Abstract
Purpose
Only a few studies are available on dose-related effects of sacubitril/valsartan (angiotensin receptor neprilysin inhibition (ARNI)) in real-life patients with heart failure and reduced ejection fraction (HFrEF). We sought to investigate clinical and functional effects in real-life HFrEF patients receiving ARNI at a different cumulative dose.
Methods
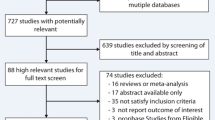
This was an observational study in consecutive outpatients admitted for HFrEF from October 2017 to June 2019. The PARADIGM criteria were needed for enrolment. ARNI was uptitrated according to blood pressure, drug tolerability, renal function and kaliemia. At least 10-month follow-up was required in each patient. Clinical assessment, Kansas City Cardiomyopathy Questionnaire (KCCQ) score, 6-min walk test and strain echocardiography were performed in each patient on a regular basis during the observational period. At the end of the study, patients were divided into two groups based on the median yearly dose of the ARNI medication.
Results
A total of 90 patients, 64 ± 11 years, 82% males, were enrolled. The cut-off dose was established in 75 mg BID, and the study population was divided into group A (≤ 75 mg), 52 patients (58%), and group B (> 75 mg), 38 patients (42%). The follow-up duration was 12 months (range 11–13). NYHA class, KCCQ score and 6MWT performance ameliorated in both groups, with a quicker time to benefit in group B. The proportion of patients walking > 350 m increased from 21 to 58% in group A (p < 0.001), and from 29 to 82% in group B (p < 0.001). A positive effect was also disclosed in the left ventricular remodelling, strain deformation and diastolic function.
Conclusion
One-year ARNI treatment was effective in our real-life HFrEF patient population, leading to clinical and functional improvement in both study groups, slightly greater and with a shorter time to benefit in group B.
Similar content being viewed by others
Introduction
Heart failure (HF) is the final stage of many cardiovascular diseases. Despite optimal medical therapy (OMT), HF with reduced ejection fraction (HFrEF) remains a central issue of clinical management, with high social and economic impact, worldwide [1,2,3]. Among the latest technological and pharmacological innovations, the sacubitril/valsartan drug combination, also known as angiotensin receptor neprilysin inhibitor (ARNI), has been demonstrated to get relevant benefits in this clinical setting [4,5,6,7,8]. Hence, neurohormonal modulation by ARNI has gradually become a landmark of HF treatment, but questions on its dose-dependent effectiveness are open yet [7,8,9].
We sought to evaluate clinical and functional effects in low- vs high-dose medication use in real-life HFrEF patients.
Methods
This was a prospective observational study conducted at Messina and Palermo University Hospitals (Italy). Among all outpatients admitted from October 2017 to June 2019 due to HFrEF from any aetiology, we enrolled those fulfilling the same inclusion criteria as in the PARADIGM-HF study [5]. Patients should have been New York Heart Association (NYHA) functional class II or III, clinically stable since their last hospitalization and with left ventricular ejection fraction (LVEF) ≤ 0.35. Patients who had received an implanted cardioverter defibrillator (ICD) at least 3 months prior to admission to study, whether in combination with cardiac resynchronization therapy (CRT-D), were also included.
Conversely, refractory HF, impaired glomerular filtration rate (< 60 mL/min), severe hepatic dysfunction, sustained hypotension, permanent atrial fibrillation, aortic or mitral stenosis, history of angioedema, hospitalization within the last 3 months due to destabilization, acute coronary syndrome and recent surgery were exclusion criteria.
