Abstract
Introduction and hypothesis
Urinary incontinence (UI) is prevalent among women, including young women (18–30 years old). This article aims to explore the prevalence of UI, as well as toileting behaviors and other factors that are associated with UI, in female college students in central China.
Methods
We used convenience sampling to recruit 1000 students from five institutions of higher education. We distributed pencil-and-paper questionnaires to obtain demographic, environmental, and general health information, including whether UI was present or not, and information regarding toileting behaviors used by the respondents.
Results
Most students, n = 929, responded to the questionnaire. Their ages ranged from 18 to 26 years old (average: 20.5 ± 1.6); 23.6% of these respondents reported UI, 52.7% often/always worried about public toilet cleanliness, and 25.3% often/always delayed emptying their bladder when they were busy. Respondents who were between 21 and 26 years old had a lower probability of UI (odds ratio [OR] = 0.867 and 95% confidence interval [CI] = 0.771–0.975) than younger respondents (18–21 years old). Respondents who reported constipation (OR = 2.395, 95% CI = 1.494–3.839), drank alcohol (OR = 1.763, 95% CI = 1.114–2.792), often/always delayed urination (OR = 1.738, 95% CI = 1.306–2.313), and/or often/always strained to urinate (OR = 1.433, 95% CI = 1.111–1.849) had greater odds of having UI than respondents who did not have constipation or engage in these behaviors.
Conclusions
UI is prevalent in young Chinese women who are attending college. These women should be asked and given culturally appropriate information about UI and associated factors that include toileting behaviors.

Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Parden AM, Griffin RL, Hoover K, Ellington DR, Gleason JL, Burgio KL, et al. Prevalence, awareness, and understanding of pelvic floor disorders in adolescent and young women. Female Pelvic Med Reconstr Surg. 2016;22(5):346–54.
Angelini KJ, Newman DK, Palmer MH. Psychometric evaluation of the toileting behaviors: women's elimination behaviors scale in a sample of college women. Female Pelvic Med Reconstr Surg. 2019. https://doi.org/10.1097/SPV.0000000000000711.
Aoki Y, Brown HW, Brubaker L, Cornu JN, Daly JO, Cartwright R. Urinary incontinence in women. Nat Rev Dis Primers. 2017;3:17042.
Harlow BL, Bavendam TG, Palmer MH, Brubaker L, Burgio KL, Lukacz ES, et al. The prevention of lower urinary tract symptoms (PLUS) research consortium: a transdisciplinary approach toward promoting bladder health and preventing lower urinary tract symptoms in women across the life course. J Women's Health (Larchmt). 2018;27(3):283–9.
Wan X, Wu C, Xu D, Huang L, Wang K. Toileting behaviours and lower urinary tract symptoms among female nurses: a cross-sectional questionnaire survey. Int J Nurs Stud. 2016;65:1–7.
Palmer MH, Willis-Gray MG, Zhou F, Newman DK, Wu JM. Self-reported toileting behaviors in employed women: are they associated with lower urinary tract symptoms? Neurourol Urodyn. 2018;37(2):735–43.
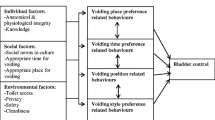
Wang K, Palmer MH. Women's toileting behaviour related to urinary elimination: concept analysis. J Adv Nurs. 2010;66(8):1874–84.
The State Council of Office of Population Censuses and Surveys. Data of the 2010 Census in China. China Statistics Press. 2012. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm.
Chinese Medical Association. Guidelines for diagnosis and treatment of chronic constipation in China. Chin J Dig. 2013;33(5):291–7.
Chinese Medical Association. Guidelines for clinical diagnosis and treatment of dysfunctional uterine bleeding. Chin J Obstet Gynecol. 2009;44(3):234–6.
Liu y WC, Sun T, Guan XM, Wang KF. Reliability and validity of the Chinese version of Women's toileting behavior scale: testing in community urinary incontinence. J Nurs Sci. 2012;27(16):78–80.
Huang L, Zhang SW, Wu SL, Ma L, Deng XH. The Chinese version of ICIQ: a useful tool in clinical practice and research on urinary incontinence. Neurourol Urodyn. 2008;27(6):522–4.
