Abstract
Summary
Number and age-standardized incidences of femoral fractures by sex and localization were determined annually between 1998 and 2021 in subjects aged 45 years or older living in Switzerland. The number and incidences of femoral neck, pertrochanteric, subtrochanteric, and femoral shaft fractures followed distinct unexpected trend patterns.
Introduction
Long-term incidence trends for femoral fractures by individual localizations are unknown.
Methods
Annual absolute number of hospitalizations and median age at hospital admission between 1998 and 2021 were extracted from the medical database of the Swiss Federal Office of Statistics by sex and 10-year age groups for the following 10th International Classification of Diseases (ICD-10) codes: femoral neck (ICD-10 S72.0), pertrochanteric (S72.1), subtrochanteric (S72.2), and femoral shaft fractures (S72.3). Age-standardized incidence rates (ASI) and corresponding trends were calculated.
Results
Over 24 years, the number of femoral neck fractures increased in men (+ 45%) but decreased in women (− 7%) with ASI significantly decreasing by 20% and 37% (p < 0.001 for trend for both), respectively. By contrast, the number of pertrochanteric fractures increased by 67% and 45% in men and women, respectively, corresponding to a horizontal ASI-trend in men (n.s.) and a modest significant decreasing ASI-trend in women (p < 0.001). The number of subtrochanteric fractures increased in both sexes with corresponding modest significant reductions in ASI-trends (p = 0.015 and 0.002, respectively). Femoral shaft fractures almost doubled in men (+ 71%) and doubled in women (+ 100%) with corresponding significant increases in ASI-trends (p = 0.001 and p < 0.001, respectively). Age at admission increased for all fracture localizations, more so in men than in women and more so for subtrochanteric and shaft fractures than for “typical” hip fractures.
Conclusion
Incidence changes of pertrochanteric fractures and femoral shaft fractures deserve increased attention, especially in men. Pooling diagnostic codes for defining hip fractures may hide differing patterns by localization and sex.
Similar content being viewed by others
Introduction
Osteoporosis is a systemic skeletal disease characterized by low bone mass and bone microarchitecture decay resulting in increased bone fragility and fracture risk [1]. A patient with osteoporosis may experience a fracture of any bone but is particularly exposed to an increased risk of fracture after a low-energy trauma, whereby the latter increases with increasing age [2]. Hip fractures, usually including femoral neck and pertrochanteric fractures, represent the most typical and at the same time the most severe complications of osteoporosis, usually leading to immediate functional impairment with subsequent hospitalization for orthopedic repair in almost all cases, as well as long-term disability and increased mortality [3, 4]. Other femoral fractures such as subtrochanteric and shaft fractures are also more frequent in patients with osteoporosis, whereby fractures of the femoral diaphysis more typically follow a high-intensity trauma. When occurring after a low-energy trauma and in accordance with a defined set of diagnostic criteria, which also includes radiological considerations, subtrochanteric and shaft fractures may correspond to an atypical femoral fracture (AFF) [5, 6]. Atypical femoral fractures have been reported in patients taking antiresorptive drugs (such as bisphosphonates and denosumab), but they also occur in patients with no exposure to these drugs [5, 7].
Osteoporosis remains an underdiagnosed and undertreated disease in women but even more so in men [8, 9]. However, a reversal of the secular trend for hip fractures was reported as early as in 1987 in the USA [10], later confirmed in Switzerland, first in women [11, 12], and thereafter in both men and women [13]. In a recent publication on the global epidemiology of hip fractures, a negative trend was shown in some industrialized countries, including USA, UK, Spain, and Italy, but an increasing trend in other (France, Germany) [14]. In none of these publications, subanalyses by femoral fracture localization were made available. Whether one or another fracture type has contributed more than others to the aggregated results for hip fractures remains unknown.
