Abstract
Summary
Orthogeriatric co-management (OGCM) may provide benefits for geriatric fragility fracture patients in terms of more frequent osteoporosis treatment and fewer re-fractures. Yet, we did not find higher costs in OGCM hospitals for re-fractures or antiosteoporotic medication for most fracture sites within 12 months, although antiosteoporotic medication was more often prescribed.
Purpose
Evidence suggests benefits of orthogeriatric co-management (OGCM) for hip fracture patients. Yet, evidence for other fractures is rare. The aim of our study was to conduct an evaluation of economic and health outcomes after the German OGCM for geriatric fragility fracture patients.
Methods
This retrospective cohort study was based on German health and long-term care insurance data. Individuals were 80 years and older, sustained a fragility fracture in 2014–2018, and were treated in hospitals certified for OGCM (ATZ group), providing OGCM without certification (OGCM group) or usual care (control group). Healthcare costs from payer perspective, prescribed medications, and re-fractures were investigated within 6 and 12 months. We used weighted gamma and two-part models and applied entropy balancing to account for the lack of randomization. All analyses were stratified per fracture site.
Results
We observed 206,273 patients within 12-month follow-up, of whom 14,100 were treated in ATZ, 133,353 in OGCM, and 58,820 in other hospitals. Total average inpatient costs per patient were significantly higher in the OGCM and particularly ATZ group for all fracture sites, compared to control group. We did not find significant differences in costs for re-fractures or antiosteoporotic medication for most fracture sites, although antiosteoporotic medication was significantly more often observed in the OGCM and particularly ATZ group for hip, pelvic, and humerus fractures.
Conclusion
The observed healthcare costs were higher in ATZ and OGCM hospitals within 12 months. Antiosteoporotic medication was prescribed more often in both groups for most fracture sites, although the corresponding medication costs did not increase.
Similar content being viewed by others
Introduction
As in many other countries, there is an ongoing demographic shift in the German population. The proportion of older individuals is increasing and is expected to increase further in the future [1]. Thus, geriatric health conditions will become more and more important. Falls are regular events in older and fragile persons, with a high risk for fragility fractures [2]. The incidence, number, and severity of negative consequences after these fractures increase with age [3, 4]. Fragility fractures may lead to numerous negative health consequences including pain, immobility, reduced quality of life, care dependence, and mortality, with the impact depending on the fracture site [5,6,7,8].
For a frail, geriatric patient, a fragility fracture may be only one among a number of comorbidities that may exceed the scope and expertise of orthopaedic surgeons. To better deal with the special needs of those patients, collaborative orthogeriatric care has been developed and implemented in the last years [9,10,11,12], initially for the treatment of hip fracture patients. Numerous studies investigated forms of multidisciplinary treatment approaches involving orthopaedic surgeons and geriatricians regarding health-related and health-economic outcomes after fragility fractures.
As collaborative orthogeriatric care was initially intended for hip fractures, most studies focused on these fractures and found beneficial effects compared to usual care regarding in-hospital [10, 13, 14], 30-day [15,16,17,18,19,20,21], and 1-year mortality [10, 14, 18, 22,23,24], regain of functional status and walking ability [13, 24, 25], and more quality-adjusted life years [22, 26]. Studies focusing on pelvic and spine fractures found benefits compared to usual care in terms of more identified complications [27, 28] and fewer revision surgeries necessary [28]. However, evidence on mortality for fracture sites other than hip or outcomes for humerus and forearm fractures is less conclusive or lacking at all [27,28,29,30]. Overall, collaborative orthogeriatric care might be beneficial for the treatment of non-hip fragility fractures as well, but as to date, comprehensive evidence is scarce.
Literature showed a treatment gap for patients eligible for osteoporosis treatment [31], which was found to even increase [32]. Therefore, a key element of collaborative orthogeriatric care usually is screening for and treatment of an underlying osteoporosis to improve the bone quality and to prevent possible secondary fractures as the risk for a secondary fracture is particularly high after a preceding fracture [33,34,35]. A large systematic review and meta-analysis found higher treatment rates of osteoporosis treatment in both antiosteoporotic drug initiation and vitamin D and calcium supplementation compared to usual care for hip fractures [36]. For other fragility fractures including pelvic and spine fractures, studies found potential benefits as well [28, 29, 37, 38].
For secondary fractures, the evidence is scarce and less conclusive for hip fracture patients [36], and non-existent for other fractures at all. Studies found no significant differences [18, 39, 40] or only a slightly decreased re-fracture rate [41, 42] after collaborative orthogeriatric care measures compared to usual care.