According to the Italian Heath Care Regulatory System, the ARNI administration was authorized after 6-month treatment with ACE inhibitor or angiotensin-receptor blocker (ARB). Sacubitril-valsartan was given on top of optimal medical therapy (OMT) at the starting dose of 50 (24/26) mg twice a day (bis in die, BID), in an open-label fashion. According to 2017 guidelines [10], uptitration to 100 (49/51) mg and 200 (97/103) mg BID was established within the first 2-month period, upon clinical condition, drug tolerance, home-reported blood pressure (BP), renal function and kaliemia. Patient had to accomplish at least 10-month follow-up treatment. The observation period ended July 2020. The median medication dose was calculated on the annual dose taken by each patient and served for clustering the low-mid- (group A) and mid-high-dose (group B) recipients.
Physical examination, quality of life (QoL) assessment by Kansas City Cardiomyopathy Questionnaire (KCCQ) [11], 12-lead ECG, transthoracic echocardiography, 6-min walk test (6MWT), ICD check and laboratory samples were scheduled every 3 months. Changes in NT-proBNP levels and estimated glomerular filtration rate (eGFR) from serum creatinine (Cockroft-Gault equation) were monitored all through the study length. The protocol was conducted according to the Helsinky declarations and international guidelines, so it was just approved by the local advisory boards, with no trial number registration required.
All patients gave informed consent.
Six-minute walk test
An indoor 6MWT was performed along a flat straight corridor with a hard surface. The walking course was 30 m in length, with turnaround points safely marked. Patients were asked to walk as fast as possible with no restriction in resting for a while, if necessary. Heart rate (HR) and symptoms were monitored during the walk. Absolute and predicted walk distance (WD), and walk speed, were calculated in everyone. Predicted WD was calculated according to individual characteristics (weight, height and age), as follows [12, 13]:
-
Men: [(7.57 × height in cm) − (5.02 × age) − (1.76 × weight in kg) − 309 m]
-
Women: [(2.11 × height in cm) − (2.29 × weight in kg) − (5.78 × age) + 667 m]
Echocardiography
Colour Doppler ultrasound examination with standard measurements was performed in each participant. Examiners were blinded on previous achievements from the patient file. Studies were stored in Digital Imaging and Communications in Medicine (DICOM) format and then analysed offline. Left ventricular end-diastolic/end-systolic volumes and LVEF were calculated using the modified biplane (4- and 2-chamber apical views) Simpson rule method [14].
In 77/90 patients (85.5%), LV diastolic function was assessed by mitral valve early Doppler velocity (E)/early tissue velocity (E′) ratio (normal value < 12) and global longitudinal strain (GLS) deformation (normal value: lower than −18%) was measured from the 4-, 3- and 2-chamber apical views.
Statistical methods
Continuous variables are expressed as mean ± SD and categorical variables as numbers and percent (%). Paired data analysis of clinical (NYHA and KCCQ score) and functional (6MWT distance, BNP, NT-proBNP) markers was performed at 3-, 6- and 12-month time follow-ups vs the previous timeline step by using the Pearson model with an alpha level of 0.01 for statistical consistency. Moreover, analysis of variance by ANOVA with Levene’s and Tukey’s correction was performed to establish the between-group homogeneity. Interobserver variability for echocardiographic measurements was calculated in each laboratory as by 0.052 (95% CI 0.034–0.063). The null hypothesis was rejected at two-tailed p < 0.01.
Results
A total of 90 HFrEF patients, mean age 64.5 ± 10.9 years, 74 males (82%), predominantly of an ischaemic aetiology (72%), were enrolled from an initial study population of 96 patients. Of these, 6 were excluded due to ARNI intolerance in 3, allergic reaction in one and non-cardiac hospitalization (COVID-19) in another 2 cases. Demographic and clinical characteristics are summarized in Table 1. Forty-six patients (51%) had received an ICD, and 17 (19%) CRT-D.
The study duration was 12 months (range 11–13) in length, and nobody was lost to follow-up. According to the median cumulative dose of the ARNI (75 mg BID), 52 patients (58%) entered group A (≤ 75 mg) and 38 (42%) group B (> 75 mg).