In Switzerland, life expectancy is among the highest worldwide, possibly still second after Japan [15]. Between 1998 and 2021, life expectancy at birth increased from 76.3 to 81.6 years in men (+ 5.3 years) and from 82.5 to 85.7 years in women (+ 3.2 years) [16]. Thus, the population living in Switzerland is old and ageing, even more rapidly so for men than women. The latter may be, at least in part, related to a larger decrease in cardiovascular mortality in men than in women, a general epidemiological observation made in the developed world. For example, in Switzerland, mortality due to coronary heart disease was approximately halved in men and women between 1995 and 2018, with men remaining at twice as high risk than women [17]. Considering that coronary heart disease is the leading cause of death in men and usually occurs at earlier ages than hip fractures, numerically, more men than women will enter age groups at increased risk for femoral fractures. Epidemiological observations on fractures made in such an old mainly Caucasian population may represent a paradigm for the near or midterm future of other industrialized Western countries.
In this context, the aim of the present analyses was to document the epidemiological trends of femoral fractures by localization, in men and women living in Switzerland and aged 45 years or older, in terms of number, incidence, and changes in age at admission between 1998 and 2021. The findings could be of major importance for health care planning policy.
Methods
Data source
Raw data were extracted from the administrative and medical statistics database of the Swiss Federal Statistical Office of Statistics (SFSO). Since 2010, all Swiss hospitals (100.0%) are bound to report to the SFSO an administrative and medical core dataset for each hospitalized patient. Representativeness was 62.2% in 1998 and has increased steadily since then, exceeding 98% as of year 2005 and reaching 100% in year 2010. Of note, as of 1998, the hospital statistics were representative of the country as a whole, legitimating linear extrapolations. The stringent quality control measures include plausibility testing of all records by a SFSO proprietary software (MedPlaus version 6.0) which runs more than 700 plausibility checks for each case, including with regard to coding for diseases according to the International Classification of Diseases (ICD-10) [18]. In addition, before consolidation at the federal level, yearly validation of diagnostic coding at individual hospital level is mandatory since 1998, and consistency in reporting across cantons is ensured by the SFSO. The SFSO also publishes the structure of the population living in Switzerland by sex and 5-year age groups on an annual basis.
Dataset
For men and women aged 45 years or older, all cases of femoral fractures having led to an acute hospitalization between year 1998 and 2021 (24 years) were extracted and included in the primary analysis. Only femoral fractures coded as the main reason for hospitalization (primary diagnosis) were considered; fractures listed as co-diagnoses (secondary diagnoses) were excluded. Hospitalizations in rehabilitation clinics and rehospitalizations for the same fracture occurring within 2 months after the index event were excluded to prevent double counting, according to SFSO recommendations.
Femoral fractures (ICD-10 code S72) were identified by using the following: fractures of femoral neck including not otherwise specified fractures of the hip (S72.0), pertrochanteric fractures including intertrochanteric and trochanteric fractures (S72.1), subtrochanteric fractures (S72.2), fractures of the femoral shaft (S72.3). In a second step, for the purpose of this analysis and for didactical reasons, femoral neck and pertrochanteric fractures were pooled under the header “typical” osteoporotic femoral fractures (S72.0 + S72.1) while subtrochanteric and shaft fractures were defined as “non-typical” osteoporotic fractures (S72.2 + S72.3). The remaining four subordinate ICD-10 codes (fractures of the distal femur (S72.4), multiple fractures of the femur (S72.7), fractures of other parts of the femur (S72.8), and fractures of an unspecified part of the femur (S72.9)) represented less than 10% of all reported cases and were excluded from the present analysis. For each individual patient included in the database, age at admission was also extracted. The age structure of the male and female population living in Switzerland by 10-year age groups was obtained directly from the SFSO for years 1998 through 2021.
