Abstract
Purpose
To develop a novel machine learning algorithm capable of predicting TKA implant sizes using a large, multicenter database.
Methods
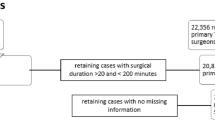
A consecutive series of primary TKA patients from two independent large academic and three community medical centers between 2012 and 2020 was identified. The primary outcomes were final tibial and femoral implant sizes obtained from an automated inventory system. Five machine learning algorithms were trained using six routinely collected preoperative features (age, sex, height, weight, and body mass index). Algorithms were validated on an independent set of patients and evaluated through accuracy, mean absolute error (MAE), and root mean-squared error (RMSE).
Results
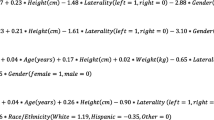
A total of 11,777 patients were included. The support vector machine (SVM) algorithm had the best performance for femoral component size(MAE = 0.73, RMSE = 1.06) with accuracies of 42.2%, 88.3%, and 97.6% for predicting exact size, ± one size, and ± two sizes, respectively. The elastic-net penalized linear regression (ENPLR) algorithm had the best performance for tibial component size (MAE 0.70, RMSE = 1.03) with accuracies of 43.8%, 90.0%, and 97.7% for predicting exact size, ± one size, and ± two sizes, respectively.
Conclusion
Machine learning algorithms demonstrated good-to-excellent accuracy for predicting within one size of the final tibial and femoral components used for TKA. Patient height and sex were the most important factors for predicting femoral and tibial component size, respectively. External validation of these algorithms is imperative prior to use in clinical settings.
Level of evidence
Case–control, III.




Similar content being viewed by others
References
TKA Sizing Prediction Application. https://orthopedics.shinyapps.io/TKASizing_AI/
Berend ME, Ritter MA, Hyldahl HC, Meding JB, Redelman R (2008) Implant migration and failure in total knee arthroplasty is related to body mass index and tibial component size. J Arthroplasty 23:104–109
Bhowmik-Stoker M, Scholl L, Khlopas A, Sultan AA, Sodhi N, Moskal JT et al (2018) Accurately predicting total knee component size without preoperative radiographs. Surg Technol Int 33:337–342
Bonnin MP, Saffarini M, Shepherd D, Bossard N, Dantony E (2016) Oversizing the tibial component in TKAs: incidence, consequences and risk factors. Knee Surg Sports Traumatol Arthrosc 24:2532–2540
Bozic KJ, Kamath AF, Ong K, Lau E, Kurtz S, Chan V et al (2015) Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res 473:2131–2138
Breiman L (2001) Random forests. Mach Learn 45:5–32
Cichos KH, Hyde ZB, Mabry SE, Ghanem ES, Brabston EW, Hayes LW et al (2019) Optimization of orthopedic surgical instrument trays: lean principles to reduce fixed operating room expenses. J Arthroplasty 34:2834–2840
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594
Cucchi D, Menon A, Compagnoni R, Ferrua P, Fossati C, Randelli P (2018) Significant differences between manufacturer and surgeon in the accuracy of final component size prediction with CT-based patient-specific instrumentation for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:3317–3324
Dyas AR, Lovell KM, Balentine CJ, Wang TN, Porterfield JR Jr, Chen H et al (2018) Reducing cost and improving operating room efficiency: examination of surgical instrument processing. J Surg Res 229:15–19
Friedman J, Hastie T, Tibshirani R (2010) Regularization paths for generalized linear models via coordinate descent. J Stat Softw 33:1–22
Friedman JH (2001) Greedy function approximation: a gradient boostingmachine. Ann Stat 29:1189–1232
Friedman JH (2002) Stochastic gradient boosting. Comput Stat Data Anal 38:367–378
Hastie T, Tibshirani R, Friedman J (2009) The elements of statistical learning data mining, inference, and prediction, 2nd edn. Springer
Hsu AR, Kim JD, Bhatia S, Levine BR (2012) Effect of training level on accuracy of digital templating in primary total hip and knee arthroplasty. Orthopedics 35:e179-183
Klemt C, Laurencin S, Uzosike AC, Burns JC, Costales TG, Yeo I et al (2021) Machine learning models accurately predict recurrent infection following revision total knee arthroplasty for periprosthetic joint infection. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06794-3
