Abstract
Introduction and hypothesis
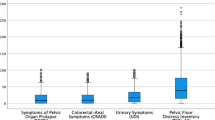
Pelvic floor disorders (PFD), including urinary incontinence, anal incontinence, and pelvic organ prolapse, are common and have a negative effect on the quality of life of women. Treatment is associated with morbidity and may not be totally satisfactory. Prevention of PFDs, when possible, should be a primary goal. The purpose of this paper is to summarise the current literature and give an evidence-based review of the prevention of PFDs
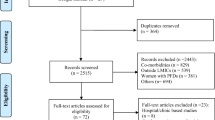
Methods
A working subcommittee from the International Urogynecological Association (IUGA) Research and Development (R&D) Committee was formed. An initial document addressing the prevention of PFDs was drafted, based on a review of the English-language literature. After evaluation by the entire IUGA R&D Committee, revisions were made. The final document represents the IUGA R&D Committee Opinion on the prevention of PFDs.
Results
This R&D Committee Opinion reviews the literature on the prevention of PFDs and summarises the findings with evidence-based recommendations.
Conclusions
Pelvic floor disorders have a long latency, and may go through periods of remission, thus making causality difficult to confirm. Nevertheless, prevention strategies targeting modifiable risk factors should be incorporated into clinical practice before the absence of symptomatology.
Similar content being viewed by others
Abbreviations
- AI:
-
Anal incontinence
- CD:
-
Caesarean delivery
- LA:
-
Levator avulsion
- OAB:
-
Overactive bladder
- OASIS:
-
Obstetric anal sphincter injuries
- PFD:
-
Pelvic floor disorder
- PFM:
-
Pelvic floor muscle
- PFMT:
-
Pelvic floor muscle training
- POP:
-
Pelvic organ prolapse
- SUI:
-
Stress urinary incontinence
- UI:
-
Urinary incontinence
- VD:
-
Vaginal delivery
References
Dieter AA, Wilkins MF, Wu JM (2015) Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol 275:380–384
Minassian VA, Drutz HP, Al-Badr A (2003) Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet 82:327–338
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123:1201–1206
American Urological Association; Society of Urodynamics, Female Pelvic Medicine, Gormley EA, Lightner DJ, Faraday M, Vasavada SP (2015) Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol 193:1572–1580
Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Muñoz A (2011) Pelvic floor disorders 5–10 years after vaginal or cesarean childbirth. Obstet Gynecol 118:777–784
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG 107:1460–1470
Gyhagen M, Bullarbo M, Nielsen T, Milsom I (2013) The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120:144–151
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120:152–160
Wilson D, Dornan J, Milsom I, Freeman R (2014) UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J 25:1449–1452
Norwegian EPINCONT Study, Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S (2003) Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med 348:900–907
Vergeldt Tineke FM, Weemhoff M, IntHout J, Kluivers KB (2015) Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J J26:1559–1573
Mous M, Muller SA, de Leeuw JW (2008) Long-term effects of anal sphincter rupture during vaginal delivery: faecal incontinence and sexual complaints. BJOG 115:234–8
Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R (2012) Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol 39:372–383
Dietz HP, Simpson JM (2007) Does delayed child-bearing increase the risk of levator injury in labour? Aust N Z J Obstet Gynaecol 47:491–495
Hijaz A, Sadeghi Z, Byrne L, Hou JC, Daneshgari F (2012) Advanced maternal age as a risk factor for stress urinary incontinence : a review of the literature. Int Urogynecol J 23:395–401