Data processing
The annual absolute number of hospitalized femoral fractures was extracted from age 45 onwards by sex and 10-year age groups for years 1998 to 2021. Where appropriate (i.e., before year 2010), the absolute number of cases was extrapolated linearly to 100% to adjust for non-participating hospitals. Crude incidence rates by sex, expressed as the number of cases per 100,000 person-years, were calculated by 10-year age groups and in all patients aged 45 years or older for each fracture category. Age-standardized incidences with corresponding 95% confidence intervals were calculated by sex and fracture localization using the 1998 population structure as a reference, following the methodology first suggested by Lewinnek [19]. For a given year, the age-standardized incidence rate is the summary rate that would be observed, given the single age-specific rates in that year, in a population with the age composition of the reference population. Thus, age-standardization allows for direct comparisons across populations with different age structures. Time trends were explored by simple regression analyses (a positive r value indicating a positive trend and conversely for a negative r value, with a two-sided p < 0.05 considered significant) and based on the average annual percent change (AAPC) with corresponding 95% confidence intervals (95%CI), whereby an interval not including zero stands for statistical significance, consistent with the methodology detailed in [20]. For men and women aged 45 years or older, median age at hospital admission with corresponding lower and upper quartiles (interquartile range, IQR) was calculated by sex and year for each femoral fracture category. All calculations were performed using the StatsDirect statistical software, version 3.3.5, developed by Statsdirect Ltd, Birkenhead, Merseyside, UK.
Results
During the 24-year observation period covered by the present analysis, the male population aged 45 years or older increased by 52% with largest percent increases in the oldest age groups, reaching + 116% in the oldest old (aged 85 years or older). The corresponding female population increased by 40%, reaching + 56% in the oldest old (Fig. 1).
With detailed numbers for years 1998 and 2021 available in supplemental Table 1 and annual numbers shown in Figs. 2a and 3a, the number of fractures increased in all four fracture categories retained for analysis in both sexes between 1998 and 2021, except the number of femoral neck fractures in women which decreased by 7%. In men, the ratio of femoral neck fractures to pertrochanteric fractures decreased from 1.3 in 1998 to 1.1 in 2021 with corresponding ratios for women of 1.4 and 1.0, respectively.
Femoral neck and pertrochanteric fractures (ICD-10 S72.0 and S72.1, respectively) in men (left) and women (right)—absolute number of cases (a), crude incidence per 100,000 person-years (b), age-standardized incidence per 100,000 person-years (c). r and two-sided p values for trend between 1998 and 2021
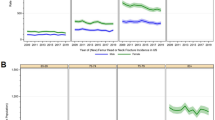
Subtrochanteric and femoral shaft fractures (ICD-10 S72.2 and S72.3, respectively) in men (left) and women (right)—absolute number of cases (a), crude incidence per 100,000 person-years (b), age-standardized incidence per 100,000 person-years (c). r and two-sided p values for trend between 1998 and 2021
Femoral neck fractures (ICD-10 S72.0)
The total number of acute hospitalizations (cases) for a femoral neck fracture increased by 45% in 24 years. The crude incidence decreased modestly from 102 to 97 per 100,000 male-years, following a statistically significant almost linear negative trend (r and two-sided p value for trend shown in Fig. 2b). The latter significant trend was observed in all 10-year age groups except in those aged 55–64. The age-standardized incidence (95%CI) in men decreased significantly by 20% from 102 (96–107) to 82 (78–85) per 100,000 male-years between 1998 and 2021 (Table 1, with r and two-sided p value for trend shown in Fig. 2c), corresponding to an average annual percent change (AAPC) of − 1.71% (95%CI − 3.43 to − 0.01). Median (IQR) age at admission increased by two years in men, from 78 years (67–86) in 1998 to 80 years (70–87) in 2021.
By contrast and as shown in Fig. 2a–c, the number of femoral neck fractures decreased by 7% in women in 24 years, with a corresponding decrease in the crude incidence from 272 to 180 per 100,000 female-years. The latter negative trend was statistically significant in all 10-year age groups. As shown in Table 1, the age-standardized incidence (95%CI) decreased significantly by 37% from 272 (264–281) to 171 (165–176). The corresponding AAPC (95%CI) was − 2.41% (− 4.30 to − 0.52). Median (IQR) age at admission increased by only 1 year in women, from 82 years (75–87) in 1998 to 83 (76–89) in year 2021.