As fragility fractures cause high healthcare consumption and may entail a reduced functional ability and even care dependence, their economic burden is high [4,5,6,7], depending on the fracture site. Several systematic reviews and meta-analyses found decreased healthcare costs for acute hospital stay and within 12–18-month follow-up for hip fracture patients after collaborative orthogeriatric care compared to usual care [14, 24, 36]. However, most of the included studies observed a shorter length of stay for patients treated with collaborative orthogeriatric care while studies from Germany did not find a reduced [28, 29] or even an increased length of stay [21, 43], thus entailing increased healthcare costs [44].
Different models of collaborative orthogeriatric care have been developed, e.g., treatment in an orthopaedic ward with regular or requested geriatric consultations, initial treatment in an orthopaedic ward and transfer to a geriatric ward, or joint treatment by an orthopaedic surgeon and a geriatrician. Thus, precise terms differ [9, 45]. Evidence is inconclusive which of these models is most beneficial, but early involvement of a geriatric interdisciplinary team seems to be favorable. In Germany, the term orthogeriatric co-management (OGCM) describes a hospital treatment either on a geriatric or an orthopaedic ward, which is delivered by a multidisciplinary geriatric team headed by a geriatrician. Elements of the OGCM are standardized comprehensive geriatric assessments, early mobilization, and inpatient rehabilitation starting few days after hospital admission. Inpatient rehabilitation is usually delivered either during OGCM in a hospital or subacute in a separate rehabilitation facility. Offering both forms subsequently is also possible.
The aim of our study was to compare healthcare costs, particularly costs for medication from the treatment of osteoporosis and costs of re-fractures after a fragility fracture, as well as health outcomes, in particular the corresponding treatment of osteoporosis and re-fractures, in geriatric patients treated in German hospitals providing collaborative orthogeriatric care, compared to patients treated in hospitals providing usual care within 6 and 12-month follow-up. For this purpose, hospitals providing collaborative orthogeriatric care were subdivided into hospitals certified for OGCM treatment as geriatric traumatology centers (“Alterstraumatologisches Zentrum”; ATZ) or providing OGCM treatment without certification.
Data and methods
Study design, data source, and selection criteria
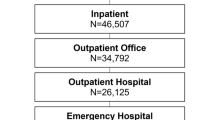
For this retrospective cohort study, we used nationwide health and long-term care insurance claims data provided by the “Wissenschaftliches Institut der AOK” (“WIdO”) for the years 2013–2019. WIdO administers data of the largest association of statutory health insurance companies in Germany, covering about one-third of the population. We included patients if they sustained an incident fracture of the hip (hospital discharge diagnosis S72.0 or S72.1 from the 10th revision of the International Classification of Diseases (ICD-10)), pelvic (ICD-10: S32.1, S32.3, S32.4, S32.5, S32.81, S32.83), spine (ICD-10: S12.0, S12.1, S12.2, S12.7, S12.9, S22.0, S22.1, S32.0), humerus (S42), or forearm (S52). Additionally, we included patients with a hospital stay due to osteoporosis with pathological fracture (ICD-10: M80) as discharge diagnosis and one of the mentioned ICD-10 codes as admission or secondary diagnosis as well. We excluded patients with more than one fracture location according to secondary diagnoses (n = 42). The index period for the incident fracture was from January 2014 until December 2018. Patients were then followed for 6 and 12 months (follow-up period) or until death. As a baseline, we used 1 year prior to the index date for risk adjustment. To ensure that fractures were incident, i.e., the first fracture within a time period, we used a washout period of 180 days preceding the index stay and excluded cases with a fracture within this period.
As we analyzed an intervention for geriatric patients, we applied the definition of geriatric patients by the German Society for Geriatric Medicine [46] and excluded patients younger than 80 years. We excluded patients who changed their insurance or patients treated in hospitals with an extraordinarily high (≥ 99% percentile; n = 1 hospital) hospital volume of fracture cases to improve the comparability and reduce possible heterogeneity between all groups. Furthermore, patients were excluded if the treating hospital transferred more than 5% of their total fracture patients (n = 462 hospitals), as we could not clearly determine the treating hospital in such cases.
Intervention
OGCM is defined by the operation and procedure code “OPS8-550” in health insurance claims data. It is a rehabilitation treatment lasting 7, 14, or 21 days (depending on the subcode) which is provided by a multidisciplinary team of physiotherapists, occupational therapists, specifically trained nurses, social workers, and others, and headed by a geriatrician. The intervention involves standardized geriatric assessments, early mobilization, antiosteoporotic medication if needed, regular team meetings, and a rehabilitation plan with functional goals and a focus on geriatric syndromes. It can be delivered on a geriatric or orthopaedic ward. OGCM is offered additionally to the usual care of the fracture (e.g., surgery) which does not intend contact with a geriatrician. Further information can be found elsewhere [21]. As there is a high reimbursement due to the OPS8-550 code, data are thoroughly checked and can be assumed accurate.
