Abstract
Introduction and hypothesis
Data from a large US population-based, cross-sectional, epidemiological study (the EpiNP Study) were used to assess the symptoms and bother experienced by women with nocturnal polyuria (NP).
Methods
Consenting participants recruited from an online panel completed the baseline EpiNP survey online (Lower Urinary Tract Symptoms Tool and urological comorbidities). All reporting ≥2 voids/night and a random sample of 100 respondents, each reporting 0 or 1 void/night were asked to complete a 3-day web-based bladder diary recording time, volume, and urgency rating of each void. NP was calculated by the proportion of urine production that occurred during nocturnal hours using a Nocturnal Polyuria Index (NPI33) threshold of >0.33 or nocturnal urine production of >90 ml/h (NUP90). The frequency of participants reporting LUTS and bother was determined by age and NP: idiopathic NP, NP associated with overactive bladder (NPOAB), NP associated with comorbidities (NPCom), and no NP (did not meet NP criteria).
Results
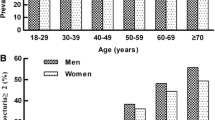
A total of 5,290 women completed the baseline survey. Mean age (range) was 54.9 (30–95) years; 1,841 (34.8%) reported ≥2 nocturnal voids. The prevalence of LUTS increased across the lifespan; however, bother associated with each LUTS decreased with increasing age. The percentage of women rating bother by nocturia episodes ≥2 “> somewhat” ranged from 40.3% to 68.3%, with bother ratings highest in the NPOAB and No NP groups.
Conclusions
NP is prevalent in women with considerable bother and is often associated with other urinary symptoms. Multifactorial causes and potential treatments of NP should be considered, particularly at a later age.


Similar content being viewed by others
References
Hashim H, Blanker MH, Drake MJ, Djurhuus JC, Meijlink J, Morris V, et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn. 2019;38(2):499–508.
Andersson F, Anderson P, Holm-Larsen T, Piercy J, Everaert K, Holbrook T. Assessing the impact of nocturia on health-related quality-of-life and utility: results of an observational survey in adults. J Med Econ. 2016;19(12):1200–6.
Asplund R, Henriksson S, Johansson S, Isacsson G. Nocturia and depression. BJU Int. 2004;93(9):1253–6.
Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10(5):540–8.
Hafner M, Andersson FL, Burtea T, van Stolk C, Whitmore M, Yerushalmi E, et al. Assessing the burden of nocturia in the workplace: the associations between nocturnal voiding, subjective well-being, work engagement and productivity. J Med Econ. 2020;23(9):994–1003.
Zumrutbas AE, Bozkurt AI, Alkis O, Toktas C, Cetinel B, Aybek Z. The prevalence of nocturia and nocturnal polyuria: can new cutoff values be suggested according to age and sex? Int Neurourol J. 2016;20(4):304–10.
Baines G, Da Silva AS, Cardozo L, Bach F, Parsons M, Robinson D, et al. Defining nocturnal polyuria in women. Neurourol Urodyn. 2021;40(1):265–71.
Monaghan TF, Kavoussi AM, Agudelo CW, Rahman SN, Michelson KP, Bliwise DL, et al. Nocturnal urine production in women with global polyuria. Int Neurourol J. 2020;24(3):270–7.
Weiss JP, Bosch JLHR, Chapple CR, Bacci ED, Simeone JC, Rosenberg MT, Mueller ER, Andersson FL, Juul K, Chughtai B, Coyne KS. The prevalence of nocturnal polyuria in the United States: results from the epidemiology of nocturnal polyuria study. Eur Urol Focus. 2022;8(5):1415–23. https://doi.org/10.1016/j.euf.2021.12.016.
Van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, et al. The standardization of terminology in nocturia: report from the standardization subcommittee of the International Continence Society. BJU Int. 2002;90:11–5.
Blanker MH, Bernsen RM, Bosch JR, Thomas S, Groeneveld FP, Prins A, et al. Relation between nocturnal voiding frequency and nocturnal urine production in older men: a population-based study. Urology. 2002;60(4):612–6.
Van Doorn B, Blanker MH, Kok ET, Westers P, Bosch JR. Prevalence, incidence, and resolution of nocturnal polyuria in a longitudinal community-based study in older men: the Krimpen study. Eur Urol. 2013;63(3):542–7.
Chapple CR, Rosenberg MT, Mueller ER, Chughtai B, Weiss JP, Juul K, Brooks AB, Bacci ED, Andersson FL, Coyne KS, Bosch JR. The patient burden of nocturnal polyuria in the United States: results from the epidemiology of nocturnal polyuria (EpiNP) study. Neurourol Urodyn. 2023. https://doi.org/10.1002/nau.25126.