Pertrochanteric fractures (ICD-10 S72.1)
Between 1998 and 2021, the number of pertrochanteric fractures in men increased by 67%. The crude incidence increased from 78 to 86 per 100,000 male-years following an overall statistically significant trend (Fig. 2b). This overall trend reflected a composite of a significantly decreasing trend in younger age groups (45–64) overwhelmed by an increasing trend in all age groups above 65. As shown in Table 1, the age-standardized incidence (95%CI) went from 78 (73–83) to 71 (68–74) following a non-significant horizontal trend over 24 years (Fig. 2c) with a non-significant APCC of − 0.48% (95%CI − 2.38 to 1.42). Median (IQR) age at admission increased by 3 years in men, from 77 (64–84) to 80 (70–87).
In women aged 45 years or older, the total number of acute hospitalizations for pertrochanteric fractures increased by 32% in 24 years (Fig. 2a), which contrasts with the numerical decrease observed for femoral neck fractures. Nevertheless, the crude incidence followed a statistically significant negative trend, overall (Fig. 2b), and in all 10-year age groups except the oldest old. As shown in Table 1, the change in age-standardized incidence (IQR) followed a similar pattern with a reduction from 194 (187–201) to 172 (166–177) per 100,000 female-years (Fig. 2c) corresponding to an AAPC of − 1.09% (95%CI − 3.44 to 1.27). Median (IQR) age at admission increased by only 1 year in women, from 84 (78–88) years in 1998 to 85 (79–90) in year 2021.
“Typical” osteoporotic fractures (ICD-10 S72.0 + S72.1)
From the above, it becomes clear that trend changes to be expected for typical osteoporotic fractures will result from merged trends at the level of the individual fracture localizations. In men aged 45 years or older, this age-standardized incidence (95%CI) per 100,000 male-years decreased from 179 (172–187) to 153 (148–158) between 1998 and 2021, corresponding to a significant negative trend over 24 years (r = − 0.83, two-sided p < 0.001; AAPC − 0.81% with 95%CI − 2.21 to 0.59). The latter was the combined result of a decreasing trend in femoral neck fractures (consistent with a reversal of the secular trend) and a non-significant horizontal trend for pertrochanteric fractures. In women, the age-standardized incidence for typical osteoporotic fractures went from 466 (455–477) to 342 (335–350) with r = − 0.94, p < 0.001 and AAPC − 1.73% with 95%CI − 3.58 to 0.13, reflecting a significantly decreasing incidence of femoral neck but not pertrochanteric fractures. Median age at admission increased by 2 to 3 years in men and by 1 year only in women for both fractures, which is consistent with the more rapid ageing of the male population (Fig. 1). Of note, and as evidenced in Fig. 2b, c, the interval between the incidence curves of femoral neck and pertrochanteric fractures narrowed over time. While both curves remained distinct in men, with femoral neck fractures remaining the most frequent, they became overlapping in women as of year 2010, with both fractures occurring at almost identical incidences since then.
Subtrochanteric fractures (ICD-10 S72.2)
In men aged 45 years or older, the annual number of subtrochanteric fractures increased by 52% between 1998 and 2021 (Fig. 3a). The overall crude incidence remained unchanged at 11 per 100,000 male-years (Fig. 3b) with non-significant trends being observed in all age groups. After age-standardization (Table 1), a modest but significant negative trend in incidence was observed (Fig. 3c). The average annual percent change in age-standardized incidence was − 0.32% (95%CI − 4.69 to 4.05). Median (IQR) age increased by 8 years, from 70 (57–82) to 78 (65–85).
In women (Fig. 3a–c), the number of subtrochanteric fractures increased by only 9% during the 24 years of observation. By contrast, the crude incidence decreased from 27 to 21 per 100,000 female-years corresponding to a statistically significant negative trend in women aged 45 years or older, seen at all ages but reaching statistical significance in the age group 75–84 only. Age-standardization further confirmed this negative trend Table 1. The overall AAPC was not significant: − 0.62% (95%CI − 4.51 to 3.28). Median (IQR) age at admission went from 82 (75–87) to 85 (77–89), an increase by 3 years.
