Abstract
Purpose
Fixation of soft tissue grafts with interference screws relies on the friction of the graft between the screw and the bone tunnel. The goal of this study was to precondition such grafts by mechanical compression in order to reduce anticipated and undesired viscoelastic adaptation of the graft to screw pressure. Further, the otherwise slippery graft surface was modified with impressed tricalcium phosphate granules (TCP) to improve friction and mechanical hold.
Methods
Fresh flexor digitorum tendons from young bovines were used to create bundles with a diameter of 8–9 mm and were divided into 10 groups to compare the pullout strength and bone damage in a variety of construct scenarios. Specifically, the effects of graft precompression to reduce preimplantation graft diameter were investigated. Further the effects of impressing TCP granules and/or a screw thread into the tendon surface during the compression process were studied.
Results
In sawbone tests, radial graft compression allowed for a smaller bone tunnel (7 mm), but resulted in a significantly lower pullout strength of 174 N (95% CI: 97, 250), compared with controls [315 N (204, 426)]. In contrast, TCP coated [402 N (243, 561)], screw embossed grafts [458 N (302, 614)], and the combination of TCP and embossing [409 N (274, 543)] achieved higher pullout strengths when compared to the standard technique. In porcine bone, untreated grafts using an 8 mm screw pulled out at 694 ± 93 N, significantly higher loads were required to pullout compressed grafts with or without TCP coating (870 ± 74 and 878 ± 131 N), yet fixed with a 7 mm screw.
Conclusion
Modification of the tendon graft surface has a large influence on the biomechanical performance of interference screw fixation and results in less bone damage inflicted during insertion to a smaller tunnel diameter, while simultaneously achieving superior pullout strength.
Similar content being viewed by others
Introduction
One of the most popular techniques to fixate a tendon graft for anterior cruciate ligament (ACL) reconstruction is the use of an interference screw in a bone tunnel [4, 12]. However, particularly hamstring tendon grafts do have a naturally slippery surface and will relax under mechanical compression. Therefore, interference screws of a similar diameter to the graft and drilled hole are commonly used to compensate for this effect and for local compression fractures of the bone that occur during screw insertion [6, 9, 10]. The most common mechanical failure mechanism is considered to be slippage at the tendon–screw or tendon–bone interface [1, 5, 8, 17, 19]. Therefore, it was intended to devise a method by which mechanical purchase at the graft–tunnel interface could be improved while minimizing tunnel damage. Mechanical preconditioning of the graft through compression prior to bone tunnel insertion anticipates the viscoelastic adaptation of the tissue by reduction in water content, resulting in a less viscous and more stiff elastic compressive behaviour, but without affecting tensile strength. The main hypothesis of this study was that grafts used for ACL reconstruction, if preconditioned by hydrostatic compression, could decrease the viscous behaviour once fixated in a smaller tunnel with smaller interference screws with at least equal pullout strength. A further hypothesis was that roughening the surface with impressed tricalcium phosphate (TCP) granules or embossing the pattern of a screw thread may enhance fixation strength.
Materials and methods
Graft preparation
Flexor digitorum tendons were harvested from young bovines directly after slaughter, and any muscle or connective tissue was removed before cutting to a length that would result in a bundle with dimensions of 8 or 9 mm of diameter and 45 mm length. The suitability of this graft material has been established earlier by other groups [2]. The ends of the tendon were then pinched with Vicryl USP No. 0 suture and Ethibond USP No. 0 in the suture loops. Under slight tension to the bundles, the bundles were sutured with UPS No. 0 Vicryl sutures at quarter, half and three-quarter length of the graft to finish. Once made, graft diameter was assessed with a pull-through round calliper to assure that the desired diameter was achieved. Finished grafts were stored in Ringer Lactate-soaked gauze.
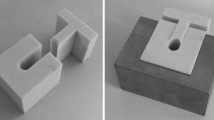
Bundles to be tested were divided into groups of either no preconditioning, inserted into a 9 mm hole fixated with either a 9 mm (control group) or an undersized 7 mm interference screw (undersized screw group), or with preconditioning using mechanical compression to achieve a 7-mm diameter graft, inserted into a 9 mm hole with a 9 mm screw (compressed group) or into a 7 mm hole with a 7 mm screw (compressed graft and small tunnel/screw group). Furthermore, 9 mm grafts were used to investigate the effect of preconditioning bundles (to 8 mm diameter) with a coating of coarse (approx. 1–3 mm diameter) granules of TCP (TCP coat group) or by pressing an 8 mm interference screw into the tendon during compression to emboss a screw thread pattern (screw emboss group) or both (combined screw emboss and TCP coat group) to subsequently fix the construct in a 8 mm hole with a 8 mm interference screw (Table 1; Fig. 1). Therefore, other than in the undersized screw group, the interference screw size matched the hole size. The hole size matched the bundle size, other than in the setting where the bundle was compressed to a smaller size (compressed group) or space was provided for the TCP granula.