Most patients gradually required a less amount of loop diuretics on follow-up (online Table 2). Systolic BP was mildly higher in patients from group B, on both admission and follow-up, and this allowed keeping a greater dose of medication.
A clinical improvement was observed in most patients from both groups, according to their QoL. No relevant side effects or adverse events were observed. Renal function (eGFR) showed just a trivial decline in both medication groups.
Regarding exercise tolerance, mildly greater WD and walk speed were observed in group B, especially after the first 6-month treatment (Fig. 1). This difference, however, become trivial as normalized for sex and weight. The proportion of patients walking > 350 m increased from 21 to 58% in group A (p < 0.001), and from 29 to 82% in group B (p < 0.001).
Clinical condition improved according to a lessening in NT-proBNP levels, quicker in group B. Left ventricular volumes decreased in all patients, with a mild improvement in the stroke volume and LVEF (3 points % in group A, 5 points % in group B, p = NS). A positive effect was also seen in the E/E′ ratio and GLS (online Table 3; Fig. 2).
Overtime changes in left ventricular (LV) volumes, ejection fraction (LVEF) and global longitudinal strain (GLS) at transthoracic echocardiography. LVEDVi, left ventricular end-diastolic volume index; LVESVi, left ventricular end-systolic volume index; NT-proBNP, N-terminal pro B–type natriuretic peptide. LVEF value is percent (%). *p < 0.001
Discussion
Twelve-month ARNI therapy was clinically advantageous in our HFrEF outpatient population. We analysed the impact of different cumulative ARNI dosage on clinical status, physical performance, QoL and echocardiographic parameters. After switching to ARNI, both groups moved towards better clinical conditions. Also, reverse LV remodelling and slight systo-diastolic functional amelioration were observed according to a gradual decrease in circulating NT-proBNP levels. Overall, patients from group B attained greater and quicker clinical achievements, which were however satisfactory even in group A at the end of follow-up. Such improvements may be consistent with a positive impact on the progression and prognosis of HFrEF in the real-life patient population.
Despite the proportion of high-dose ARNI recipients in large pivotal trials, the adherence to multidrug therapy remains a challenging item in clinical practice, even if adults with cardiovascular diseases are prone to polypharmacy due to comorbidities and complexity of medication regimens [15, 16]. Though we have already observed drug-related benefit in patients at a high risk of arrhythmic disorders, high-dose ARNI therapy has some practical limitations, especially in patients with low BP symptoms [17, 18]. In fact, despite suitable clinical characteristics, Martens et al. demonstrated that high doses were administered only to 32% of HFrEF patients [19].
Unfortunately, the PARADIGM-HF study showed that patients scheduled to a dose reduction were at a higher risk of major cardiovascular events [5, 9]. Nevertheless, Vardeny et al. reported a reduced risk of death and HF hospitalization even by taking lower ARNI doses, compared to ACE inhibitors [20]. A recent meta-analysis confirmed the dose of 200 mg BID to be possible in 35% of European patients, with a potential of discontinuation in 12.8% of cases [21]. These findings likely support the fact that real-life patients are different from pivotal studies, and encourage clinicians to search for OMT without extremes.
In our study, exercise performance improved in both groups, and this is an important therapeutic target. The proportion of patients walking > 350 m at the end of study was greater in group B (82%) than in group A (58%), but we also demonstrated that confounders like weight, body mass, sex and physical inactivity can affect their performance.
The interplay between clinical and functional achievements and NT-proBNP levels in this study confirmed previously published data by Pandey et al. who found that even lower than standard doses of ARNI were able to reduce the circulating NT-proBNP and loop diuretic requirement, without any relevant change in potassium or serum creatinine [22]. Though the dose of 50 mg BID has been considered the lowest ARNI dose to be given to HFrEF patients, clinical advantages have also been shown with very low-doses (12/13 mg BID) [23].
