Abstract
Purpose
Providing mechanical ventilation is challenging at supra-atmospheric pressure. The higher gas density increases resistance, reducing the flow delivered by the ventilator. A new hyperbaric ventilator (Siaretron IPER 1000) is said to compensate for these effects automatically. The aim of this bench test study was to validate the compensation, define its limits and provide details on the ventilator’s output at varied atmospheric pressures.
Methods
Experiments were conducted inside a multiplace hyperbaric chamber at 1, 2.2, 2.8 and 4 atmospheres absolute (ATA), with the ventilator connected to a test lung. Transducers were recalibrated at each ATA level. Various ventilator settings were tested in volume and pressure control modes. Measured tidal volumes were compared with theoretical predictions based on gas laws.
Results
Results confirmed the ventilator’s ability to provide compensation, but also identified its limits. The compensation range could be predicted and depended on the maximal flow attainable, decreasing linearly with increasing atmospheric pressure. With settings inside the range, tidal volumes approximated set values (mean error 10 ± 5 %). With settings outside the range, the volume was limited to the predicted maximal value calculated from maximal flow. A practical guide for clinicians is provided.
Conclusion
The IPER 1000 ventilator attempted to deliver stable tidal volume by adjusting the opening of the inspiratory valve in proportion to atmospheric pressure. Adequate compensation was observed, albeit only within a predictable range, which can be reliably predicted for each setting and ATA level combination. Setting a tidal volume outside this range can result in an unwanted decrease in minute ventilation.
Similar content being viewed by others
Introduction
Hyperbaric oxygen therapy (HBOT) is used in the treatment of several acute medical conditions, including decompression sickness, carbon monoxide poisoning and necrotizing infections [1]. In recent years, technical advances and a better understanding of mechanical ventilation under hyperbaric pressure have contributed to the increasing use of HBOT in the treatment of critically ill patients. Nevertheless, applying HBOT to mechanically ventilated patients remains challenging because of safety and technical reasons [2]. Devices used in the hyperbaric chamber must resist the crushing effect of pressurization, while electronic components must operate at low voltage to mitigate the risk of fire hazard in the oxygen-enriched environment, precluding the use of conventional ventilators [1, 3]. The higher gas density at supra-atmospheric pressure increases resistance, reducing the flow delivered by the ventilator [4, 5]. This is frequently worsened by the suboptimal performance of hyperbaric-approved ventilators [2, 5, 6].
A hyperbaric ventilator combining safety and acceptable performance, mostly in terms of sufficient and stable minute ventilation (VE), is clearly needed. Ideally, it should be portable, user friendly, with adequate alarms and various ventilation modes, notably assisted ones (as opposed to fully controlled ventilation). To our knowledge, the recently released Siaretron IPER 1000 (Siare, Bologna, Italy; distributed by Haux Life-Support, Karlsbad-Ittersbach, Germany) is the only ventilator approved for use inside the chamber that offers assisted modes of ventilation and automatic adjustment of the inspiratory valve opening to provide stable flow regardless of the ambient pressure.
The IPER 1000 has never been bench tested independently under hyperbaric pressure. This study was carried out to evaluate the performance and operational characteristics of the IPER 1000. Since this ventilator is said to compensate for the effects of increased gas density automatically, we compared the measurements obtained in supra-atmospheric conditions with theoretical calculations based on gas laws. This allowed us to (1) estimate the amount of compensation provided by the ventilator; (2) test and understand its limits; and (3) provide users with practical information about its operational range.
Materials and methods
The IPER 1000 is a portable electropneumatic ventilator, functioning with a low-tension electrical circuit and compressed medical gases. Volume-assist control (VC) and pressure-assist control (PC) modes are available, in addition to pressure support (PS). There is no integrated volume/flow monitoring (nor alarms), but the airway pressure (Paw) is displayed on a bar graph, and there is a low/high Paw alarm. The device is CE certified in accordance with European regulations, but is not yet available in the US, pending FDA approval.