Femoral shaft fractures (ICD-10 S72.3)
As shown in Fig. 3a–c and Table 1, the number of acute hospitalizations for femoral shaft fractures increased by 71% in men, corresponding to a significantly increasing trend in the crude incidence per 100,000 male-years from 15 in year 1998 to 17 in year 2021. This trend reached statistical significance in all 10-year groups beyond age 65. The age-standardized incidence was identical in years 1998 and 2021 with a remarkable biphasic aspect of the incidence curves unveiling a decrease between 1998 and 2005 followed by a marked increase between 2006 and 2021 leading to an overall significantly increasing trend over 24 years. However, when estimated by the AAPC and owe to the low number of cases, this overall trend was no more significant (+ 0.52% per year with 95%CI − 3.70 to 4.08). In men aged 45 years or older, median (IQR) age at admission was 71 (57–78) in year 1998 and 78 (66–86) in year 2021, an increase by 7 years.
In women (Fig. 3a–c; Table 1), the number of femoral shaft fractures doubled over 24 years. The crude incidence followed an increasing significant trend from 25 to 36 per 100,000 female-years with significant positive trends seen in all age groups beyond 65 years of age. The corresponding numbers (95%CI) for age-standardized incidence in women aged 45 years or older were 25 (23–28) and 34 (31–36), respectively. The AAPC for the age-standardized incidence was 1.34% (95%CI − 3.39 to 6.07). Median (IQR) age at admission went from 80 (71–86) to 85 (77–90), an increase by 5 years.
“Non-typical” osteoporotic fractures (ICD-10 S72.2 + S72.3)
In line with the above, the age-standardized incidence of non-typical osteoporotic fractures showed a significant positive trend in both men and women aged 45 years or older (r = 0.42, two-sided p = 0.042 and r = 0.60, p = 0.002, respectively) but not when estimated based on the average annual percent changes (95%CI) of + 0.19% (− 3.70 to 4.08) and + 0.49 (− 1.36 to 2.35) for men and women, respectively. This merged trend was the result of a decrease in subtrochanteric fractures combined with an increase in femoral shaft fractures observed in both sexes. The latter was driven by incidence increases in all age groups beyond 65 years of age for both sexes but more pronounced in women.
Discussion
Over the 24-year observation period (1998–2021) covered in the present analysis, femoral fractures were numerically increasing, especially in men, and followed epidemiological patterns differing by fracture localization, sex, age groups, and age at admission for acute hospitalization. The incidence of typical osteoporotic femoral fractures, also referred to as hip fractures, was decreasing in both men and women living in Switzerland. However, the analysis by fracture localization unveiled that this decrease in hip fracture incidence, also referred to as a reversal of the secular trend, was mainly driven by a reduction in femoral neck fracture incidence while, in contrast, the incidence of pertrochanteric fractures remained either unchanged (in men) or decreased only slightly (in women). The incidence of subtrochanteric fractures decreased slightly in both sexes, but the incidence of femoral shaft fractures markedly increased, even more so in women than in men. Overall, median age at admission increased for all fractures but more so in men than women, consistent with the faster ageing of the male population aged 45 years or older.
Hip fractures, a typical and severe complication of underlying osteoporosis in both men and women, involve the proximal part of the femur and usually include fractures of the femoral neck and pertrochanteric fractures [11, 12], but may also include subtrochanteric fractures [9, 13, 21]. In a recent analysis covering years 1998 through 2018, the number of hip fractures (including subtrochanteric fractures) was shown to have increased by 42% and 11% in men and women aged 45 years or older, respectively, with decreasing age-standardized incidences in both (− 15% and − 22%, respectively) [13]. The latter has also been referred to as a reversal of a secular trend, first reported by Melton et al. in their seminal work in Rochester, Minnesota [10]. In Switzerland, such a reversal of the secular trend in hip fracture incidence was first shown in the female population of Geneva, but not in males, in a prospective study covering 10 years (1991 to 2000) with a sample size of approximately one-twentieth of the one used for the present analysis [11, 12]. While pooling fractures under the header of hip fractures does have its merits, including simplified analysis and reporting, it may dissimulate more discrete changes of clinical relevance occurring at the individual fracture localization level.
