Abstract
Introduction and Hypothesis
Bladder pain syndrome (BPS) is a debilitating condition characterised by exaggerated bladder sensations and altered bladder function. It is still unknown whether the condition is a peripheral sensory problem or due to abnormal central sensory processing as seen in central sensitisation. This systematic review, which followed a published and Prospective Register of Systematic Reviews-registered protocol (CRD42021229962), is aimed at establishing the scope of central sensitisation in patients with BPS to aid optimal management and treatment.
Methods
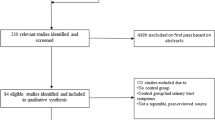
Four databases were searched, and appraisal of the identified studies was conducted by two independent reviewers based on eligibility criteria: patients with BPS being investigated for central sensitisation with or without comparison of controls, English-language articles, full text and publication in a peer-reviewed journal. The Methodological Index for non-Randomised Studies was used to determine study quality. We identified 763 papers in total, with 15 studies included in the final analysis. All studies were observational and had a low risk of bias. Measures included in the evaluation of CS were questionnaires, urodynamics, and quantitative sensory testing methods.
Results
There was evidence of central sensitisation in patients with BPS in all papers evaluated (15 out of 15). In addition, more significant central sensitisation correlated with severe disease presentation (3 out of 3 papers) and concomitant chronic pain conditions (5 out of 5 papers).
Conclusions
Central sensitisation plays an integral role in BPS patient pathology. Many secondary measures are used to evaluate this condition. Stratification of patients based on their pathology (peripheral, central or a combination of the two) will aid in implementing an individualised management strategy.


Similar content being viewed by others
Data Availability
The data that support the findings of this paper are available on request from the lead author.
References
Offiah I, McMahon SB, O’Reilly BA. Interstitial cystitis/bladder pain syndrome: diagnosis and management. Int Urogynecol J. 2013;24(8):1243–58.
Doggweiler R, Whitmore KE, Meijlink JM, et al. A standard for terminology in chronic pelvic pain syndromes: a report from the chronic pelvic pain working group of the international continence society. Neurourol Urodyn. 2017;36(4):984–1008.
Offiah I, Didangelos A, Dawes J, et al. The expression of inflammatory mediators in Bladder Pain Syndrome. Eur Urol. 2016;70(2):283–90.
Wall PD, McMahon SB, Koltzenburg M. Wall and Melzack’s textbook of pain. 5th edn. Philadelphia: Elsevier/Churchill Livingstone. 2006.
Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139:267–84.
Latremoliere A, Woolf CJ. Central sensitisation: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895–926.
Woolf CJ. Central sensitisation: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2–15.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA group. BMJ. 2009;339:b2535.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomised studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–6.
Lai HH, Newcomb C, Harte S, et al. Comparison of deep phenotyping features of UCPPS with and without Hunner lesion: a MAPP-II Research Network Study. Neurourol Urodyn. 2021;40:810–8.
Hellman KM, Roth GE, Dillane KE, et al. Dysmenorrhea subtypes exhibit differential quantitative sensory assessment profiles. Pain. 2020;161:1227–36.
Thu JHL, Vetter J, Lai HH. The severity and distribution of non-urologic pain and urogenital pain in overactive bladder are intermediate between interstitial cystitis and controls. Urology. 2019;130:59–64.
Offiah I, Dilloughery E, McMahon SB, O’Reilly BA. Prospective comparative study of the effects of lidocaine on urodynamic and sensory parameters in bladder pain syndrome. Int Urogynaecol J. 2019;30:1293–301.
Harte SE, Schrepf A, Gallop R, et al. Quantitative assessment of non-pelvic pressure pain sensitivity in urologic chronic pelvic pain syndrome: a MAPP research network study. Pain. 2019;160(6):1270–80.
Cervigni M, Onesti E, Ceccanti M, et al. Repetitive transcranial magnetic stimulation for chronic neuropathic pain in patients with bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2018;37:2678–87.
Grinberg K, Granot M, Lowenstein L, Abramov L, Weissman-Fogel I. A common pronociceptive pain modulation profile typifying subgroups of chronic pelvic pain syndromes is interrelated with enhanced clinical pain. Pain. 2017;158:1021–9.
Chelimsky G, Simpson P, McCabe N, Zhang L, Chelimsky T. Autonomic testing in women with chronic pelvic pain. J Urol. 2016;196(2):429–34.
Schrepf A, Bradley CS, O’Donnell M, et al. Toll-like receptor 4 and comorbid pain in interstitial cystitis/bladder pain syndrome: a multidisciplinary approach to the study of chronic pelvic pain research network study. Brain Behav Immun 2015;49:66–74.
Lai HH, Gardner V, Ness TJ, Gereau RW IV. Segmental hyperalgesia to mechanical stimulus in interstitial cystitis/bladder pain syndrome: evidence of central sensitization. J Urol. 2014;191(5):1294–9.