Patients were categorized into groups on hospital level. If hospitals were certified for the OGCM treatment as ATZ by a standardized assignment, their patients were categorized as ATZ group. If hospitals had no certification, but treated at least 10 fracture cases per year with the OPS8-550 procedure, they were considered as providing OGCM measures, and their treated patients were classified as OGCM group. All patients treated in other hospitals were categorized as control group. Otherwise, when focusing on patients who actually received OPS8-550, we would introduce an immortal time bias. The OPS8-550 code requires patients to survive and receive at least 7, 14, or 21 days of treatment by definition. The assignment of groups on hospital level based on the treatment of patients in the hospitals overcomes this problem. Not all fracture patients in ATZ or OGCM hospitals may have actually received the intervention. Yet, they may still have benefited from the multidisciplinary OGCM team.
Outcomes
Direct healthcare costs included costs for inpatient stays and medication over the follow-up. Inpatient costs were subdivided into costs due to the index stay and costs for the inpatient treatment for re-fractures. Medication costs were subdivided into costs for antiosteoporotics and vitamin D and calcium. Costs were reported in 2019 Euro and adjusted for inflation using the gross domestic product price index [47, 48]. All costs were available from claims data and we winsorized all costs at the 99% percentile to avoid bias by extreme outliers. We applied a payer perspective. In Germany, health insurances reimburse almost all costs for fracture treatment which implies that healthcare costs differ only marginally between the payer’s and the societal perspective. An exception would be long-term care where recipients have to pay a large share of costs and therefore the payer’s and the societal perspective differ.
To compare the observed healthcare costs with corresponding health effects and medications, we calculated the following outcomes. We observed the number of all medications the patients received and in particular new antiosteoporotic medication (bisphosphonates and combinations; ATC: M05BA, M05BB, M05BX) and new vitamin D or calcium (ATC: A11CC, A12AX) after hospital discharge until the end of follow-up. The number of re-fractures per patient was observed as the number of hospital re-admission with one of the above-defined diagnoses. We estimated survived lifetime within 1 year. Furthermore, a fracture-free lifetime within 1 year was calculated as survived time free of fractures.
Risk adjustment
Unfortunately, we could not randomly assign patients to the groups. Due to the lack of randomization, selection bias and unbalanced baseline characteristics may occur. In order to reduce confounding, we applied entropy balancing (EB) [49] to remove inequalities in the baseline variables. EB reweights each individual of the control group such that the covariates in the control group equals the ATZ or OGCM group, respectively, in mean, variance, and skewness. This allows the maximization of the comparability of the groups concerning the risk adjustment variables.
We considered the following variables during baseline or at index fracture date: sex; age at hospital admission date of the index stay; number of months with care degrees 1–5 during baseline; number of months living in a nursing home during baseline; healthcare costs during baseline for inpatient treatment, outpatient treatment, devices/medical appliances, and medication; medication-based comorbidities during baseline [50, 51]; hospital volume defined as mean number of fracture cases per hospital and fracture site, weighted with the market share of the health insurance per federal state; year of treatment.
EB has potential limitations if there are inconsistent balance constraints or extreme differences between groups. This may be possible if the distributions of the variables of the groups have little overlap. We avoided this by checking each variable’s distribution and the EB results and by excluding variables with less than 1% of observations (i.e., the comorbidities cancer, HIV, intestinal inflammatory diseases, migraines, and tuberculosis). The weights calculated with EB were used for all statistical analyses.
Statistical analysis
We estimated healthcare costs in two steps. Not for all patients costs occurred (e.g., if they did not sustain a re-fracture during follow-up). Therefore, we used weighted logistic regressions to estimate the likelihood of the occurrence of costs. The amount of costs usually is not normally distributed, but instead positive, right-skewed, and with some outliers. Therefore, weighted generalized linear models with a gamma distribution and a log link function were applied to estimate the amount of costs [52]. To mutually estimate the likelihood of occurring costs and the amount of costs, if occurred, we applied weighted two-part models [53]. However, we estimated inpatient and index hospital stay costs using weighted generalized linear models with a gamma and a log link function only, as the follow-up started at hospital admission and thus these costs occurred for every patient. The probability of medications and re-fractures was estimated with logistic regressions. Mean differences in life years and fracture-free life years were tested using t-tests.