Regarding LV function by echocardiography, drug-related reverse remodelling likely remains a controversial issue. In previous studies, ARNI was effective when initiated early after diagnosis, and at least for 3 months [24,25,26]. Though most patients in our series have gotten a decrease in cardiac chamber volumes, chiefly related to a reduced end-systolic volume, case-by-case and interobserver variability represent important shortcomings for a correct interpretation of these findings. The weak improvement in LVEF (4 points %) in our patients, a bit more relevant in group B, confirmed the results of Almufleh et al. who reported + 5% LVEF in high-dose vs + 4% in low-dose recipients [26]. Conversely, we did not see the complete functional recovery found in 17% of non-ischaemic HF patients by Chang et al. [27].
Tissue Doppler and strain imaging could be the way to overcome the limitation of LVEF variability. Improved GLS and LV diastolic function was recognized in our subset of 77 patients, though their absolute values remained quite low. Strain echocardiography likely represents an interesting imaging modality to explore myocardial impairment in HF patients as consequence of tissue oedema, inflammation and fibrosis [28], which can be counterbalanced by ARNI treatment [29, 30].
Limitations
The small sample size is the main limitation of the present study. Our patients, however, were strongly asked to follow the whole scheduled observational period, and this allowed the study completion at 1-year follow-up. Findings from the study population were not compared to controls, and this may have affected the true assessment of clinical outcomes. However, the aim of the study was not to establish the ARNI effectiveness vs conventional therapy, but dose-related discrepancies, if any. Though no serious outcomes occurred in our study population, informative findings on subclinical events, like intercurrent atrial fibrillation or ventricular arrhythmias, are missing except for the ICD-monitored patients. Echocardiography examination was only partially blinded, and the examiner could retain therapeutic information by the patient. Prospective longitudinal studies with a central echo data reading should be encouraged to avoid any interference in data analysis. Further functional information might have been achieved by cardiopulmonary exercise testing, which remains the gold standard for functional assessment of HF patients.
Though the prevalence of type 2 diabetes was not so high in our study population, metabolic parameters interact with the cardiomyocyte function and lead to increased inflammation, apoptosis, reactive oxygen species and altered calcium signalling [31]. Diabetes cardiomyopathy likely impairs prognosis and deserves more awareness in HF populations, also in view of the most recent studies on SGLT2 inhibitors in both diabetic and non-diabetic patients [32].
Current literature also suggests early initiation of the ARNI (50 mg BID) as an effective, risk-free, therapeutic approach that increases quality-adjusted life expectancy and cost savings compared with no initiation or initiation late after hospitalization [33, 34].
Conclusion
One-year sacubitril/valsartan treatment on top of OMT was advantageous in our real-like HFrEF patient population. Beneficial effects on clinical condition, QoL, exercise performance, LV remodelling and function were observed in both study groups, though slightly greater and with a shorter time to benefit in patients from group B.
Availability of data and material
Upon request.