Leijonhufvud A, Lundholm C, Cnattingius S, Granath F, Andolf E, Altman D (2012) Risk of surgically managed pelvic floor dysfunction in relation to age at first delivery. Am J Obstet Gynecol 207:303.e1–303.e7
Jander C, Lyrenas S (2001) Third and fourth degree perineal tears. Predictor factors in a referral hospital. Acta Obstet Gynecol Scand 80:229–234
Beckmann, Michael M, Stock, Owen M (2013) Antenatal perineal massage for reducing perineal trauma. Cochrane Database Syst Rev 4
Brito LG, Ferreira CH, Duarte G, Nogueira AA, Marcolin AC (2015) Antepartum use of Epi-No birth trainer for preventing perineal trauma: systematic review. Int Urogynecol J 26:1429–1436
Boyle R, Hay-Smith JE, Cody JD, Morkved S (2012) Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 10:CD007471
Moore K, Dumoulin C, Bradley C, Burgio K, Chambers T, Hagen S, Hunter K, Imamaura M, Thakar R, Williams K, Vale L (2013) Adult conservative management. In: Abrams P, Cardozo L. Khouy S, Wein A (eds) Incontinence, 5th edn. IUCD, 5th International Consultation on Incontinence, Paris, pp 1101–1227
Pelaez M, Gonzalez-Cerron S, Montejo R, Barakat R (2014) Pelvic floor muscle training included in a pregnancy exercise program is effective in primary prevention of urinary incontinence: a randomized controlled trial. Neurourol Urodyn 33:67–71
Arrue M, Diez-Itza I, Ibañez L, Paredes J, Murgiondo A, Sarasqueta C (2011) Factors involved in the persistence of stress urinary incontinence from pregnancy to 2 years post partum. Int J Gynaecol Obstet 115:256–259
Pizzoferrato AC, Fauconnier A, Quiboeuf E et al (2014) Urinary incontinence 4 and 12 years after first delivery: risk factors associated with prevalence, incidence, remission, and persistence in a cohort of 236 women. Neurourol Urodyn 338:1229–1234
Jango H, Langhoff-Roos J, Rosthoj S, Sakse A (2014) Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol 210:59.e1–59.e6
Aasheim V, Nilsen BA, Lukasse M, Reinar ML (2011) Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 12:CD006672
Dahlen HG, Homer CS, Cooke M, Upton AM, Nunn R, Brodrick B (2007) Perineal outcomes and maternal comfort related to the application of perineal warm packs in the second stage of labor: a randomized controlled trial. Birth 34:282–290
Shek KL, Dietz HP (2010) Intrapartum risk factors for levator trauma. BJOG 117:1485–1492
Ashton-Miller JA, DeLancey JO (2009) On the biomechanics of vaginal birth and common sequelae. Annu Rev Biomed Eng 11:163–176
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO (2006) Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107:144–149
Gartland D, Donath S, MacArthur C, Brown SJ (2012) The onset, recurrence and associated obstetric risk factors for urinary incontinence in the first 18 months after a first birth: an Australian nulliparous cohort study. BJOG 119:1361–1369
Verheijen EC, Raven JH, Hofmeyr GJ (2009) Fundal pressure during the second stage of labour. Cochrane Database Syst Rev 4:CD00606
Lemos A, Amorim MM, Dornelas de Andrade A, de Souza AI, Cabral Filho JE, Correia JB (2015) Pushing/bearing down methods for the second stage of labour. Cochrane Database Syst Rev 10:CD009124
Elvander C, Ahlberg M, Thies-Lagergren L, Cnattingius S, Stephansson O (2015) Birth position and obstetric anal sphincter injury: a population-based study of 113 000 spontaneous births. BMC Pregnancy Childbirth 15:252
Bulchandani S, Watts E, Sucharitha A, Yates D, Ismail KM (2015) Manual perineal support at the time of childbirth: a systematic review and meta-analysis. BJOG 122:1157–1165
Carroli G, Mignini L (2009) Episiotomy for vaginal birth. Cochrane Database Syst Rev 1:CD000081
Räisänen S, Selander T, Cartwright R, Gissler M, Kramer MR, Laine K, Heinonen S (2014) The association of episiotomy with obstetric anal sphincter injury—a population based matched cohort study. PLoS One 9:e107053. doi:10.1371/journal.pone.0107053