All analyses were conducted per fracture site, both follow-up periods, and for ATZ compared to control group and OGCM compared to control group separately. All results were presented as average marginal means. All calculations were performed using SAS software v9.4 (SAS Institute Inc, Cary, NC), Stata 17 (StataCorp, College Station, TX), and R 4.2.3. (R Foundation for Statistical Computing, Vienna, Austria). This study was approved by the ethics committee of the University of Ulm (177/20).
Results
In total, we observed 206,273 patients within the follow-up of 12 months, of whom 14,100 were treated in ATZ, 133,353 in OGCM, and 58,820 in usual care hospitals. Of all patients, 91,813 sustained a fracture of the hip, 21,156 of the pelvic, 35,482 of the spine, 31,984 of the humerus, and 25,838 of the forearm. For the follow-up of 6 months, we observed 206,373 patients. About 75–93% of the patients were female and the mean age was 85–87 years, depending on the fracture site. Baseline differences between ATZ or OGCM and the control group were mainly observable in the number of fracture cases per hospital and the amount of baseline healthcare costs (both higher for ATZ and OGCM groups). However, after EB, both groups were virtually equal in terms of mean, variance, and skewness of the risk adjustment variables. Descriptive characteristics and results from EB are displayed in supplementary tables 1–20.
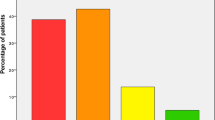
Total inpatient healthcare costs were significantly increased for all fracture sites in the ATZ and OGCM groups within 12 months. Those costs were mainly driven by higher costs due to the index stay. Costs for antiosteoporotic medication were significantly but slightly increased only for hip (ATZ group) and spine (OGCM group) fractures within 12 months (see Fig. 1), although the probability of prescription significantly but slightly increased for pelvic and humerus fractures as well (see Fig. 2). For vitamin D and calcium, costs slightly increased after hip, spine (OGCM group only), and humerus (ATZ group only) within 12 months (see Fig. 3), although the probability of prescription significantly increased after all fractures in both groups (see Fig. 4).
To further investigate these differing effects in costs and prescriptions, we displayed the number of prescriptions over 12 months starting from hospital discharge and compared them between ATZ, OGCM, and control groups, respectively. Both for the prescription of antiosteoporotic medications (supplementary Figs. 1 and 2) and vitamin D and calcium (supplementary Figs. 3 and 4), prescriptions were high shortly after hospital discharge and decreased after 1–2 months. This was more pronounced in the OGCM and even more in the ATZ group. Particularly for high-dose vitamin D (supplementary Figs. 5 and 6), this effect could be observed.
The amount of costs for re-fractures within 12 months significantly increased after incident hip fractures in the OGCM group (see Fig. 5), although the probability of re-fractures did not significantly differ for any group (see Fig. 6).
Furthermore, in the ATZ group, lifetime and fracture-free lifetime within 12-month follow-up were significantly but slightly increased compared to the control group for pelvic fractures. In the OGCM group, lifetime and fracture-free lifetime were significantly but slightly increased within 12-month follow-up compared to the control group for humerus fractures.
When repeating the analyses for 6-month follow-up, we again found significantly increased total inpatient healthcare costs after all fractures and in both groups. Furthermore, costs for antiosteoporotic medication were significantly increased after hip (ATZ group only) and spine (OGCM group only) fractures, and for vitamin D and calcium after hip, pelvic (OGCM group only), spine (OGCM group only), and humerus (ATZ group only) fractures. We found no significant differences in costs due to re-fractures within 6 months. Detailed results are available in supplementary tables 21–40.
Discussion
In this study, we evaluated healthcare costs and health outcomes of hospitals certified for OGCM treatment, hospitals providing OGCM treatment, and hospitals offering usual care for geriatric fragility fracture patients in Germany within 1 year. Costs were higher in hospitals with both certified or uncertified OGCM treatment, particularly due to index treatment costs. The results stand in line with two other studies [26, 44] which found increased costs associated with collaborative orthogeriatric care. However, other existing studies found reduced costs of collaborative orthogeriatric care during the hospital stay compared to the control group [24].
The main reason for these differences between countries may be the design of the OGCM treatment in Germany. It comprises inpatient rehabilitation and early mobilization at the hospital and therefore intends a longer hospital stay than usual care, as opposed to other countries. In Germany, OGCM can only be reimbursed if the patient survived and received the treatment for at least 7, 14, or 21 days, which leads to a long hospital stay. Thus, costs for OGCM are intended to increase in Germany. Particularly for usual care, but also possible for OGCM, an additional inpatient rehabilitation stay in a separate facility can be delivered.