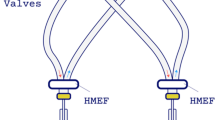
All the experiments were conducted inside a multiplace hyperbaric chamber (Haux-Starmed 2400, Haux Life-Support, Germany) at 1, 2.2, 2.8 and 4 atmospheres absolute (1 ATA = atmospheric pressure). The IPER 1000 was connected to a passive Michigan test lung (Michigan Instruments, Grand Rapids, MI, USA) using an 8-mm endotracheal tube and a double-limb circuit [7, 8]. Compliance was set at 50 ml cmH2O−1, without additional resistance. The ventilator, test lung and sensors were placed inside the chamber, while the data collecting units were kept outside for safety reasons. Four set tidal volume (V T; 250, 500, 750 and 1,000 ml) and inspiratory pressures (Pinsp; 5, 10, 15, 20 cmH2O) were tested in VC and PC, respectively, with the following settings: respiratory rate (RR) 15 cycles min−1, no inspiratory pause, positive end-expiratory pressure (PEEP) 5 cmH2O and FiO2 21 %. The inspiratory time was modified by varying the inspiratory:expiratory ratio (I:E): 1:2, 1:3, 1:4. Detailed methods are presented in the online supplement.
Theoretical predictions
Due to compression, gas density increases linearly with ambient pressure, with density being doubled at 2 ATA [2, 9]. This higher density increases resistance to gas flow. Since ventilators control flow through the proportional opening of the inspiratory valve, greater resistance results in decreased flow across the valve for a given aperture [4, 10].
The difference in gas density determines the impact on flow and hence on delivered V T. We calculated the theoretical V T predicted by the effects of gas laws only, using a volume correction factor detailed in the online supplement:
where gas ρ = gas density; x = current ATA level. Since they are linearly correlated, the ATA level can directly replace gas density in the equation.
The IPER 1000 compensates for hyperbaric pressure by adjusting the opening of the inspiratory valve in proportion to the ambient pressure. This should function until the maximal valve opening area is attained; the flow then generated dictates the upper limit of the compensation range. According to the manufacturer, the maximal flow (flowmax) at 1 ATA is 99 l min−1, and we hypothesized a direct linear decrease with increasing ATA level (e.g., 25 l min−1 at 4 ATA). We subsequently determined the predicted maximal V T attainable (V Tmax) for each experimental condition by multiplying the flowmax by the set inspiratory time. The V Tmax fixed the upper limit of the compensation range. In theory, the decline in V T should be less of an issue with PC, since the ventilator should intrinsically compensate for the decrease in flow to attain the target Pinsp [4].
Results
As predicted, peak flow was progressively limited with higher ambient pressures, decreasing linearly by a factor proportional to the ATA level, confirming our hypothesis of a predictable flowmax (Fig. 1). The area under the flowmax values delineates the range of compensation, the ventilator being unable to generate higher flow for a given ATA level. The complete results obtained in VC are displayed in Table 1. The mean error of the delivered V T was only 5 ± 4 % at 1 ATA. Performances were progressively less accurate with increasing ambient pressure, but the results can be dichotomized according to theoretical predictions of the compensation range. At supra-atmospheric pressures, for settings inside the range (i.e., under V Tmax), the V T did not decrease as predicted based on gas laws, but remained roughly stable (mean error of 10 ± 5 %), confirming adequate compensation. Conversely, with settings outside the range (bold-italic values in Table 1), the delivered V T differed widely from the set values, but were in close agreement with our predicted V Tmax (3 ± 3 %), indicating the inability of the ventilator to exceed V Tmax. As the experimental results confirmed our theoretical predictions, we produced a practical user’s guide, fixing the range of compensation of the IPER 1000 at frequently used settings (Table 2).