Compression of bundles (compressed group) was performed with two moulds with semi-circular cross-sections to produce a compressed graft with a circular cross-sectional area. The compression protocol was also adapted for the compressed graft and small tunnel/screw group to achieve a concave cross-sectional profile of the compressed tendon. This was done by placing an 8 mm rod in an 8 mm slot and placing the tendon on top before compressing up to 10 kN at a strain rate of 1 mm/min. This was done to accommodate the interference screw, so as to reduce tunnel widening during the process of inserting tendon and screw into the drilled hole. Extending this concept further, groups VI and VII utilized a PMMA-filled interference screw to emboss a screw thread pattern into the tendon surface.
Compression was applied by a universal material testing machine (Zwick 1456, Zwick GmbH, Ulm, Germany). Compression of samples was done by initially applying a 5 N preload at a rate of 10 mm/min, at which point the sample could be shifted in the mould, to ensure the entire sample was being compressed by the load head. Load was then applied up to the peak force at a displacement rate of 1 mm/min using a creep loading protocol.
For pullout tests from porcine bone, there were three groups of five bundles each, one group (A) of 8 mm diameter without compression, inserted into an 8 mm bone tunnel, fixed with an 8 mm interference screw. In groups (B) and (C), all grafts were loaded in a custom-made compression device to emboss an interferential screw (7/28 mm Megafix©, Karl Storz) at the graft ending. Embossing was executed on the mechanical testing machine (Zwick 1456, Zwick GmbH, Ulm, Germany) with cyclical loading as described above. In group (C), grafts were covered about 50% of the surface with ß-tricalcium phosphate granules of 1–1.6 mm (Calc-i-oss©, Meissner, 41468 Neuss, Germany).
Biomechanical testing
Bone tunnels were simulated in sawbone blocks with densities of 20 and 64 gcm−3 for the trabecular and 1 mm cortical layers, respectively, with blind 7, 8 and 9 mm holes drilled to leave a minimum distance of 35 mm between holes.
Bundles were inserted to a depth of 20 mm in the prepared saw bone or porcine femoral tunnels before interference screws of 28 mm length were used to fixate the bundles. All screws were wetted before insertion and inserted until the tops were flush with the surface of the sawbone block. Once the grafts were fixated by the interference screw, the sawbone blocks with grafts inserted were submerged in Ringer Lactate overnight to allow exhibition of potential dependent viscoelastic behaviour. Following this, the exposed end of the graft was wrapped with a thin (1 cm × 5 cm) wetted piece of gauze and clamped over this point. The graft bone block construct was then tested in tensile loading at a strain rate of 0.5 mm/s until failure, and the pullout force was recorded with an accuracy of 1 N.
Tunnel enlargement
After pullout testing, the canal diameter was measured by a calliper as accurate as 0.1 mm in all sawbone blocks to determine the expansion of the bone due to the interference screw. Therefore, a roughly elliptical cross-section was assumed, allowing for direct calculation of the tunnel area through measurement of the major and minor semi-axes (Fig. 2 and equation in Fig. 2). Measurements were taken 10 mm below the surface and at the sawbone surface, representing tunnel widening of the trabecular and cortical regions, respectively.
After pullout testing, the canal diameter was measured to determine the expansion of the bone due to the interference screw. Therefore, a roughly elliptical cross-section was assumed, allowing for direct calculation of the tunnel area through measurement of the major and minor semi-axes L1 and L2 by the formula \( {\text{Area}} = \pi * L1 * L2 \)
Tests in porcine bone
To validate the results from the sawbone blocks, the same test protocol was repeated by pullout tests on 15 distal porcine femora (however, with testing 1 h after screw insertion), a well-established pullout model [15]. After freeing from soft tissue, an 8 mm hole was drilled at the anatomical site of the ACL insertion and fixed with a interferential screw of 8 mm diameter in group A and 7 mm in group B and C, respectively. Grafts were tensioned into the tunnel and fixed with an interference screw 28 mm in length, flush to the tunnel aperture. Pullout was performed after 1 h of adaptation in wet conditions in line with the insertion axis of the graft. The same precycling protocol as above was applied.