Further reasons for the diverging study results might be different health and reimbursement systems in other countries, which restrict the comparability of the results, different study designs, and different models of collaborative orthogeriatric care, as these differ depending on the country [10]. Some studies analyzed models where the geriatrician is the primary physician who coordinates all services; others focused on models where geriatricians are consulted on a regular basis or request.
Moreover, we could only consider a maximum of 12-month follow-up due to data availability, which may not accurately estimate total inpatient healthcare costs in the long run. Costs were particularly high at the beginning of follow-up according to the considerable costs of the index fracture which, however, only occurred once. Over a longer follow-up, total costs would increase less sharply, although other costs would increase, for example, those for medication or re-fractures. The limited follow-up period may also affect the observed lifetime and fracture-free lifetime, which were only found to slightly increase for pelvic fractures in the ATZ group and humerus fractures in the OGCM group. A longer follow-up may likely increase both outcomes.
When focusing on costs due to medication, we found statistically significant differences in costs only for some fracture sites regarding antiosteoporotic medication and regarding costs for vitamin D and calcium, respectively. This stands in contrast to the increased rates of prescription of antiosteoporotic medication, vitamin D, and calcium for almost all or all fracture sites in ATZ and OGCM hospitals. However, both costs and prescription rates were only slightly increased. When focusing on 6 instead of 12-month follow-up, we did find significantly increased costs due to antiosteoporotic medication, vitamin D, and calcium for some fracture sites. We could observe that those medications were prescribed more often after treatment in the OGCM and particularly the ATZ group, but less so in the long run. Furthermore, vitamin D and calcium require a prescription only in high doses and are otherwise over-the-counter medications with out-of-pocket expenses for the patients instead of health insurance. Probably, a high dose was prescribed initially and the patients were then required to purchase lower doses at their own expense.
In line with existing literature [36], we found no significantly different rates of re-fractures after treatment in an ATZ or OGCM hospital. Despite this fact, we found increased inpatient costs due to re-fractures after an incident hip fracture. When assuming that patients’ secondary fractures were treated in the same hospital as the first (e.g., due to spatial proximity), higher costs for the index fracture in OGCM/ATZ hospitals might explain higher costs for re-fractures despite not finding statistically significantly higher re-fracture rates. The increased prescription of antiosteoporotic medication, vitamin D, and calcium may have a preventive effect on re-fractures as suggested in literature [54]. However, this increase in prescription was only small and the follow-up period limited to only 12 months, which might explain why we could not observe a reduction in re-fracture rates. Furthermore, the slight increase in prescriptions and the slight decrease in re-fractures may point to limited prevention of secondary fractures in Germany due to restricted budgets and unclear responsibility of hospitals, general practitioners, or specialists. The current German guideline for the treatment of osteoporosis calls for more and faster medication and clear responsibilities after fragility fractures in order to provide better and more comprehensive prevention [55].
In our study, differences in outcomes often were higher when comparing the ATZ with the usual care group than comparing the OGCM with the usual care group. This seems plausible, as certain standardized expenses are necessary for the hospital to achieve a certification for the OGCM treatment. Furthermore, the hospital’s certification may suggest that a higher proportion of patients actually received the OGCM treatment compared to the hospitals offering OGCM without certification. The actual reimbursement due to the OPS8-550 code was relatively high for hip fractures (ATZ group: 57.51%; OGCM group: 44.88%) and pelvic fractures (ATZ group: 43.84%; OGCM group: 36.05%), mediocre for humerus fractures (ATZ group: 31.07%; OGCM group: 24.26%) and spine fractures (ATZ group: 29.75%; OGCM group: 27.21%), and low for forearm fractures (ATZ group: 9.40%; OGCM group: 9.83%).
Our study has some limitations. Groups were classified on hospital instead of patient level, which may bias the effects because not all patients assigned to one of the intervention groups actually received OGCM. However, when categorizing groups on patient level, we would have implied an immortal time bias as only for cases who survived at least 7, 14, or 21 days after hospital admission the OGCM procedure was reimbursed and recorded in the claims data. Yet, other patients in the ATZ or OGCM group not actually receiving the treatment may still have benefitted from the presence of a multidisciplinary OGCM team or the established standards in the hospital. In the same vein, it might be possible that a few patients in the usual care group actually received OGCM treatment after transfer to another hospital, as we only considered the first treating hospital for group assignment. Furthermore, we excluded patients who were treated in hospitals that frequently transferred patients to other groups in order to ensure they were treated in the group they were assigned to. Moreover, health insurance claims data does not comprise all relevant covariates which might be relevant confounders, for example, information on lifestyle, nutrition, risky health behavior, or details on the treatment and the severity of the fracture.