Changes in peak flow with increasing atmospheric pressure. The figure shows the change in measured peak flow at various flow settings and ambient pressures. The IPER 1000 maintains a stable flow despite increasing atmospheric pressure, but only up to the point where the predicted flowmax is reached. This flowmax decreased with increasing ATA level. From the flowmax values at each ATA level (99 l min−1 at 1 ATA, 45 l min−1 at 2.2 ATA, 35 l min−1 at 2.8 ATA and 25 l min−1 at 4 ATA), a schematic zone of compensation can be represented (hatched area). ATA absolute atmosphere, flowmax predicted maximal attainable flow
A progressive loss of PEEP of 2–3 cmH2O was revealed (40–60 % of the set value) for all experimental settings, without being significantly influenced by the ATA level. Importantly, an aberrant insufflation, with high delivered V T, was frequently noticed immediately after setting modifications during ventilation (e-figure 5). The results obtained in PC are detailed in the online supplement (e-table 1). In short, large discrepancies were frequently found between the measured and the predicted V T. This can be mainly attributed to the flow limitation at higher ATA levels, preventing the ventilator from attaining the target Pinsp (e-table 1 and e-figure 1).
Discussion
Our results confirmed that the IPER 1000 compensated for the greater resistance induced by higher gas density, apparently by increasing the opening of the inspiratory valve in proportion to the ATA level. However, this compensation only takes place inside an operational range, which becomes narrower at higher ATA levels. This range was shown to be reliably predicted using the theoretical flowmax for each ATA level. Users must be aware of this range to prevent an unnoticed decrease in V E, as there is no built-in volume monitoring. The practical guide presented in Table 2 might give a good estimate of the V Tmax for a given condition. Clinicians should not expect delivered V T to be higher than V Tmax. The highest attainable V E is quite low at the higher ATA levels (6.2 l min−1 at 4 ATA; 4.2 l min−1 at 6 ATA, with a 1:3 ratio), which could be insufficient for patients with moderate-high ventilatory needs.
In clinical practice, it is recommended that the IPER 1000 be used with an independent volumeter. Since results are more predictable in VC, this mode should be used preferentially, especially as predictions in PC would be even harder because of the patient’s variable respiratory mechanics. Ventilator settings should correspond to the predicted values in Table 2. If the clinical adequacy of the maximal V E is doubtful, one should consider evaluating its impact on the patient before attempting HBOT with the IPER 1000. Using a 1:2 instead of 1:3 I:E ratio increases the maximal V E, but this should be done carefully because of the risk of dynamic hyperinflation, further magnified by the relatively high resistance of the exhalation apparatus (online appendix). To limit the impact of ventilating the fixed dead space, the use of a respiratory frequency in the low range (≈10/min) along with a relatively high V T (limited by the V Tmax) should be considered, at least for higher ATA levels.
With respect to study limitations, only one ventilator unit was tested, but the concordance between predicted and measured values suggests reproducible results. Even if a systematic decrease in PEEP is supposed to occur for every set value, only one PEEP level was formally tested. Theoretical predictions were not confirmed at 6 ATA because such a depth is not possible with our chamber. Also, gas mixtures other than air, such as heliox, were not tested because their use is not approved with the IPER 1000, but wide variations in V T should be expected.
It can be appreciated that a hyperbaric environment poses a challenge for manufacturers; the alternatives to the IPER 1000 also have limitations. With monoplace chambers, the ventilator unit is kept outside of the chamber. The Sechrist 500A and the Omni-vent have been used in this context, but limited performances and capabilities (control mode only) were shown by Weaver et al. [11, 12]. For multiplace chambers, the ventilator must be placed in the enclosure, allowing manipulations by the caregivers. Most of the ventilators tested in one report have shown unacceptable performance, mainly because of insufficient V E [5]. Some older devices, such as the Monaghan 225, have also been used in the past, but technical support is now difficult with these devices [13]. Modified standard ICU ventilators have been bench tested with variable results, but none are currently approved for use in clinical practice [4]. Despite not being approved for hyperbaric use, the Impact UNI-VENT Eagle 754 ventilator was shown to provide a stable V E under various supra-atmospheric pressures [14]. The recently FDA-approved Atlantis ventilator also has generated a lot of interest, but also suffers from several drawbacks as it provides only control ventilation and is devoid of alarms, and the compensation mechanism is not in function when used in a multiplace chamber. Interestingly, a hyperbaric-compatible version of the Servo-i (Maquet, Solna, Sweden) is expected on the market by mid-2012.
