP, Rowley HA, Bjeljac M, Boesiger P (2006) Pitfalls in lactate measurements at 3T. AJNR Am J Neuroradiol 27(4):895–901
Funding
This research was supported by a grant from the Spanish Fundación Eugenio Rodríguez Pascual and the Fundación Mutua Madrileña. The financial sponsors had no role in the analysis or the development of conclusions. The investigators are solely responsible for the content and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study received approval from the Ethics Committee of the University Hospital 12 de Octubre (Madrid, Spain; approval number: 20/032).
Informed consent
All subjects provided written informed consent.
Conflict of interest
We have no Conflict of Interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guerrero-Molina, M.P., Bernabeu-Sanz, Á., Ramos-González, A. et al. Magnetic resonance spectroscopy in MELAS syndrome: correlation with CSF and plasma metabolite levels and change after glutamine supplementation. Neuroradiology 66, 389–398 (2024). https://doi.org/10.1007/s00234-023-03263-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-023-03263-1