Statistical analysis
Standard statistical software (PRISM Version 5.01 for Windows; Graphpad) was used for all analyses. Values were documented as mean with their 95% confidence interval (mean (lower 95%CI, upper 95% CI). Boxplots are depicted as mean with whiskers from minimum to maximum. Mann–Whitney test was employed for intergroup comparison for normal and not normal distributed data, respectively. A subgroup of the control group was built (group Ib) where two samples where the cortical bone remained intact with pullout strengths of 510 and 631 N were excluded to investigate the effect of the cortical bone integrity on pullout performance. Significance was set at a level of P < 0.05.
Results
Pullout strength
Undersized 7 mm screws used to fixate 9 mm untreated grafts into 9 mm holes (undersized screw group) trended towards inferior mean pullout strength compared with the control (group Ia). Graft compression was successful in reducing the diameter of the bundle from 9 to 7 mm, but resulted in significantly inferior pullout strength if inserted into a 9 mm hole using a 9 mm screw (compressed group) (Table 2). Compression allowed for a smaller screw (7 mm) and a smaller bone tunnel (7 mm) to be used (compressed graft and small tunnel/screw group), however, with a significantly lower pullout strengths if compared with group Ia and trended to lower pullout forces if compared with group Ib (Table 2). Bundles coated in TCP, with or without a screw thread embossed both achieved higher pullout strengths when compared to the normal technique (Table 1). The strongest fixation technique in terms of pullout strength was with screw-embossing only (screw emboss group), which had a mean pullout force of 458 N (95% CI: 302, 614). After accounting for two samples where no cortical damage was documented (510 and 631 N—treated as control group Ib), groups V, VI, and VII were then found to be significantly superior in terms of pullout strength (Table 2 and Fig. 3).
Pullout strength of different groups described in Table 1. Graft compression was successful in reducing the diameter of the bundle from 9 to 7 mm, but resulted in significantly (asterisk) inferior pullout strength if inserted into a 9 mm hole using a 9 mm screw (compressed group). Compression allowed for a smaller screw (7 mm) and a smaller bone tunnel (7 mm) to be used (compressed graft and small tunnel/screw group), however, with a significantly lower pullout strengths if compared with group Ia. Bundles coated in TCP, with or without a screw thread embossed both achieved significantly (triangle) higher pullout strengths when compared to the normal technique (group Ib)
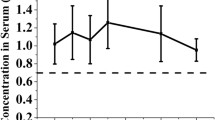
Pullout from bone
The preconditioned groups both had superior pullout strengths compared with the controls in the porcine bone model. While untreated grafts pulled out with 694 ± 93 N although a 8 mm screw was used, significantly higher loads (870 ± 74 N, P = 0.010 and 878 ± 131 N, P = 0.033) were needed to pullout the compressed grafts with or without TCP coating, respectively (Fig. 4) despite the use of only a 7 mm screw.
Tunnel enlargement
As expected, an undersized 7 mm screw (undersized screw group) caused less damage to the cortical and trabecular bone structures (P < 0.05 and n.s.) during insertion when compared to the control construct of a 9 mm screw to fixate a 9 mm graft into a 9 mm hole (control group). In the case of a compressed graft and reduced screw and hole diameters (groups III and IV), tunnel widening and cortical damage were not found to be less than in the control, where damage to both the cortical and trabecular regions was extensive at 2.5 times and 1.5 times the original diameter at the surface and trabecular regions of the bone block, respectively (Fig. 5).
Normalized change in cortical bone area (grey bars) and trabecular bone area (white bars added to the grey bars). Both, use of an undersized 7 mm screw (undersized screw group) or use of a screw embossed graft caused significantly (asterisk) less damage to the cortical bone structure when compared to the control construct of a 9 mm screw to fixate a 9 mm graft into a 9 mm hole
When a screw thread was embossed into the graft during compression (screw emboss group), the resulting imprint of the screw thread (Fig. 1) allowed for much easier insertion into the bone block and also accommodated the interference screw much better than when an 8 mm rod was used to create the concave shape (as was used in compressed graft and small tunnel/screw group). This resulted in less observed surface and internal damage to the block than was found for any of the other cases tested, particularly in regard to the cortical bone with the exception of undersized screw group (where an undersized screw was used in a 9 mm tunnel).
Discussion
The most important finding of this study was that modification of the tendon graft surface has a large influence on the biomechanical performance of interference screw fixation and results in less bone damage inflicted during insertion to a smaller tunnel diameter, while simultaneously achieving superior pullout strength.
