Abstract
Importance
Robotic assistance in pelvic organ prolapse surgery can improve surgeon ergonomics and instrument dexterity compared with traditional laparoscopy but at increased costs.
Objective
To compare total costs for robotic-assisted sacrocolpopexy (RSC) between two robotic platforms at an academic medical center.
Methods
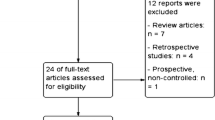
Retrospective cohort of Senhance (Ascensus) RSC between 1/1/2019 and 6/30/21 who were matched 2:1 with DaVinci (Intuitive) RSC. Primary outcome was total costs to hospital system; secondarily we evaluated cost sub-categories. Purchase costs of the robotic systems were not included. T-test, chi-square, and Fisher’s exact tests were used. A multivariable linear regression was performed to model total costs adjusting for potential confounders.
Results
The matched cohort included 75 subjects. The 25 Senhance and 50 DaVinci cases were similar overall, with mean age 60.5 ± 9.7, BMI 27.9 ± 4.7, and parity 2.5 ± 1.0. Majority were white (97.3%) and postmenopausal (86.5%) with predominantly stage III prolapse (64.9%). Senhance cases had longer OR times (Δ = 32.1 min, p = 0.01). There were no differences in concomitant procedures, intraoperative complications, or short-term postoperative complications between platforms (all p > 0.05). On univariable analysis, costs were similar (Senhance $5368.31 ± 1486.89, DaVinci $5741.76 ± 1197.20, p = 0.29). Cost subcategories (medications, supplies, etc.) were also similar (all p > 0.05). On multivariable linear regression, total cost was $908.33 lower for Senhance (p = 0.01) when adjusting for operative time, estimated blood loss, concomitant mid-urethral sling, and use of the GelPoint mini port system.
Conclusions
Despite longer operating times, total cost of robotic-assisted sacrocolpopexy was significantly lower when using the Senhance compared to the DaVinci system.
Similar content being viewed by others
References
Freeman RM, Pantazis K, Thomson A, et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013;24(3):377–84. https://doi.org/10.1007/S00192-012-1885-X.
Coolen ALWM, van Oudheusden AMJ, Mol BWJ, van Eijndhoven HWF, Roovers JPWR, Bongers MY. Laparoscopic sacrocolpopexy compared with open abdominal sacrocolpopexy for vault prolapse repair: a randomised controlled trial. Int Urogynecol J. 2017;28(10):1469–79. https://doi.org/10.1007/S00192-017-3296-5/TABLES/5.
Miller K, Benden M, Pickens A, Shipp E, Zheng Q. Ergonomics principles associated with laparoscopic surgeon injury/illness. Hum Factors. 2012;54(6):1087–92. https://doi.org/10.1177/0018720812451046.
Wee IJY, Kuo LJ, Ngu JCY. A systematic review of the true benefit of robotic surgery: Ergonomics. Int J Med Robot. 2020;16(4). https://doi.org/10.1002/RCS.2113.
Tarr ME, Brancato SJ, Cunkelman JA, Polcari A, Nutter B, Kenton K. Comparison of postural ergonomics between laparoscopic and robotic sacrocolpopexy: a pilot study. J Minim Invasive Gynecol. 2015;22(2):234–8. https://doi.org/10.1016/J.JMIG.2014.10.004.
Sinha R, Sanjay M, Rupa B, Kumari S. Robotic surgery in gynecology. J Minim Access Surg. 2015;11(1):50–9. https://doi.org/10.4103/0972-9941.147690.
Elliott CS, Hsieh MH, Sokol ER, Comiter C, v. Payne CK, Chen B. Robot-assisted versus open sacrocolpopexy: a cost-minimization analysis. J Urol. 2012;187(2):638–43. https://doi.org/10.1016/J.JURO.2011.09.160.
Paraiso MFR, Jelovsek JE, Frick A, Chen CCG, Barber MD. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol. 2011;118(5):1005–13. https://doi.org/10.1097/AOG.0b013e318231537c.
Anger JT, Mueller ER, Tarnay C, et al. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014;123(1):5–12. https://doi.org/10.1097/AOG.0000000000000006.
Sassani JC, Clark SG, McGough CE, Shepherd JP, Bonidie M. Sacrocolpopexy experience with a novel robotic surgical platform. Int Urogynecol J. 2022. Published online. https://doi.org/10.1007/S00192-022-05155-Z.
Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open. 2020;3(1):e1918911. https://doi.org/10.1001/JAMANETWORKOPEN.2019.18911.
Bodenheimer T. High and rising health care costs. Part 1: seeking an explanation. Ann Intern Med. 2005;142(10):847–54. https://doi.org/10.7326/0003-4819-142-10-200505170-00010.
Coussons H, Feldstein J, McCarus S. Senhance surgical system in benign hysterectomy: A real-world comparative assessment of case times and instrument costs versus da Vinci robotics and laparoscopic-assisted vaginal hysterectomy procedures. Int J Med Robot. 2021;17(4):e2261. https://doi.org/10.1002/RCS.2261.
Asensus Surgical building bridge from laparoscopy to robotic surgery — BioTuesdays. Accessed June 6, 2022. https://biotuesdays.com/2021/07/20/asensus-surgical-building-bridge-from-laparoscopy-to-robotic-surgery/.
Luo G, Liao D, Lin W, Chen L, Chen X, Yao D. Cost analysis of supply chain management of Da Vinci surgical instruments: a retrospective study. Technol Health Care. 2022:1–9. Published online May 20. https://doi.org/10.3233/THC-213563.
Sanchez A, Herrera L, Teixeira A, et al. Robotic surgery: financial impact of surgical trays optimization in bariatric and thoracic surgery. J Robot Surg. 2022. Published online. https://doi.org/10.1007/S11701-022-01412-X.
Author information
Authors and Affiliations
Contributions
SGC: concept, design, analysis, writing; JS: study design, analysis, writing; JCS: study design, analysis, writing; MB: concept, design, analysis, writing
This work was presented at the American Urogynecologic Society/International Urogynecologic Association Scientific Meeting held June 14–18, 2022 in Austin, TX.
Corresponding author
Ethics declarations
Conflicts of interest
SGC reports no conflicts of interest. JS reports no conflicts of interest. JCS reports no conflicts of interest. MB serves as a consultant for proctoring for Intuitive Surgical.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 18 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Glass Clark, S., Shepherd, J.P., Sassani, J.C. et al. Surgical cost of robotic-assisted sacrocolpopexy: a comparison of two robotic platforms. Int Urogynecol J 34, 87–91 (2023). https://doi.org/10.1007/s00192-022-05391-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05391-3