Our study has some important strengths. We used a large dataset with information from over 200,000 patients for the years 2013 through 2019. We used health and long-term care insurance claims data from the AOK which are not as vulnerable to dropout, information, and selection biases as, e.g., survey data. The AOK has the highest coverage in Germany insuring about one-third of its inhabitants, which makes our results quite representative for Germany and similar countries. We used the reweighting algorithm entropy balancing to reduce confounding due to potential selection bias and diverging baseline characteristics. Entropy balancing works well in large datasets like ours and for covariates with frequent observations [56]. To our knowledge, this is the first study assessing the costs of hospitals providing collaborative orthogeriatric care, in particular costs of medication due to osteoporosis and re-fractures from a broad payer perspective with a large number of patients.
Conclusion
This retrospective cohort study is the largest evaluation of costs and health outcomes, considering in particular osteoporosis treatment and re-fractures, after collaborative orthogeriatric care for geriatric patients with fragility fractures from Germany within 12-month follow-up. It showed an increased utilization of healthcare measures in terms of healthcare costs as intended by collaborative orthogeriatric care, driven by inpatient costs for the treatment of primary and partly even secondary fractures. Although the rate of incidentally prescribed medication for the treatment of osteoporosis increased after the primary fracture, we found no increased medication costs in the long run. Total costs are likely to increase less sharply with a longer follow-up, as costs for immediate treatment occur only once per fracture.
Data availability
The German statutory health insurance AOK owns the datasets supporting the conclusions of this article. Since public deposition of the data would breach ethical and legal compliance, data are only available upon formal request from the research institute of the AOK (WIdO). To request the data please contact the institutional body of the WIdO (wido@wido.bv.aok.de). In order to fulfill the legal requirements to obtain that kind of data, researchers must obtain permission for a specific research question from the German Federal (Social) Insurance Office. Additionally, researchers must conclude a contract with the statutory health insurance regarding data access which can be requested from the “AOK-Bundesverband GbR” (Federal Association of Local Health Insurance Funds) under http://aok-bv.de/kontakt/. The licensee is permitted to use the data for the purpose of the research proposal within their company, exclusively. Thereby, a company is defined as an economical unit. Licensees are not allowed to pass the data to a third party or to create Software or databases with the exception of scientific publications. Moreover, the study has to be approved by the data protection officer both at the statutory health insurance and the research institute.
References
Statistisches Bundesamt Deutschland (2015) Bevölkerung Deutschlands bis 2060: 13. koordinierte Bevölkerungsvorausrechnung. Statistisches Bundesamt, Wiesbaden
Bukata SV, DiGiovanni BF, Friedman SM, Hoyen H, Kates A, Kates SL, Mears SC, Mendelson DA, Serna FH Jr, Sieber FE (2011) A guide to improving the care of patients with fragility fractures. Geriatric Orthop Surg Rehab 2:5–37
Sànchez-Riera L, Wilson N (2017) Fragility fractures & their impact on older people. Best Pract Res Clin Rheumatol 31:169–191
Muschitz C, Hummer M, Grillari J, Hlava A, Birner A, Hemetsberger M, Dimai H (2021) Epidemiology and economic burden of fragility fractures in Austria. Osteoporos Int 33:1–11
Hartholt KA, van Beeck EF, Polinder S, van der Velde N, van Lieshout EM, Panneman MJ, van der Cammen TJ, Patka P (2011) Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma: Injury, Infect Crit Care 71:748–753
Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA (2005) The human cost of fracture. Osteoporos Int 16:2046–2052
World Health Organization (WHO) Scientific Group (2003) The burden of musculoskeletal conditions at the start of the new millennium. World Health Organ Tech Rep Ser 919:i
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet (London, England) 359:1761–1767
Kammerlander C, Roth T, Friedman S, Suhm N, Luger T, Kammerlander-Knauer U, Krappinger D, Blauth M (2010) Ortho-geriatric service—a literature review comparing different models. Osteoporos Int 21:637–646
Grigoryan KV, Javedan H, Rudolph JL (2014) Ortho-geriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28:e49