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2014) Faecal incontinence 20 years after one birth: a comparison between vaginal delivery and caesarean section. Int Urogynecol J 25:1411–1418
Coats PM, Chan KK, Wilkins M, Beard RJ (1980) A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol 87:408–412
Kalis V, Laine K, de Leeuw JW, Ismail KM, Tincello DG (2012) Classification of episiotomy: towards a standardisation of terminology. BJOG 119:522–526
Stedenfeldt M, Pirhonen J, Blix E, Wilsgaard T, Vonen B, Oian P (2012) Episiotomy characteristics and risks for obstetric anal sphincter injuries: a case–control study. BJOG 119:724–730
O’Mahony F, Hofmeyr GJ, Menon V (2010) Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev 11:CD005455
Dietz HP (2015) Forceps: towards obsolescence or revival? Acta Obstet Gynecol Scand 94:347–351
Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen KÅ (2015) Forceps delivery is associated with increased risk of pelvic organ prolapse and muscle trauma: a cross-sectional study 16–24 years after first delivery. Ultrasound Obstet Gynecol 46:487–495
MacArthur C, Glazener C, Lancashire R, Herbison P, Wilson D (2011) Exclusive caesarean delivery and subsequent urinary and faecal incontinence: a 12 year longitudinal study. BJOG 118:1000–1007
Fernando RJ, Sultan AH, Kettle C, Thakar R (2013) Methods of repair for obstetric anal sphincter injury. Cochrane Database Syst Rev 2:CD002866
Andrews V, Thakar R, Sultan AH (2009) Structured hands-on training in repair of obstetric anal sphincter injuries (OASIS): an audit of clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 20:193–199
Browning A, Lewis A, Whiteside S (2014) Predicting women at risk for developing obstetric fistula: a fistula index?: an observational study comparison of two cohorts. BJOG 121:604–609
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) A comparison of the long-term consequences of vaginal delivery versus caesarean section on the prevalence, severity and bothersomeness of urinary incontinence subtypes: a national cohort study in primiparous women. BJOG 120:1548–1555
Term Breech Trial 3-Month Follow-up Collaborative Group, Hannah ME, Hannah WJ, Hodnett ED, Chalmers B, Kung R, Willan A, Amankwah K, Cheng M, Helewa M, Hewson S, Saigal S, Whyte H, Gafni A (2002) Outcomes at 3 months after planned cesarean vs planned vaginal delivery for breech presentation at term: the international randomized Term Breech Trial. JAMA 287:1822–1831
Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M, Gafni A, Guselle P, Helewa M, Hodnett ED, Hutton E, Kung R, McKay D, Ross S, Saigal S, Willan A (2004) Term breech trial collaborative group maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized term breech trial. Am J Obstet Gynecol 191:917–927
Handa VL, Pierce CB, Muñoz A, Blomquist JL (2015) Longitudinal changes in overactive bladder and stress incontinence among parous women. Neurourol Urodyn 34:356–361
Jelovsek JE, Piccorelli A, Barber MD, Tunitsky-Bitton E, Kattan MW (2013) Prediction models for postpartum urinary and fecal incontinence in primiparous women. Female Pelvic Med Reconstr Surg 19:110–118
Silver RM (2012) Implications of the first cesarean: perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Semin Perinatol 36:315–323
https://www.cia.gov/library/publications/the-world-factbook/rankorder/2127rank.html. Accessed 18 November 2015
Hagen S, Stark D (2011) Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev 12:CD003882. 10.1002/14651858
Hilde G, Stær-Jensen J, Siafarikas F, Ellström Engh M, Bø K (2013) Postpartum pelvic floor muscle training and urinary incontinence: a randomized controlled trial. Obstet Gynecol 122:1231–1238
Diokno AC, Sampselle CM, Herzog AR, Raghunathan TE, Hines S, Messer K, Karl C, Leite MC (2004) Prevention of urinary incontinence by behavioral modification program: a randomized, controlled trial among older women in the community. J Urol 171:1165–1171