The statistically significant decreasing trend in hip fracture incidence observed in both sexes over the past 24 years covers in fact a marked decrease in femoral neck fractures, more so in women than in men, and much smaller (women) or even inexistent (men) decrease in pertrochanteric fractures. This suggests that the observed reversal of the secular trend may not occur with the same magnitude at all hip fracture sites and should ultimately, if continuing, lead to a shift from femoral neck fractures to pertrochanteric fractures becoming the predominant fracture localization. This is of concern as pertrochanteric fractures are usually considered as more severe than femoral neck fractures and typically associated with longer hospital stays, higher functional impairment, reduced likeliness of early recovery, and higher mortality [4, 22]. A recent study performed in the Kyoto Prefecture of Japan, which compared two recent 5-year time periods (2008–2012 and 2013–2017) reported that the number of femoral neck and pertrochanteric fractures had increased in all age groups beyond 65 years of age, except for pertrochanteric fractures in 75–84-year-old women. The estimated incidences showed an increase in femoral neck fractures in men aged 75 years or more and in women aged 85 years or more only [23]. The findings in Japan are discrepant with our findings according to which the incidence of femoral neck fractures decreased in all age groups between 1998 and 2021, more so in women than in men. The reasons for these differing observations may be multiple, including the duration of observation (24 vs. 10 years), the population base used for calculating the incidences (full country vs. regional/prefectural population), and Caucasian vs. Japanese hip fracture patients. However, also this study unveiled a difference in epidemiological “behavior” between femoral neck and pertrochanteric fractures deserving more research.
In the present analysis, median age at admission for a femoral fracture increased over time in both sexes, more so in men than in women, but was the same for femoral neck and pertrochanteric fractures in men (80 years in 2021) while women were generally older (83 years for femoral neck and 85 years for pertrochanteric fractures). This is consistent with the observed incidence trends and the faster ageing of the male population but is of further concern as increasing age is associated with more comorbidities and poorer outcomes [22]. On the other hand, osteoporosis treatment is far more frequent in women than in men [24], which would be consistent with the larger magnitude of decrease of the age-standardized hip fracture incidence observed in women. However, no association was found between the change in hip fracture incidence and the treatment rate with antiresorptives at the population level [9]. Furthermore, the proportion of patients at increased risk for fractures treated for osteoporosis remains low leading to a dilution of effect hampering signal detection at the population level [9]. Finally, antiresorptives increase bone mineral density more at the trochanter than at the femoral neck, possibly in relation with the larger amount of trabecular bone at the former, but may decrease the risk of both types of hip fractures by the same order of magnitude [25, 26] although some clinical endpoint trials showed a lower effect with regard to pertrochanteric fracture risk reduction [27, 28]. Thus, at the population level, an effect of treatment would expectedly be seen, if at all, rather in women than in men and with a similar effect size at both fracture localizations. The marked decrease seen in femoral neck fractures in both sexes and the discrepant changes seen with pertrochanteric fractures are not consistent, neither in quantity nor in quality, with a to-be-expected effect of osteoporosis drug therapy at the population level.
A task force of the American Society for Bone and Mineral Research proposed a case definition for atypical femoral fractures (AFF) which included the following major features: a localization in the subtrochanteric region or the femoral shaft, transverse or short oblique orientation, minimal or no associated trauma, a medial spike when the fracture is complete, and absence of comminution [5, 6]. In a population of female patients with osteoporosis included in three fracture endpoint trials, of which 50% were treated with placebo, the overall incidence of AFF was estimated at 23 per 100,000 patient-years (12 AFFs of 283 hip or femoral fractures during 51,287 patient-years) [25]. For the present work, neither radiological nor fall or trauma information was available. Thus, only fracture localization could be used as an indicator for suspicion of an AFF, and the terminology of non-typical femoral fracture was used to prevent any confusion. Subtrochanteric fractures exhibited a flat to slightly decreasing incidence trend. By contrast, femoral shaft fractures showed a marked increase in incidence in men and even more so in women. Considering the low incidence of AFF, the increase in shaft fractures observed in both sexes, although men are undertreated, and following the above argumentation regarding signal detection at the population level, it appears unlikely that the use of antiresorptives may explain an increase of this magnitude. Rather, this increase should be seen in the context of increased physical and injury-prone high-velocity activities at ever older ages. The latter include heavily advertised e-biking but also skiing and mountain-trekking for seniors. Men hospitalized for a femoral shaft fracture in 2021 were 7 years older than in 1998 and women 5 years older. Furthermore, the incidence increase was observed in the 10-year age groups beyond 65 with the largest increases observed in the oldest old. In January 2009, a new tariff-system based on diagnosis-related groups (DRG) was implemented in Switzerland. Briefly, acute hospitalizations became reimbursed by health insurances based on flat rates. Despite quality control measures aimed at preserving longitudinal data consistency, an effect of such an important change on the use of diagnostic codes cannot be excluded. However, femoral shaft fractures started increasing earlier (in 2005 in men and in 2008 in women), and the magnitude of increase renders an intended or unintended pure effect of changes in diagnostic coding highly unlikely.