Conclusion
The Siaretron IPER 1000 ventilator attempts to maintain a constant V T at various ambient pressures by adjusting the inspiratory valve opening. Clinicians should be aware of the range of compensation, which is predictable for each ATA level. Setting a V T outside the range can result in an unwanted decrease in V E with adverse clinical consequences. The maximal V E provided by the ventilator may be insufficient, especially at high ATA levels and for patients with lung injuries and moderate-high ventilatory needs. The manufacturer should consider restricting the settings to those within the operational range of the ventilator.
References
Weaver LK (2011) Hyperbaric oxygen in the critically ill. Crit Care Med 39:1784–1791
Skinner M (1998) Ventilator function under hyperbaric conditions. Diving Hyperb Med J 28:62–71
Workman WT (1999) Hyperbaric facility safety: a practical guide. Best Pub. Co., Flagstaff
Stahl W, Radermacher P, Calzia E (2000) Functioning of ICU ventilators under hyperbaric conditions–comparison of volume- and pressure-controlled modes. Intensive Care Med 26:442–448
Stanga D, Beck G, Chimiak J (2003) Evaluation of respiratory support devices for use in the hyperbaric chamber. NEDU TR 03-18 Panama City, FL, Department of Defense, Navy Experimental Diving Unit
Blanch PB, Desautels DA, Gallagher TJ (1989) Mechanical ventilator function under hyperbaric conditions. Undersea Hyperb Med 16 (Supp):17
Lyazidi A, Thille AW, Carteaux G, Galia F, Brochard L, Richard JC (2010) Bench test evaluation of volume delivered by modern ICU ventilators during volume-controlled ventilation. Intensive Care Med 36:2074–2080
Thille AW, Lyazidi A, Richard JC, Galia F, Brochard L (2009) A bench study of intensive-care-unit ventilators: new versus old and turbine-based versus compressed gas-based ventilators. Intensive Care Med 35:1368–1376
West JB (1999) The original presentation of Boyle’s law. J Appl Physiol 87:1543–1545
Tassaux D, Jolliet P, Thouret JM, Roeseler J, Dorne R, Chevrolet JC (1999) Calibration of seven ICU ventilators for mechanical ventilation with helium-oxygen mixtures. Am J Respir Crit Care Med 160:22–32
Weaver LK, Greenway L, Elliot CG (1988) Performance of the Sechrist 500A hyperbaric ventilator in a monoplace hyperbaric chamber. J Hyperb Med 3:215–225
Churchill S, Weaver LK, Haberstock D (1999) Performance of the Omni-vent mechanical ventilator for use with the monoplace hyperbaric chamber. Undersea Hyperb Med 26(Suppl):70–71
Moon RE, Bergquist LV, Conklin B, Miller JN (1986) Monaghan 225 ventilator use under hyperbaric conditions. Chest 89:846–851
Hennessey PJ (2007) Evaluation of the UNI-VENT Eagle Model 754 ventilator for use in the surface recompression chambers (SRC) of the submarine rescue diving and recompression system (SRDRS). NEDU TR 07-03 Panama City, FL, Department of Defense, Navy Experimental Diving Unit
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lefebvre, JC., Lyazidi, A., Parceiro, M. et al. Bench testing of a new hyperbaric chamber ventilator at different atmospheric pressures. Intensive Care Med 38, 1400–1404 (2012). https://doi.org/10.1007/s00134-012-2590-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2590-4