Hagen S, Glazener C, McClurg D, Macarthus C, HerbisonP WD, Tooz-Hobson P, Bain C, Hay-Smith J, Collins M, Elders A (2014) A multicenter randomised controlled trial of a pelvic floor muscle training intervention for the prevention of pelvic organ prolapse (PREVPOL). Neurourol Urodyn 33:852–853
Bø K (2004) Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Med 34(7):451–464
Bø K (2015) Pelvic floor dysfunction, prevention and treatment in elite athletes. In: Bø K, Berghmans B, Mørkved S, van Kampen M (eds) Evidence based physical therapy for the pelvic floor—bridging science and clinical practice, 2nd edn. Elsevier, Amsterdam, pp 387–407
Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group, Sarma AV, Kanaya A, Nyberg LM, Kusek JW, Vittinghoff E, Rutledge B, Cleary PA, Gatcomb P, Brown JS (2009) Risk factors for urinary incontinence among women with type 1 diabetes: findings from the epidemiology of diabetes interventions and complications study. Urology 73:1203–1209
Prentice AM (2006) The emerging epidemic of obesity in developing countries. Int J Epidemiol 35:93–99
Vissers D, Neels H, Vermandel A, De Wachter S, Tjalma WA, Wyndaele JJ, Taeymans J (2014) The effect of non-surgical weight loss interventions on urinary incontinence in overweight women: a systematic review and meta-analysis. Obes Rev 15:610–617
Waetjen LE, Leung K, Crawford SL, Huang MH, Gold EB, Greendale GA (2013) Study of women’s health across the nation. Menopause 20:428–436
Legendre G, Ringa V, Panjo H, Zins M, Fritel X (2015) Incidence and remission of urinary incontinence at midlife: a cohort study. BJOG 122:816–824
Townsend MK, Danforth KN, Lifford KL, Rosner B, Curhan GC, Resnick NM, Grodstein F (2007) Incidence and remission of urinary incontinence in middle-aged women. Am J Obstet Gynecol 197:167.e1–167.e5
Maserejian NN, Minassian VA, Chen S, Hall SA, McKinlay JB, Tennstedt SL (2014) Treatment status and risk factors for incidence and persistence of urinary incontinence in women. Int Urogynecol J 25:775–782
Townsend MK, Matthews CA, Whitehead WE, Grodstein F (2013) Risk factors for fecal incontinence in older women. Am J Gastroenterol 108:113–119
Kudish BI, Iglesia CB, Sokol RJ, Cochrane B, Richter HE, Larson J, Hendrix SL, Howard BV (2009) Effect of weight change on natural history of pelvic organ prolapse. Obstet Gynecol 113:81–88
Thom DH, Brown JS, Schembri M, Ragins AI, Subak LL, Van Den Eeden SK (2010) Incidence of and risk factors for change in urinary incontinence status in a prospective cohort of middle-aged and older women: the reproductive risk of incontinence study in Kaiser. J Urol 184:1394–1401
Kruger J (2014) Intra-abdominal pressure changes during activities of daily living. How much is too much? IUGA Annual Meeting Abstract Video https://www.youtube.com/watch?v=ccieeVvTCNs. Accessed 17 November 2015
Chantereau P, Brieu M, Kammal M, Farthmann J, Gabriel B, Cosson M (2014) Mechanical properties of pelvic soft tissue of young women and impact of aging. Int Urogynecol J 25:1547–1553
Møller L, Lose G, Jørgensen T (2000) Risk factors for lower urinary tract symptoms in women 40 to 60 years of age. Obstet Gynecol 96:446–451
Byles J, Millar CJ, Sibbritt DW, Chiarelli P (2009) Living with urinary incontinence: a longitudinal study of older women. Age Ageing 38:333–338
Hannestad YS, Rortveit G, Daltveit AK, Hunskaar S (2003) Are smoking and other lifestyle factors associated with female urinary incontinence? the Norwegian EPINCONT study. BJOG 2003(110):247–254
Townsend MK, Resnick NM, Grodstein F (2012) Caffeine intake and risk of urinary incontinence progression among women. Obstet Gynecol 119:950–957
Jura YH, Townsend MK, Curhan GC, Resnick NM, Grodstein F (2011) Caffeine intake, and the risk of stress, urgency and mixed urinary incontinence. J Urol 185:1775–1780