Interference screw fixation of tendon grafts has several important advantages [3]. Firstly, the method is very straightforward and results in a relatively stiff fixation close to the joint surface. An interference screw may easily be exchanged or removed, and usually no additional surgical approach is needed. Furthermore, the surgeon gets an immediate feel for the quality of the fixation by the resistance during insertion [8, 11]. However, in combination with hamstring grafts where no bone block is used, there are inherent drawbacks of the method. One results from the naturally slippery surface of tendons, which are designed to glide in the body. Interference screw fixation, however, relies on friction of the graft against bone and screw; therefore, relatively high pressure is needed for sufficient friction and hold. Efforts have been made to enhance the friction at the interface for example by autograft bone augmentation, with, however, not yet superior fixation strengths [14]. Secondly, tendons are a viscoelastic material and will adapt and relax under compression, resulting in a reduced contact pressure within the construct, consequently resulting in decreased fixation strength. In the presented work, it was the goal to improve the use of interference screws by addressing both the tendon graft viscoelasticity by mechanical compression before implantation and the roughness of the surface by incorporating rough TCP granules into it. Without compression, TCP cement has already been described to be advantageous when added to the graft surface [13, 18].
Unexpectedly, it was found that pure compression of the tendon resulted in a thinner graft with less water content, but the resulting surface was glass-like and slippery resulting lower fixation strengths. However, if during compression a screw thread was embossed into the tendon where later the interference screw was inserted, superior pullout strength could be achieved using the same graft in a smaller bone tunnel and a smaller interference screw. Also, incorporation of TCP granules into the surface was comparably advantageous for the fixation strength of the graft. The combination of the two methods, however, did not further increase fixation strength in sawbone or porcine bone, possibly because now the tunnel wall surface represented the weakest link and the stability of which was not influenced with the proposed methods.
There are limitations in interpretation of this in vitro study. Firstly, even though the use of sawbone, porcine femora and bovine tendons [2] have been validated as suitable in vitro substitutes for cruciate ligament reconstruction testing, they of course do not fully represent the situation in man and cannot be generalized. Particularly local anatomical variations in man are certainly an influencing factor not specified here. However, due to limited availability of homogenous human tendons, the use of the animal model is justifiable, as it allowed for the development of a very standardized and consistent model. It was also not the goal to find absolute values, but to compare various techniques to each other. The fact that the relative behaviour of the methods in sawbone and porcine bone was very similar supports the potential of the presented method. Secondly, the assumption of an elliptical cross-section to estimate the tunnel size, while an acceptable approximation, could be improved upon. More accurate techniques, such as CT scanning, might potentially yield more quantitative and reliable results when determining the extent of tunnel widening.
The primary goal of this study is considered to have been achieved, as simple soft tissue graft compression made it possible to reduce the size of the required bone tunnel and to correspondingly reduce the diameter of the interference screw all while simultaneously increasing fixation strength. Although other testing modalities such as cyclic testing will be important to consider in the future, to screen for the most promising variation of the proposed concept, the applied testing setup was sufficient to answer the posed research question. Various authors have shown that it is reasonable to extrapolate form between-group comparisons in pullout strength to cyclic loading tests [7, 16]. However, others have shown that load to failure test might not reliably predict cyclic loading results [9]. The aim of this study was to investigate whether preconditioning by hydrostatic compression and/or TCP coating could decrease the viscous behaviour of the graft and allow a smaller tunnel with smaller interference screws while preserving at least an equal pullout strength. While this aim has been achieved, further research is needed to gain additional information not only regarding behaviour of compressed grafts on cyclic loading tests, but also the effect of various sizes of granula, different graft types, different bones and the behaviour in vivo.
From a biological perspective, the introduction of TCP into an ACL graft appears desirable, as it is likely to aid tendon-bone healing, due to its osteoinductive properties and due to the effective increase in contact area at the graft–tunnel interface. In further research, it will be interesting to determine the exact surface exposed to healing and the potentially favourable biological [18] implications of this in vitro mechanically thus far promising approach.
Conclusion
To achieve optimal fixation of a tendon graft in a bone tunnel with an interference screw, current techniques advocate a screw diameter of a similar diameter as the drilled hole and transplant. This is to compensate for the elastic and viscoelastic adaptation of the tendon graft and bone. The presented method of preconditioning the graft by mechanical compression with impression of TCP granules or embossing of a screw thread anticipates and apparently reduces the undesired viscoelastic adaptation to pressure. Therefore, one may reduce the bone tunnel width and inflict less bone damage, while simultaneously achieving superior pullout strength, advantages that are welcomed in many surgical procedures such as in reconstruction of a torn ACL.
