Abstract
Background and hypothesis
Pelvic organ prolapse (POP) is a very common and distressing problem that affects women’s quality of life. This systematic review aimed to investigate the association of the dimensions of the genital hiatus and levator hiatus at rest and Valsalva with POP.
Methods
The Cochrane Library, PubMed, Scopus, Embase and Web of Science were searched on 25 April 2020. All data were analyzed using Review Manager 5.3.
Results
Of the 1288 papers reviewed, 21 (n = 5145: 2909 women with POP and 2236 controls) were considered for meta-analysis. Compared with the normal pelvic floor group, the urogenital hiatus size in the POP group was significantly higher at rest (mean difference: 0.49; 95% CI: [0.43, 0.55], P < 0.00001) and at Valsalva (mean difference: 0.79; 95% CI: [0.70, 0.89], P < 0.00001). Also, the levator ani hiatus size in the POP group was significantly higher at rest (mean difference: 0.52, 95% CI: [0.25, 0.78], P < 0.0001) and at Valsalva (mean difference: 1.01; 95% CI: [0.73,1.28], P < 0.00001) compared with that in the normal pelvic floor group.
Conclusion
This systematic review showed that the sizes of the urogenital hiatus and levator ani hiatus and area of the levator hiatus in the POP group were significantly higher than those in the normal pelvic floor groups in both positions (rest or Valsalva maneuver). Also, in the POP group, the levator hiatus length at rest was significantly lower than that in the Valsalva maneuver.









Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available by the corresponding author.
References
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194(5):1455–61.
Iglesia CB, Smithling KR. Pelvic organ prolapse. Am Fam Physician. 2017;96(3):179–85.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26(11):1559–73.
Lamblin G, Delorme E, Cosson M, Rubod C. Cystocele and functional anatomy of the pelvic floor: review and update of the various theories. Int Urogynecol J. 2016;27(9):1297–305.
Arenholt LTS, Pedersen BG, Glavind K, Glavind-Kristensen M, DeLancey JOL. Paravaginal defect: anatomy, clinical findings, and imaging. Int Urogynecol J. 2017;28(5):661–73.
Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol. 2006;195(6):1837–40.
Summers A, Winkel LA, Hussain HK, DeLancey JO. The relationship between anterior and apical compartment support. Am J Obstet Gynecol. 2006;194(5):1438–43.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2 Pt 1):295–302.
Gowda SN, Bordoni B. Anatomy, abdomen and pelvis, levator ani muscle. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JOL, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Berek JS. Berek & Novak’s Gynecology, 15th ed., chapter 27; Pelvic organ prolapse. Wolters Kluwer; 2012. pp. 1232.
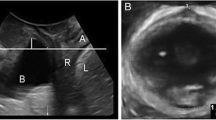
Dietz H, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25(6):580–5.
Dietz HP, Severino M, Kamisan Atan I, Shek KL, Guzman Rojas R. Warping of the levator hiatus: how significant is it? Ultrasound Obstet Gynecol. 2016;48(2):239–42.
Berger MB, Kolenic GE, Fenner DE, Morgan DM, DeLancey JOL. Structural, functional, and symptomatic differences between women with rectocele versus cystocele and normal support. Am J Obstet Gynecol. 2018;218(5):510.e1–.e8.
Athanasiou S, Chaliha C, Hobson P, Salvatore S, Khullar V, Cardozo L. Direct imaging of the pelvic floor muscles using two-dimensional ultrasound: a comparison of women with urogenital prolapse versus controls. BJOG. 2007;114:882–8.
Delancey JO, Hurd WW. Size of the urogenital hiatus in the levator ani muscles in normal women and women with pelvic organ prolapse. Obstet Gynecol. 1998;91(3):364–8.
Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. Bjog. 2008;115(8):979–84.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Handler AKJ, Peacock N. In: Reducing racial/ethnic disparities in reproductive and perinatal outcomes: the evidence from population-based interventions: methodological approach to assessing the evidence: Springer Science + Business Media, LLC.; 2011.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
Chen L, Lisse S, Larson K, Berger M, Ashton-Miller J, DeLancey J. Structural failure sites in anterior vaginal wall prolapse: identification of a collinear triad. Obstet Gynecol. 2016;128:1.
Dunivan GC, Lyons KE, Jeppson PC, Ninivaggio CS, Komesu YM, Alba FM, et al. Pelvic organ prolapse stage and the relationship to genital hiatus and perineal body measurements. Female Pelvic Med Reconstr Surg. 2016;22(6):497–500.
Handa VL, Blomquist JL, Carroll M, Roem J, Muñoz A. Longitudinal changes in the genital hiatus preceding the development of pelvic organ prolapse. Am J Epidemiol. 2019;188(12):2196–201.
Hoyte L, Schierlitz L, Zou K, Flesh G, Fielding J. Two- and 3-dimensional MRI comparison of levator ani structure, volume, and integrity in women with stress incontinence and prolapse. Am J Obstet Gynecol. 2001;185:11–9.
Hsu Y, Summers A, Hussain H, Guire K, DeLancey J. Levator plate angle in women with pelvic organ prolapse compared to women with normal support using dynamic MR imaging. Am J Obstet Gynecol. 2006;194:1427–33.