References
Cook C, Cole G, Asaria P, Jabbour R, Francis DP (2014) The annual global economic burden of heart failure. Int J Cardiol 171:368–376
Camplain R, Kucharska-Newton A, Keyserling TC, Layton JB, Loehr L, Heiss G (2018) Incidence of heart failure observed in emergency departments, ambulatory clinics, and hospitals. Am J Cardiol 11:1328–1335
Khan SS, Ning H, Shah SJ, Yancy CW, Carnethon M, Berry JD et al (2019) 10-year risk equations for incident heart failure in the general population. J Am Coll Cardiol 73:2388–2397
Ziaeiana B, Fonarowc GC (2016) The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis 58:379–385
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR et al (2014) PARADIGM-HF investigators and committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371:993–1004
Arrigo M, Vodovar N, Nougué H, Sadoune M, Pemberton CJ, Ballan P et al (2018) The heart regulates the endocrine response to heart failure: cardiac contribution to circulating neprilysin. Eur Heart J 39:1794–1798
Moliner-Abós C, Rivas-Lasarte M, Pamies Besora J, Fluvià-Brugues P, Solé-González E, Mirabet S et al (2019) Sacubitril/valsartan in real-life practice: experience in patients with advanced heart failure and systematic review. Cardiovasc Drugs Ther 33:307–314
Morrow DA, Velazquez EJ, DeVore AD, Desai AS, Duffy CI, Ambrosy AP et al (2019) Clinical outcomes in patients with acute decompensated heart failure randomly assigned to sacubitril/valsartan or enalapril in the PIONEER-HF trial. Circulation 139:2285–2288
Senni S, McMurray JJV, Wachter R, McIntyre HF, Reyes A, Majercak I, Andreka P et al (2018) Initiating sacubitril/valsartan (LCZ696) in heart failure: results of TITRATION, a double-blind, randomized comparison of two uptitration regimens. Eur J Heart Fail 18:1193–1202
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM et al (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 136:e137–e161
Yee D, Novak E, Platts A, Nassif ME, LaRue SJ, Vader JM (2019) Comparison of the Kansas City Cardiomyopathy Questionnaire and Minnesota Living with Heart Failure Questionnaire in predicting heart failure outcomes. Am J Cardiol 123:807–812
Enright PL, Sherrill DL (1998) Reference equations for the six minute walk in healthy adults. Am J Respir Crit Care Med 158:1384–1387
ATS Committee on proficiency standards for clinical pulmonary function laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–7
Wahr DW, Wang YS, Schiller NB (1983) Left ventricular volumes determined by two-dimensional echocardiography in a normal adult population. J Am Coll Cardiol 1:863–868
Blood AJ, Fraiche AM, Eapen ZJ (2017) Is an admission for decompensated heart failure inevitable? Prog Cardiovasc Dis 60:171–177
Iorio A, Senni M, Barbati G, Greene SJ, Poli S, Zambon E et al (2018) Prevalence and prognostic impact of non-cardiac co-morbidities in heart failure outpatients with preserved and reduced ejection fraction: a community-based study. Eur J Heart Fail 20:1257–1266
Corrado E, Saladino A, Morgante G, Mignano A, Nugara C, Novo G et al (2020) Reverse remodeling and arrhythmic burden reduction in a patient with an implantable cardioverter defibrillator treated with sacubitril/valsartan: case report. Clin Case Rep 8:1349–1352
Casale M, Correale M, Laterra G, Vaccaro V, Morabito C, Crea P et al (2021) Effects of sacubitril/valsartan in patients with high arrhythmic risk and an ICD: a longitudinal study. Clin Drug Investig 41:169–176
Martens P, Verluyten L, Van de Broek H, Somers F, Dauw J, Dupont M et al (2019) Determinants of maximal dose titration of sacubitril/valsartan in clinical practice. Acta Cardiol 7:1–10
Vardeny O, Claggett B, Packer M, Zile MR, Rouleau J, Swedberg K et al (2016) Prospective comparison of ARNI with ACEi to determine impact on global mortality and morbidity in heart failure (PARADIGM-HF) investigators. Efficacy of sacubitril/valsartan vs. enalapril at lower than target doses in heart failure with reduced ejection fraction: the PARADIGM-HF trial. Eur J Heart Fail 18:1228–34