References
Becker R, Voigt D, Starke C et al (2001) Biomechanical properties of quadruple tendon and patellar tendon femoral fixation techniques. Knee Surg Sports Traumatol Arthrosc 9:337–342
Donahue TL, Gregersen C, Hull ML et al (2001) Comparison of viscoelastic, structural, and material properties of double-looped anterior cruciate ligament grafts made from bovine digital extensor and human hamstring tendons. J Biomech Eng 123:162–169
Drogset JO, Strand T, Uppheim G et al (2010) Autologous patellar tendon and quadrupled hamstring grafts in anterior cruciate ligament reconstruction: a prospective randomized multicenter review of different fixation methods. Knee Surg Sports Traumatol Arthrosc 18:1085–1093
Drogset JO, Straume LG, Bjorkmo I et al (2011) A prospective randomized study of acl-reconstructions using bone-patellar tendon-bone grafts fixed with bioabsorbable or metal interference screws. Knee Surg Sports Traumatol Arthrosc 19:753–759
Fabbriciani C, Mulas PD, Ziranu F et al (2005) Mechanical analysis of fixation methods for anterior cruciate ligament reconstruction with hamstring tendon graft. An experimental study in sheep knees. Knee 12:135–138
Giurea M, Zorilla P, Amis AA et al (1999) Comparative pull-out and cyclic-loading strength tests of anchorage of hamstring tendon grafts in anterior cruciate ligament reconstruction. Am J Sports Med 27:621–625
Halewood C, Hirschmann MT, Newman S et al (2011) The fixation strength of a novel acl soft-tissue graft fixation device compared with conventional interference screws: a biomechanical study in vitro. Knee Surg Sports Traumatol Arthrosc 19:559–567
Jarvinen TL, Nurmi JT, Sievanen H (2004) Bone density and insertion torque as predictors of anterior cruciate ligament graft fixation strength. Am J Sports Med 32:1421–1429
Micucci CJ, Frank DA, Kompel J et al (2010) The effect of interference screw diameter on fixation of soft-tissue grafts in anterior cruciate ligament reconstruction. Arthroscopy 26:1105–1110
Nebelung W, Becker R, Urbach D et al (2003) Histological findings of tendon-bone healing following anterior cruciate ligament reconstruction with hamstring grafts. Arch Orthop Trauma Surg 123:158–163
Nyland J, Kocabey Y, Caborn DN (2004) Insertion torque pullout strength relationship of soft tissue tendon graft tibia tunnel fixation with a bioabsorbable interference screw. Arthroscopy 20:379–384
Colvin A, Sharma C, Parides M et al (2011) What is the best femoral fixation of hamstring autografts in anterior cruciate ligament reconstruction?: a meta-analysis. Clin Orthop Relat Res 469:1075–1081
Reigstad O, Franke-Stenport V, Johansson CB et al (2007) Improved bone ingrowth and fixation with a thin calcium phosphate coating intended for complete resorption. J Biomed Mater Res B Appl Biomater 83:9–15
Roy S, Fernhout M, Stanley R et al (2010) Tibial interference screw fixation in anterior cruciate ligament reconstruction with and without autograft bone augmentation. Arthroscopy 26:949–956
Shen PH, Lien SB, Shen HC et al (2009) Comparison of different sizes of bioabsorbable interference screws for anterior cruciate ligament reconstruction using bioabsorbable bead augmentation in a porcine model. Arthroscopy 25:1101–1107
Sim JA, Kwak JH, Yang SH et al (2009) Comparative biomechanical study of the ligament plate and other fixation devices in acl reconstruction. Int Orthop 33:1269–1274
Weimann A, Rodieck M, Zantop T et al (2005) Primary stability of hamstring graft fixation with biodegradable suspension versus interference screws. Arthroscopy 21:266–274
Wen CY, Qin L, Lee KM et al (2009) The use of brushite calcium phosphate cement for enhancement of bone-tendon integration in an anterior cruciate ligament reconstruction rabbit model. J Biomed Mater Res B Appl Biomater 89B:466–474
Zantop T, Kubo S, Petersen W et al (2007) Current techniques in anatomic anterior cruciate ligament reconstruction. Arthroscopy 23:938–947
Conflict of interest
The following authors have claimed intellectual property ownership related to the manuscript content: Mazda Farshad, Jess G. Snedeker, Dominik C. Meyer, but have no other conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farshad, M., Weinert-Aplin, R.A., Stalder, M. et al. Embossing of a screw thread and TCP granules enhances the fixation strength of compressed ACL grafts with interference screws. Knee Surg Sports Traumatol Arthrosc 20, 268–274 (2012). https://doi.org/10.1007/s00167-011-1623-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1623-9