Ness TJ, Lloyd LK, Fillingim RB. An endogenous pain control system is altered in subjects with interstitial cystitis. J Urol. 2014;191(2):364–70.
Seth A, Teichman JMH. Differences in the clinical presentation of interstitial cystitis/painful bladder syndrome in patients with or without sexual abuse history. J Urol. 2008;180:2029–33.
Clauw DJ, Schmidt M, Radulovic D, Singer A, Katz P, Bresette J. The relationship between fibromyalgia and interstitial cystitis. J Psychiatr Res. 1997;31:125–31.
Sanses T, McCabe P, Zhong L, et al. Sensory mapping of pelvic dermatomes in women with interstitial cystitis/bladder pain syndrome. Neurourol Urodyn. 2018;37:458–65.
Warren JW, Langenberg P, Greenberg P, Diggs C, Jacobs S, Wesselmann U. Sites of pain from interstitial cystitis/painful bladder syndrome. J Urol. 2008;180:1373–7.
Kindler LL, Bennett RM, Jones KD. Central sensitivity syndromes: mounting pathophysiologic evidence to link fibromyalgia with other common chronic pain disorders. Pain Manag Nurs. 2011;12(1):15–24.
Martínez-Martínez L-A, Mora T, Vargas A, Fuentes-Iniestra M, Martínez-Lavín M. Sympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis. J Clin Rheumatol. 2014;20(3):146–50.
Adams LM, Turk DC. Psychological factors and central sensitivity syndromes. Curr Rheumatol Rev. 2015;11(2):96–108.
Jutzeler CR, Curt A, Kramer JL. Relationship between chronic pain and brain reorganisation after deafferentation: a systematic review of functional MRI findings. Neuroimage Clin. 2015;9:599–606.
Neblett R, Hartzell MM, Cohen H, Mayer TG, Williams M, Choi YH. Ability of the central sensitization inventory to identify central sensitivity syndromes in an outpatient chronic pain sample. Clin J Pain. 2014;31(4):323–32.
Jensen TS, Finnerup NB. Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. Lancet Neurol. 2014;13(9):924–35.
Matsuda M, Huh Y, Ji R. Roles of inflammation, neurogenic inflammation, and neuroinflammation in pain. J Anesth. 2019;33(1):131–9.
Aguggia M, Saracco MG, Cavallini M, Bussone G, Cortelli P. Sensitization and pain. Neurol Sci. 2013;34(Suppl 1):S37–40.
Smart KM, Blake C, Staines A, Thacker S, Doody C. Mechanisms-based classifications of musculoskeletal pain: part 1 of 3: symptoms and signs of central sensitisation in patients with low back (+/− leg) pain. Man Ther. 2012;17(4):336–44.
Peters KM, Killinger KA, Mounayer MH, Boura JA. Are ulcerative and non-ulcerative interstitial cystitis/painful bladder syndrome 2 distinct diseases? A study of coexisting conditions. Urology. 2011;78:301–8.
Akiyama Y. Biomarkers in interstitial cystitis/bladder pain syndrome with and without Hunner Lesions: a review and future perspectives. Diagnostic. 2021;11(2):2238.
Warren JW, Howard FM, Cross RK, et al. Antecedent nonbladder syndromes in case-control study of interstitial cystitis/painful bladder syndrome. Urology. 2009;73:52–7.
Molokie RE, Wang ZJ, Yao Y, et al. Sensitivities to thermal and mechanical stimuli: adults with sickle cell disease compared to healthy, pain-free African American controls. J Pain. 2020;21(9–10):957–67.
Yarnitsky D, Bouhassira D, Drewes AM, et al. Recommendations on practice of conditioned pain modulation (CPM) testing. Eur J Pain. 2015;19(6):805–6.
Granovsky Y. Conditioned pain modulation: a predictor for development and treatment of neuropathic pain. Curr Pain Headache Rep. 2013;17(9):361.
Bourke JH, Wodehouse T, Clark LV, et al. Central sensitisation in chronic fatigue syndrome and fibromyalgia; a case control study. J Psychosom Res. 2021;150:110624.
Hamid P, Malik BH, Hussain ML. Noninvasive transcranial magnetic stimulation (TMS) in chronic refractory pain: a systematic review. Cureus. 2019;11(10):e6019.
Harte SE, Harris RE, Claw DJ. Neurobiol central sensitisation. J Appl Biobehav Res. 2018;23:e12137.
Acknowledgements
The authors would like to thank Thomas Arnold for his help in the original literature search.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
S.K.: lead author, data collection and analysis, manuscript writing; I.O.: second author, data collection and analysis, manuscript writing; H.H.: reviewer, manuscript editing.
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Additional information
Handling Editor: Tamara Serdinšek
Editor in Chief: Kaven Baessler
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Knox, S., Offiah, I. & Hashim, H. Evaluation of Central Sensitisation in Bladder Pain Syndrome: A Systematic Review. Int Urogynecol J (2024). https://doi.org/10.1007/s00192-024-05793-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00192-024-05793-5