Coyne KS, Barsdorf AI, Thompson C, Ireland A, Milsom I, Chapple C, et al. Moving towards a comprehensive assessment of lower urinary tract symptoms (LUTS). Neurourol Urodyn. 2012;31(4):448–54.
Bosch J, Chapple CR, Mueller ER, et al. Differences in the prevalence of nocturnal polyuria in the US by definition: results from the Epidemiology of Nocturnal Polyuria Study. J Urol. 2022;208(1):144–54.
US Census Bureau. 2017 American community survey single-year estimates 2018. Available from: https://www.census.gov/newsroom/press-kits/2018/acs-1year.html.
Brunner A, Riss P. Nocturia in women. Maturitas. 2011;70(1):16–21.
Hsu A, Nakagawa S, Walter LC, Van Den Eeden SK, Brown JS, Thom DH, et al. The burden of nocturia among middle-aged and older women. Obstet Gynecol. 2015;125(1):35.
Milsom I. Lower urinary tract symptoms in women. Curr Opin Urol. 2009;19(4):337–41.
Bing MH, Moller LA, Jennum P, Mortensen S, Skovgaard LT, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60–80 years. BJU Int. 2006;98(3):599–604.
Drake NL, Flynn MK, Romero AA, Weidner AC, Amundsen CL. Nocturnal polyuria in women with overactive bladder symptoms and nocturia. Am J Obstet Gynecol. 2005;192(5):1682–6.
Denys MA, Decalf V, Kumps C, Petrovic M, Goessaert AS, Everaert K. Pathophysiology of nocturnal lower urinary tract symptoms in older patients with urinary incontinence. Int J Urol. 2017;24(11):808–15.
Goessaert AS, Krott L, Hoebeke P, Vande Walle J, Everaert K. Diagnosing the pathophysiologic mechanisms of nocturnal polyuria. Eur Urol. 2015;67(2):283–8.
Everaert K, Herve F, Bosch R, Dmochowski R, Drake M, Hashim H, et al. International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourol Urodyn. 2019;38(2):478–98.
Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211–7.
Acknowledgements
Evidera received funding from Ferring Pharmaceuticals A/S for this project. The authors thank the following Evidera employees: Anne Brooks, BS, for providing project management support during the study; Jun Chen, MS, for conducting the analyses; and Ann Yue, MS, for statistical guidance on the weighting procedures.
Funding
Ferring Pharmaceuticals A/S.
Author information
Authors and Affiliations
Contributions
E.R. Mueller, J.P. Weiss, J.L.H. Ruud Bosch, B. Chughtai, M.T. Rosenberg, F.L. Andersson, K. Juul, C.R. Chapple: study design, data review and interpretation, and manuscript writing; E.D. Bacci, J.C. Simeone, K.S. Coyne: study design, data collection, data analysis, review and interpretation, and manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
Elizabeth R. Mueller is a consultant to Ferring Pharmaceuticals, Inc., Butler Snow Pharmaceutical, Ethicon (legal consultation), and UpToDate (author royalties). Jeffrey P. Weiss is a consultant to Ferring Pharmaceuticals, Inc., and the Institute for Bladder and Prostate Research. J.L.H. Ruud Bosch is a consultant to Ferring Pharmaceuticals, Inc. Bilal Chughtai is a consultant to Ferring Pharmaceuticals, Inc., Boston Scientific, Olympus, Medi-Tate, Medeonbio, and Urovant. Matt T. Rosenberg is a consultant to Ferring Pharmaceuticals, Inc., Astellas, Urovant, and Sunovion. Karin S. Coyne and Elizabeth D. Bacci are employed by Evidera, and Jason Simeone was employed at Evidera while the study was being conducted, receiving funding from Ferring Pharmaceuticals, Inc. Fredrik L. Andersson and Kristian Juul are employed by Ferring Pharmaceuticals. Christopher R. Chapple reports disclosures as follows: speaker for Allergan; author for Astellas Pharma; author and consultant to Ferring Pharmaceuticals, Inc., and consultant to Proverum, Symimetic, and Urovant Sciences.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mueller, E.R., Weiss, J.P., Bosch, J.L.H.R. et al. Nocturnal polyuria in women: results from the EpiNP study. Int Urogynecol J 34, 1743–1751 (2023). https://doi.org/10.1007/s00192-022-05432-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05432-x