Moyet J, Deschasse G, Marquant B, Mertl P, Bloch F (2019) Which is the optimal orthogeriatric care model to prevent mortality of elderly subjects post hip fractures? A systematic review and meta-analysis based on current clinical practice. Int Orthop 43:1449–1454
Sabharwal S, Wilson H (2015) Orthogeriatrics in the management of frail older patients with a fragility fracture. Osteoporos Int 26:2387–2399
Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM (2010) Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ (Clin Res ed) 340:c1718
Van Heghe A, Mordant G, Dupont J, Dejaeger M, Laurent MR, Gielen E (2022) Effects of orthogeriatric care models on outcomes of hip fracture patients: a systematic review and meta-analysis. Calcif Tissue Int 110(2):162–184
Zeltzer J, Mitchell RJ, Toson B, Harris IA, Ahmad L, Close J (2014) Orthogeriatric services associated with lower 30-day mortality for older patients who undergo surgery for hip fracture. Med J Aust 201:409–411
Kristensen PK, Thillemann TM, Søballe K, Johnsen SP (2015) Can improved quality of care explain the success of orthogeriatric units? A population-based cohort study. Age Ageing 45:66–71
Forni S, Pieralli F, Sergi A, Lorini C, Bonaccorsi G, Vannucci A (2016) Mortality after hip fracture in the elderly: the role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch Gerontol Geriatr 66:13–17
Hawley S, Javaid MK, Prieto-Alhambra D, Lippett J, Sheard S, Arden NK, Cooper C, Judge A (2016) Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age Ageing 45:236–242
Middleton M, Wan B, da Assunçāo R (2017) Improving hip fracture outcomes with integrated orthogeriatric care: a comparison between two accepted orthogeriatric models. Age Ageing 46:465–470
Stenqvist C, Madsen CM, Riis T, Jørgensen HL, Duus BR, Lauritzen JB, van der Mark S (2016) Orthogeriatric service reduces mortality in patients with hip fracture. Geriatric Orthop Surg Rehab 7:67–73
Rapp K, Becker C, Todd C, Rothenbacher D, Schulz C, König H-H, Liener U, Hartwig E, Büchele G (2020) The association between orthogeriatric co-management and mortality following hip fracture: an observational study of 58 000 patients from 828 hospitals. Dtsch Arztebl Int 114:53–59
Ginsberg G, Adunsky A, Rasooly I (2013) A cost-utility analysis of a comprehensive orthogeriatric care for hip fracture patients, compared with standard of care treatment. Hip Int 23:570–575
Folbert E, Hegeman J, Vermeer M, Regtuijt E, van der Velde TD, Ten Duis H, Slaets J (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28:269–277
Eamer G, Saravana-Bawan B, van der Westhuizen B, Chambers T, Ohinmaa A, Khadaroo RG (2017) Economic evaluations of comprehensive geriatric assessment in surgical patients: a systematic review. J Surg Res 218:9–17
Wang H, Li C, Zhang Y, Jia Y, Zhu Y, Sun R, Li W, Liu Y (2015) The influence of inpatient comprehensive geriatric care on elderly patients with hip fractures: a meta-analysis of randomized controlled trials. Int J Clin Exp Med 8:19815
Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, Lydersen S, Halsteinli V, Saltnes T, Lamb SE (2015) Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet 385:1623–1633
Laubach M, Gruchow LC, Hafner T, Migliorini F, Knobe M, Hildebrand F, Pishnamaz M (2021) In-hospital clinical outcomes in patients with fragility fractures of the lumbar spine, thoracic spine, and pelvic ring: a comparison of data before and after certification as a dgu® geriatric trauma centre. Medicina 57:1197
Hafner T, Kollmeier A, Laubach M, Knobe M, Hildebrand F, Pishnamaz M (2021) Care of geriatric patients with lumbar spine, pelvic, and acetabular fractures before and after certification as a geriatric trauma center DGU®: a retrospective cohort study. Medicina 57:794
Knobe M, Böttcher B, Coburn M, Friess T, Bollheimer L, Heppner H, Werner C, Bach J-P, Wollgarten M, Poßelt S (2019) AltersTraumaZentrum DGU®: Evaluation klinischer und ökonomischer Parameter. Unfallchirurg 122:134–146
Buecking B, Timmesfeld N, Riem S, Bliemel C, Hartwig E, Friess T, Liener U, Ruchholtz S, Eschbach D (2013) Early orthogeriatric treatment of trauma in the elderly: a systematic review and metaanalysis. Dtsch Arztebl Int 110:255
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:1–115
Borgström F, Karlsson L, Ortsäter G, Norton N, Halbout P, Cooper C, Lorentzon M, McCloskey EV, Harvey NC, Javaid MK (2020) Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos 15:1–21
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C, Group OM, Group ORA (2002) Meta-analyses of therapies for postmenopausal osteoporosis. IX: Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