The present study has strengths and limitations. Among the strengths, the 24 years of observation were derived from the same database, covering more than 95% of all Swiss hospitals since 2002 (100% since 2010), managed with consistent and sustained quality standards over time. Furthermore, only femoral fractures were considered which virtually all end up with an acute hospitalization such that the observed longitudinal trends should be considered reliable. Another key strength is the analysis by fracture localization which unveiled yet unknown and still unexplained epidemiological differences between fractures of the femoral neck and pertrochanteric fractures. A sensitivity analysis restricted to the subset of hospitals which had participated throughout the whole period of observation, i.e., from the beginning in 1998 onwards, could not be performed. For preserving comparability with previously published work, age-standardization was performed based on data pooled by 10-year age groups. Owing to the exponential increase of femoral fractures with increasing age, this comes at the expense of a loss in granularity. However, with femoral neck fractures taken as an example and using year 1998 as reference year, using 10-year age groups instead of 5-year age groups led to an overestimation of the age-standardized incidence of 1.5% in men and 1.6% in women in year 2021. This overestimation in the extremes is expected to be less in years closer to the reference year. Another limitation of the study pertains to the absence of easily accessible comorbidity and trauma indicators which precluded a more detailed analysis involving trauma velocity and health status at admission. More work is thus needed for better understanding these differences. Similarly, the marked increase in femoral shaft fractures observed in both sexes deserves more research.
In conclusion, femoral fractures are frequent and increasing in number more in men than in women, consistent with a more rapid ageing of the male population aged 45 years and older. While a reversal in the secular trend for hip fractures was confirmed in both sexes, it appeared to occur at the femoral neck fracture level mainly with little or no contribution from the clinically usually more severe pertrochanteric fractures. Fractures of the femoral shaft, albeit remaining at a low incidence, have almost doubled in number over the period of observation in both sexes. Overall, osteoporosis in men requires increased clinical attention.
References
(1993) Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94:646–650. https://doi.org/10.1016/0002-9343(93)90218-e
Kanis JA, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for C, Economic Aspects of O, the Committees of Scientific A, National Societies of the International Osteoporosis F (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Oden A, McCloskey EV, Kanis JA, Harvey NC, Johansson H (2015) Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int 26:2243–2248
Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S, Hip Fracture Study G (2007) Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone 41:958–964
Shane E, Burr D, Abrahamsen B et al (2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29:1–23
Shane E, Burr D, Ebeling PR et al (2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 25:2267–2294
Meier RP, Perneger TV, Stern R, Rizzoli R, Peter RE (2012) Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med 172:930–936
Suhm N, Lamy O, Lippuner K (2008) Management of fragility fractures in Switzerland: results of a nationwide survey. Swiss Med Wkly 138:674–683
Lippuner K, Moghadam BY, Schwab P (2023) The osteoporosis treatment gap in Switzerland between 1998 and 2018. Arch Osteoporos 18:20
Melton L, O’Fallon WM, Riggs B (1987) Secular trends in the incidence of hip fractures. Calcif Tissue Int 41:57–64
Chevalley T, Guilley E, Herrmann FR, Hoffmeyer P, Rapin CH, Rizzoli R (2007) Incidence of hip fracture over a 10-year period (1991–2000): reversal of a secular trend. Bone 40:1284–1289