Lewicky-Gaupp C, Yousuf A, Larson KA, Fenner DE, Delancey JOL. Structural position of the posterior vagina and pelvic floor in women with and without posterior vaginal prolapse. Am J Obstet Gynecol. 2010;202(5):497.e1-.e6.
Nandikanti L, Sammarco AG, Chen L, Ashton-Miller JA, DeLancey JO. Levator bowl volume during straining and its relationship to other levator measures. Int Urogynecol J. 2019;30(9):1457–63.
Rostaminia G, Peck JD, Quiroz LH, Shobeiri SA. Characteristics associated with pelvic organ prolapse in women with significant levator ani muscle deficiency. Int Urogynecol J. 2016;27(2):261–7.
Sammarco AG, Nandikanti L, Kobernik EK, Xie B, Jankowski A, Swenson CW, et al. Interactions among pelvic organ protrusion, levator ani descent, and hiatal enlargement in women with and without prolapse. Am J Obstet Gynecol. 2017;217(5):614.e1-.e7.
Visco AG, Wei JT, McClure LA, Handa VL, Nygaard IE, Pelvic Floor Disorders N. Effects of examination technique modifications on pelvic organ prolapse quantification (POP-Q) results. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(2):136–40.
Sánchez-Ferrer ML, Moya-Jiménez LC, Mendiola J. Comparison of the anogenital distance and anthropometry of the perineum in patients with and without pelvic organ prolapse. Actas Urol Esp. 2016;40(10):628–34.
Sánchez-Ferrer ML, Prieto-Sánchez MT, Moya-Jiménez C, et al. Anogenital Distance and Perineal Measurements of the Pelvic Organ Prolapse (POP) Quantification System. J Vis Exp. 2018;(139):57912.
Li R, Song Y, Ma M. Relationship between levator ani and bony pelvis morphology and clinical grade of prolapse in women. Clin. Anat. 2015;28:813–9.
Wen L, Zhang J, Zeng S, Zhou Q. Using Z-scores to evaluate levator hiatal dimensions with four-dimensional translabial ultrasound. J Obstet Gynaecol Res. 2017;43(12):1840–7.
Handa V, Blomquist J, Roem J, Muñoz Á, Dietz H. Levator morphology and strength after obstetric avulsion of the levator ani muscle. Female Pelvic Med Reconstr Surg. 2018;26:1.
Vasconcelos Neto JA, Vasconcelos CTM, Regadas SMM, Bezerra LRPS, Lustosa KA, Karbage SAL. Clinical impact of bowel symptoms in women with pelvic floor disorders. Int Urogynecol J. 2017;28(9):1415–20.
Majida M, Braekken I, Bø K, Benth J, Engh M. Anterior but not posterior compartment prolapse is associated with levator hiatus area: a three- and four-dimensional transperineal ultrasound study. BJOG. 2011;118:329–37.
Huang WC, Yang SH, Yang JM. Clinical importance and surgical outcomes of green type III cystocele in women with anterior vaginal prolapse. J Ultrasound Med. 2015;12月 1;34(12):2279–85.
Kahn MA, Breitkopf CR, Valley MT, Woodman PJ, O'Boyle AL, Bland DI, et al. Pelvic organ support study (POSST) and bowel symptoms: straining at stool is associated with perineal and anterior vaginal descent in a general gynecologic population. Am J Obstet Gynecol. 2005;192(5):1516–22.
Swift S, Woodman P, O'Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806.
Volloyhaug I, Wong V, Shek KL, Dietz HP. Does levator avulsion cause distension of the genital hiatus and perineal body? Int Urogynecol J. 2013;24(7):1161–5.
Lowder JL, Oliphant SS, Shepherd JP, Ghetti C, Sutkin G. Genital hiatus size is associated with and predictive of apical vaginal support loss. Am J Obstet Gynecol. 2016;214(6):718.e1–8.
Lee S-L, Tan E, Khullar V, Gedroyc W, Darzi A, Yang G-Z. Physical-based statistical shape modeling of the levator ani. IEEE Trans Med Imaging. 2009;28(6):926–36.
Dietz HP, Shek C, De Leon J, Steensma AB. Ballooning of the levator hiatus. Ultrasound Obstet Gynecol. 2008;31(6):676–80.
Tukey JW. Exploratory data analysis. Reading, Mass: Addison-Wesley Pub. Co; 1977.
Handa VL, Roem J, Blomquist JL, Dietz HP, Muñoz A. Pelvic organ prolapse as a function of levator ani avulsion, hiatus size, and strength. Am J Obstet Gynecol. 2019;221(1):41.e1-.e7.
Nandikanti L, Sammarco AG, Chen L, Ashton-Miller JA, DeLancey JO. Levator bowl volume during straining and its relationship to other levator measures. Int Urogynecol J. 2019;30(9):1457–63.
Acknowledgments
We thank all authors of the original studies who responded to our requests for data or clarifications.
Author information
Authors and Affiliations
Contributions
Study conception and design: SHF and MI.
Search: MZ.
Screening: SHF, ZM.
Data extraction: SHF, ZM.
Quality assessment: SHF, FSH, ZM.
Writing the paper: SHF, MI, MB, FSH.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Siahkal, S.F., Iravani, M., Mohaghegh, Z. et al. Investigating the association of the dimensions of genital hiatus and levator hiatus with pelvic organ prolapse: a systematic review. Int Urogynecol J 32, 2095–2109 (2021). https://doi.org/10.1007/s00192-020-04639-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04639-0