The Leicestershire MRC Incontinence Study Group; Dallosso HM, McGrother CW, Matthews RJ, Donaldson MMK (2003) The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int 92:69–77
Bortolotti A, Bernardini B, Colli E, Di Benedetto P, Giocoli Nacci G, Landoni M et al (2000) Prevalence and risk factors for urinary incontinence in Italy. Eur Urol 37:30–35
Cartwright R, Srikrishna S, Cardozo L, Gonzalez J (2007) Does diet coke cause overactive bladder? a 4-way cross over trial investigating the effect of carbonated soft drinks on overactive bladder symptoms in normal volunteers. 37th Annual Meeting of the International Continence Society. Neurourol Urodyn 26:626–627
Thyssen HH, Clevin L, Olesen S, Lose G (2002) Urinary incontinence in elite female athletes and dancers. Int Urogynecol J Pelvic Floor Dysfunct 13:15–17
Nygaard IE (1997) Does prolonged high-impact activity contribute to later urinary incontinence? a retrospective cohort study of female Olympians. Obstet Gynecol 90:718–722
Shaw JM, Hamad NM, Coleman TJ, Egger MJ, Hsu Y, Hitchcock R, Nygaard IE (2014) Intra-abdominal pressures during activity in women using an intra-vaginal pressure transducer. J Sports Sci 32:1176–1185
Weir LF, Nygaard IE, Wilken J, Brandt D, Janz KF (2006) Postoperative activity restrictions: any evidence? Obstet Gynecol 107:305–309
Woodman PJ, Swift SE, O’Boyle AL, Valley MT, Bland DR, Kahn MA, Schaffer JI (2006) Prevalence of severe pelvic organ prolapse in relation to job description and socioeconomic status: a multicenter cross-sectional study. Int Urogynecol J Pelvic Floor Dysfunct 17:340–345
Sampselle CM, Harlow SD, Skurnick J, Brubaker L, Bondarenko I (2002) Urinary incontinence predictors and life impact in ethnically diverse perimenopausal women. Obstet Gynecol 100:1230–1238
Leicestershire MRC Incontinence Study Group, Dallosso HM, McGrother CW, Matthews RJ, Donaldson MM (2004) Nutrient composition of the diet and the development of overactive bladder: a longitudinal study in women. Neurourol Urodyn 23:204–210
Digesu GA, Verdi E, Cardozo L, Olivieri L, Khullar V, Colli E (2012) Phase IIb, multicenter, double-blind, randomized, placebo-controlled, parallel-group study to determine effects of elocalcitol in women with overactive bladder and idiopathic detrusor overactivity. Urology 80:48–54
Badalian SS, Rosenbaum PF (2010) Vitamin D and pelvic floor disorders in women: results from the national health and nutrition examination survey. Obstet Gynecol 115:795–803
Aydogmus S, Kelekci S, Aydogmus H, Demir M, Yilmaz B, Sutcu R (2015) Association of antepartum vitamin D levels with postpartum pelvic floor muscle strength and symptoms. Int Urogynecol J 26:1179–1184
Robinson D, Cardozo L, Milsom I, Pons ME, Kirby M, Koelbl H, Vierhout M (2014) Oestrogens and overactive bladder. Neurourol Urodyn 33:1086–1091
Gold EB, Waetjen LE, Ye J, Feng WY, Johnson WO, Greendale GA, Sampselle CM, Sternfield B, Harlow SD, Study of Women’s Health Across the Nation (SWAN) (2009) Association between menopausal transition stages and developing urinary incontinence. Obstet Gynecol 114:989–998
http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/retrieved. Accessed 26 January 2016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Tony Bazi: none; Satoru Takahashi: research funding from Astellas; Sharif Ismail: none; Kari Bø: none; Alejandra M. Ruiz-Zapata: none; Jonathan Duckett: paid travel expenses, honoraria, research funding by AMS, Astellas, Ethicon, Pfizer, EliLilly and was a consultant for Astellas and Ethicon; Dorothy Kammerer-Doak: none.
Rights and permissions
About this article
Cite this article
Bazi, T., Takahashi, S., Ismail, S. et al. Prevention of pelvic floor disorders: international urogynecological association research and development committee opinion. Int Urogynecol J 27, 1785–1795 (2016). https://doi.org/10.1007/s00192-016-2993-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-2993-9