Wong RMY, Wong PY, Liu C, Wong HW, Chung YL, Chow SKH, Law SW, Cheung WH (2022) The imminent risk of a fracture—existing worldwide data: a systematic review and meta-analysis. Osteoporos Int 33:2453–2466
Van Camp L, Dejaeger M, Tournoy J, Gielen E, Laurent MR (2020) Association of orthogeriatric care models with evaluation and treatment of osteoporosis: a systematic review and meta-analysis. Osteoporos Int 31:2083–2092
Schray D, Neuerburg C, Stein J, Gosch M, Schieker M, Böcker W, Kammerlander C (2016) Value of a coordinated management of osteoporosis via Fracture Liaison Service for the treatment of orthogeriatric patients. Eur J Trauma Emerg Surg 42:559–564
Goltz L, Degenhardt G, Maywald U, Kirch W, Schindler C (2013) Evaluation of a program of integrated care to reduce recurrent osteoporotic fractures. Pharmacoepidemiol Drug Saf 22:263–270
Gregersen M, Mørch MM, Hougaard K, Damsgaard EM (2012) Geriatric intervention in elderly patients with hip fracture in an orthopedic ward. J Injury Violence Res 4:45
Li Y, Tung K-K, Cho Y-C, Lin S-Y, Lee C-H, Chen C-H (2022) Improved outcomes and reduced medical costs through multidisciplinary co-management protocol for geriatric proximal femur fractures: a one-year retrospective study. BMC Geriatr 22:318
Duaso E, Formiga F, Marimón P, Sandiumenge M, Salgado MT, Murga V, Gamboa A, Rodriguez C, Castellà J, Escalante E (2018) Advantages of care for patients with hip fractures in the acute geriatric unit: Hip study Anoia. Geriatr Gerontol Int 18:407–414
Cheung W-H, Shen W-Y, Dai DL-K, Lee KB, Zhu TY, Wong RM-Y, Leung K-S (2018) Evaluation of a multidisciplinary rehabilitation programme for elderly patients with hip fracture: a prospective cohort study. J Rehabil Med 50:285–291
Grund S, Roos M, Duchene W, Schuler M (2015) Treatment in a center for geriatric traumatology. Dtsch Arztebl Int 112:113–119
Schulz C, Büchele G, Peter RS, Rothenbacher D, Brettschneider C, Liener UC, Becker C, Rapp K, König H-H (2021) Health-economic evaluation of collaborative orthogeriatric care for patients with a hip fracture in Germany: a retrospective cohort study using health and long-term care insurance claims data. Euro J Health Econ 22:873–885
Pioli G, Giusti A, Barone A (2008) Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res 20:113–122
Sieber C (2007) The elderly patient–who is that? Internist 48:1190–1194
Organisation for Economic Co-operation and Development (2018) Economic References. https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_ECOR# Accessed 05.07.2019 2019
Glick HA, Doshi JA, Sonnad SS, Polsky D (2014) Economic evaluation in clinical trials. Oxford University Press, Oxford
Hainmueller J (2012) Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal 20:25–46
Huber CA, Szucs TD, Rapold R, Reich O (2013) Identifying patients with chronic conditions using pharmacy data in Switzerland: an updated mapping approach to the classification of medications. BMC Public Health 13:1030
Huber CA, Schneeweiss S, Signorell A, Reich O (2013) Improved prediction of medical expenditures and health care utilization using an updated chronic disease score and claims data. J Clin Epidemiol 66:1118–1127
Barber J, Thompson S (2004) Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy 9:197–204
Belotti F, Deb P, Manning WG, Norton E (2015) twopm: two-part models. Stand Genomic Sci 15:3–20
Saito T, Sterbenz J, Malay S, Zhong L, MacEachern M, Chung K (2017) Effectiveness of anti-osteoporotic drugs to prevent secondary fragility fractures: systematic review and meta-analysis. Osteoporos Int 28:3289–3300
Leitlinie des Dachverbands der Deutschsprachigen Wissenschaftlichen Osteologischen Gesellschaften e.V. (2023) Prophylaxe, Diagnostik und Therapie der Osteoporose bei postmenopausalen Frauen und bei Männern ab dem 50. Lebensjahr. https://register.awmf.org/de/leitlinien/detail/183-001. Accessed 1 Oct 2023
Matschinger H, Heider D, König H-HJDG (2020) A comparison of matching and weighting methods for causal inference based on routine health insurance data, or: what to do if an RCT is impossible. Das Gesundheitswesen 82:S139–S150
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was funded by the Federal Joint Committee (Gemeinsamer Bundesausschuss) (grant number 01VSF19028).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the ethics committee of the University of Ulm (177/20). For this type of study with anonymized data, formal consent is not required.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Konnopka, C., Büchele, G., Jaensch, A. et al. Evaluation of costs, osteoporosis treatment, and re-fractures in German collaborative orthogeriatric care after fragility fractures. Osteoporos Int 35, 81–91 (2024). https://doi.org/10.1007/s00198-023-06965-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06965-7