Giovinazzo S, Carmisciano L, Toma M, Benenati S, Tomasoni D, Sormani MP et al (2021) Sacubitril/valsartan in real-life European patients with heart failure and reduced ejection fraction: a systematic review and meta-analysis. ESC Heart Fail. https://doi.org/10.1002/ehf2.13547 (in press)
Pandey AC, Jer D, Kuo RS, Yoo DH, Christophy A, Mohan RC et al (2021) Novel doses of sacubitril/valsartan in patients unable to tolerate traditional therapy: effects on N-terminal pro B-type natriuretic peptide levels. Clin Cardiol 44:85–90
Hu J, Wu Y, Zhou X, Wang X, Jiang W, Huo J et al (2020) Beneficial effects of sacubitril/valsartan at low doses in an Asian real-world heart failure population. J Cardiovasc Pharmacol 76:445–451
Wang Y, Zhou R, Lu C, Chen Q, Xu T, Li D (2019) Effects of the angiotensin-receptor neprilysin inhibitor on cardiac reverse remodeling: meta-analysis. J Am Heart Assoc 8:e012272
de Gregorio C, Laterra G, Vaccaro V, Bitto R, Dattilo G (2020) Time-based clinical and functional achievements in real-life HF patients on ARNI treatment. Eur J Intern Med 76:115–117
Almufleh A, Marbach J, Chih S, Stadnick E, Davies R, Liu P et al (2017) Ejection fraction improvement and reverse remodeling achieved with Sacubitril/Valsartan in heart failure with reduced ejection fraction patients. Am J Cardiovasc Dis 7:108–113
Chang HY, Chen KC, Fong MC, Feng AN, Fu HN, Huang KC et al (2020) Recovery of left ventricular dysfunction after sacubitril/valsartan: predictors and management. J Cardiol 75:233–241
Mazzetti S, Scifo C, Abete R, Margonato D, Chioffi M, Rossi J et al (2020) Short-term echocardiographic evaluation by global longitudinal strain in patients with heart failure treated with sacubitril/valsartan. ESC Heart Fail 7(3):964–972
Nougué H, Pezel T, Picard F, Sadoune M, Arrigo M, Beauvais F et al (2019) Effects of sacubitril/valsartan on neprilysin targets and the metabolism of natriuretic peptides in chronic heart failure: a mechanistic clinical study. Eur J Heart Fail 21:598–605
Januzzi JL, Butler J, Fombu E, Maisel A, McCague K, Piña IL et al (2018) Rationale and methods of the Prospective Study of Biomarkers, Symptom Improvement, and Ventricular Remodeling During Sacubitril/Valsartan Therapy for Heart Failure (PROVE-HF). Am Heart J 199:130–136
Dannenberg L, Weske S, Kelm M, Levkau B, Polzin A (2021) Cellular mechanisms and recommended drug-based therapeutic options in diabetic cardiomyopathy. Pharmacol Ther 228:107920
Dewan P, Solomon SD, Jhund PS, Inzucchi SE, Køber L, Kosiborod MN et al (2020) Efficacy and safety of sodium-glucose co-transporter 2 inhibition according to left ventricular ejection fraction in DAPA-HF. Eur J Heart Fail 22(7):1247–1258
Acanfora D, Scicchitano P, Acanfora C, Maestri R, Goglia F, Incalzi RA et al (2020) Early initiation of sacubitril/valsartan in patients with chronic heart failure after acute decompensation: a case series analysis. Clin Drug Investig 40:493–501
Gaziano TA, Fonarow GC, Velazquez EJ, Morrow DA, Braunwald E, Solomon SD (2020) Cost-effectiveness of sacubitril-valsartan in hospitalized patients who have heart failure with reduced ejection fraction. JAMA Cardiol 5:1236–1244
Author information
Authors and Affiliations
Contributions
EC, GD, GC, CM, EB, LZ, GN and CDG were involved in the clinical management, ultrasound imaging and treatment of the patients. EC revised the manuscript. CDG drafted, revised and upgraded the manuscript; interpreted the patient data; and performed statistical analysis; LZ was also involved in the literature search. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Human and animal rights
Research involved human participants, following current international criteria for treating HF.
Informed consent
Informed consent was given by each participant for clinical management and ultrasound imaging.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Corrado, E., Dattilo, G., Coppola, G. et al. Low- vs high-dose ARNI effects on clinical status, exercise performance and cardiac function in real-life HFrEF patients. Eur J Clin Pharmacol 78, 19–25 (2022). https://doi.org/10.1007/s00228-021-03210-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03210-0