Kunze KN, Karhade AV, Sadauskas AJ, Schwab JH, Levine BR (2020) Development of machine learning algorithms to predict clinically meaningful improvement for the patient-reported health state after total hip arthroplasty. J Arthroplasty 35:2119–2123
Levine B, Fabi D, Deirmengian C (2010) Digital templating in primary total hip and knee arthroplasty. Orthopedics 33:797
Luo W, Phung D, Tran T, Gupta S, Rana S, Karmakar C et al (2016) Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J Med Internet Res 18:e323
Marmor S, Renault E, Valluy J, Saffarini M (2019) Over-voluming predicted by pre-operative planning in 24% of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27:1544–1551
Miller AG, Purtill JJ (2012) Accuracy of digital templating in total knee arthroplasty. Am J Orthop (Belle Mead NJ) 41:510–512
Polce EM, Kunze KN, Paul K, Levine BR (2021) Machine learning predicts femoral and tibial implant size mismatch for total knee arthroplasty. Arthroplast Today. https://doi.org/10.1016/j.artd.2021.01.0061-10.e12
Scholes C, Sahni V, Lustig S, Parker DA, Coolican MR (2014) Patient-specific instrumentation for total knee arthroplasty does not match the pre-operative plan as assessed by intra-operative computer-assisted navigation. Knee Surg Sports Traumatol Arthrosc 22:660–665
Schotanus MGM, Schoenmakers DAL, Sollie R, Kort NP (2017) Patient-specific instruments for total knee arthroplasty can accurately predict the component size as used peroperative. Knee Surg Sports Traumatol Arthrosc 25:3844–3848
Seaver T, McAlpine K, Garcia E, Niu R, Smith EL (2020) Algorithm based automatic templating is less accurate than manual digital templating in total knee arthroplasty. J Orthop Res 38:1472–1476
Sershon RA, Courtney PM, Rosenthal BD, Sporer SM, Levine BR (2017) Can demographic variables accurately predict component sizing in primary total knee arthroplasty? J Arthroplasty 32:3004–3008
Sershon RA, Li J, Calkins TE, Courtney PM, Nam D, Gerlinger TL et al (2019) Prospective validation of a demographically based primary total knee arthroplasty size calculator. J Arthroplasty 34:1369–1373
Siegel GW, Patel NN, Milshteyn MA, Buzas D, Lombardo DJ, Morawa LG (2015) Cost analysis and surgical site infection rates in total knee arthroplasty comparing traditional vs. single-use instrumentation. J Arthroplasty 30:2271–2274
Tang A, Yeroushalmi D, Zak S, Lygrisse K, Schwarzkopf R, Meftah M (2020) The effect of implant size difference on patient outcomes and failure after bilateral simultaneous total knee arthroplasty. J Orthop 22:282–287
Tanzer M, Makhdom AM (2016) Preoperative planning in primary total knee arthroplasty. J Am Acad Orthop Surg 24:220–230
Trickett RW, Hodgson P, Forster MC, Robertson A (2009) The reliability and accuracy of digital templating in total knee replacement. J Bone Joint Surg Br 91:903–906
van Buuren S, Groothuis-Oudshoom K (2011) mice: multivariate imputation by chained equations in R. J Stat Softw 45:1–67
Wallace SJ, Murphy MP, Schiffman CJ, Hopkinson WJ, Brown NM (2020) Demographic data is more predictive of component size than digital radiographic templating in total knee arthroplasty. Knee Surg Relat Res 32:63
Wongsak S, Kawinwonggowit V, Mulpruck P, Channoom T, Woratanarat P (2009) Accuracy of knee implants sizing predicted by digital images. J Med Assoc Thai 92(Suppl 6):S85-90
Zhang S, Lau BPH, Ng YH, Wang X, Chua W (2021) Machine learning algorithms do not outperform preoperative thresholds in predicting clinically meaningful improvements after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06642-4
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
KK: writing of initial manuscript, methodology, supervision. EP: writing of initial manuscript, data analysis. AP: data procurement. PMC, SS, BL: revision of initial manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in relation to the subject of work.
Ethical approval
This study received institutional board approval prior to commencement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kunze, K.N., Polce, E.M., Patel, A. et al. Machine learning algorithms predict within one size of the final implant ultimately used in total knee arthroplasty with good-to-excellent accuracy. Knee Surg Sports Traumatol Arthrosc 30, 2565–2572 (2022). https://doi.org/10.1007/s00167-022-06866-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06866-y