Alves JO, Luz STD, Brandao S, Da Luz CM, Jorge RN, Da Roza T. Urinary incontinence in physically active young women: prevalence and related factors. Int J Sports Med. 2017;38(12):937–41.
Zhang L, Zhu L, Xu T, Lang J, Li Z, Gong J, et al. A population-based survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. Eur Urol. 2015;68(1):97–112.
Xu D, Chen L, Wan X, Zhang Y, Liu N, Wang K. Toileting behaviour and related health beliefs among Chinese female nurses. Int J Clin Pract. 2016;70(5):416–23.
Wan XJ, Zhang Y, Liu Y, Wu C, Wang KF. Reliability and validity of the Chinese version of women’ s toileting behavior scale among female nurses. Chin J Nurs. 2014;49(7):782–5.
Da Roza T, Brandao S, Mascarenhas T, Jorge RN, Duarte JA. Urinary incontinence and levels of regular physical exercise in young women. Int J Sports Med. 2015;36(9):776–80.
van Breda HM, Bosch JL, de Kort LM. Hidden prevalence of lower urinary tract symptoms in healthy nulligravid young women. Int Urogynecol J. 2015;26(11):1637–43.
O'Halloran T, Bell RJ, Robinson PJ, Davis SR. Urinary incontinence in young nulligravid women: a cross-sectional analysis. Ann Intern Med. 2012;157(2):87–93.
Bedretdinova D, Fritel X, Panjo H, Ringa V. Prevalence of female urinary incontinence in the general population according to different definitions and study designs. Eur Urol. 2016;69(2):256–64.
Bardino M, Di Martino M, Ricci E, Parazzini F. Frequency and determinants of urinary incontinence in adolescent and young nulliparous women. J Pediatr Adolesc Gynecol. 2015;28(6):462–70.
Wu C, Wang K, Sun T, Xu D, Palmer MH. Predicting help-seeking intention of women with urinary incontinence in Jinan, China: a theory of planned behaviour model. J Clin Nurs. 2015;24(3–4):457–64.
Ninomiya S, Naito K, Nakanishi K, Okayama H. Prevalence and risk factors of urinary incontinence and overactive bladder in Japanese women. Low Urin Tract Symptoms. 2018;10(3):308–14.
Palmer MH, Newman DK. Women's toileting behaviours: an online survey of female advanced practice providers. Int J Clin Pract. 2015;69(4):429–35.
Kowalik CG, Daily A, Delpe S, Kaufman MR, Fowke J, Dmochowski RR, et al. Toileting behaviors of women—what is healthy? J Urol. 2019;201(1):129–34.
Xu D, Huang L, Gao J, Li J, Wang X, Wang K. Effects of an education program on toileting behaviors and bladder symptoms in overactive bladder patients with type 2 diabetes: a randomized clinical trial. Int J Nurs Stud. 2018;87:131–9.
Lacima G, Espuna M, Pera M, Puig-Clota M, Quinto L, Garcia-Valdecasas JC. Clinical, urodynamic, and manometric findings in women with combined fecal and urinary incontinence. Neurourol Urodyn. 2002;21(5):464–9.
Sjogren J, Malmberg L, Stenzelius K. Toileting behavior and urinary tract symptoms among younger women. Int Urogynecol J. 2017;28(11):1677–84.
Gupta NP, Kumar A, Kumar R. Does position affect uroflowmetry parameters in women? Urol Int. 2008;80(1):37–40.
Funding
The Qing Lan Project (no. 53041608) provided funding for this research to Dr. Zhou. The First Quality Bladder Health Initiative also provided funding for this study. The funding entities had no role in the study or publication of the findings.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
First co-authors: Fang Zhou, Kaikai Xue, and Yuping Liu
Rights and permissions
About this article
Cite this article
Zhou, F., Xue, K., Liu, Y. et al. Toileting behaviors and factors associated with urinary incontinence in college-aged female students in China. Int Urogynecol J 31, 961–971 (2020). https://doi.org/10.1007/s00192-019-04043-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04043-3