Guilley E, Chevalley T, Herrmann F, Baccino D, Hoffmeyer P, Rapin CH, Rizzoli R (2008) Reversal of the hip fracture secular trend is related to a decrease of the incidence in institutional-dwelling elderly women. Osteoporos Int 19:1741–1747
Lippuner K, Rimmer G, Stuck AK, Schwab P, Bock O (2022) Hospitalizations for major osteoprotic fractures in Switzerland: a long term trend analysis between 1998 and 2018. Osteoporos Int 33:2327–2335
Sing CW, Lin TC, Bartholomew S et al (2023) Global epidemiology of hip fractures: secular trends in incidence rate, post-fracture treatment, and all-cause mortality. J Bone Miner Res 38:1064–1075
Robine JM, Paccaud F (2005) Nonagenarians and centenarians in Switzerland, 1860–2001: a demographic analysis. J Epidemiol Community Health 59:31–37
(2023) Swiss Federal Office of Statistics. Life expectancy in Switzerland. Available at https://www.bfs.admin.ch/bfs/de/home/statistiken/bevoelkerung/geburten-todesfaelle/lebenserwartung.html. Last accessed July 2023
Sorrentino L, Chiolero A, Carmeli C (2022) Cardiovascular mortality trends in Switzerland 1995–2018. Eur J Public Health 32:891–893
(2021) Swiss Federal Office of Statistics. Plausibility of medical statistics data. Available at https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/erhebungen/ms/applikation-hilfe-benutzer.html#-15052091. Last accessed Novermber 2021.
Lewinnek GE, Kelsey J, White AA 3rd, Kreiger NJ (1980) The significance and a comparative analysis of the epidemiology of hip fractures. Clin Orthop Relat Res 152:35–43
https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/average-annual-percent-change-aapc/#Relative_Advantages_and_disadvantages_AAPC_vs_APCbookmark. Last accessed October 4th, 2023. NCIAAPCAaciAa
Lippuner K, Johansson H, Kanis JA, Rizzoli R (2009) Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int 20:1131–1140
Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashner TM (1999) Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci 54:M635-640
Asada M, Horii M, Ikoma K, Goto T, Okubo N, Kuriyama N, Takahashi K (2021) Hip fractures among the elderly in Kyoto, Japan: a 10-year study. Arch Osteoporos 16:30
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, McCloskey EV, Willers C, Borgstrom F (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16:82
Black DM, Kelly MP, Genant HK et al (2010) Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J Med 362:1761–1771
Black DM, Delmas PD, Eastell R et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Black DM, Cummings SR, Karpf DB et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Black DM, Schwartz AV, Ensrud KE et al (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296:2927–2938
Acknowledgements
We are grateful to Barbara Schaer, Department of Osteoporosis, Inselspital, Bern, for her support with regard to data extraction and to Philippe Kress, MD, Kressmed, Oberembrach, Switzerland, for his contribution to data analysis and his critical review of the manuscript.
Funding
Open access funding provided by University of Bern
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not required by Swiss law for database analyses without individual patient data.
Consent to participate
Not applicable.
Consent for publication
All authors have made substantial contributions to conception and design (KL, MK) and/or analysis and interpretation of the data (MK, KL, PS, RR) and/or important contributions to the manuscript (KL, MK, RR). All authors have seen and approved the final version of the manuscript.
Conflict of interest
None (MK, PS). KL has served as an expert in advisory board meetings of Amgen Switzerland AG and UCB Pharma AG Switzerland. RR is Speaker Bureau or Scientific Advisory Board Member for Abiogen, Dairy UK, Effryx, Naturex, Nestlé, ObsEva, Theramex.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lippuner, K., Kyuchukova, M., Schwab, P. et al. Differences in femoral fracture localizations in men and women in Switzerland between 1998 and 2021—reversal of the secular trend?. Osteoporos Int 35, 893–902 (2024). https://doi.org/10.1007/s00198-024-07016-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07016-5