Abstract
Objective
To describe the incidence, risk factors, and impact on mortality of acute kidney injury (AKI) in patients with 2009 influenza A (H1N1) viral pneumonia requiring mechanical ventilation.
Design
Observational cohort study.
Patients and methods
AKI was defined as risk, injury or failure, according to the RIFLE classification. Early and late AKI were defined as AKI occurring on intensive care unit (ICU) day 2 or before, or after ICU day 2, respectively. Demographic data and information on organ dysfunction were collected daily.
Results
Of 84 patients, AKI developed in 43 patients (51%). Twenty (24%) needed renal replacement therapy. Early and late AKI were found in 28 (33%) and 15 (18%) patients, respectively. Patients with AKI, as compared with patients without AKI, had higher Acute Physiology and Chronic Health Evaluation (APACHE) II score and ICU mortality (72% versus 39%, p < 0.01) and presented on admission more marked cardiovascular, respiratory, and hematological dysfunction. Patients with early but not late AKI presented on admission higher APACHE II score and more marked organ dysfunction, as compared with patients without AKI. ICU mortality was higher in late versus early AKI (93% versus 61%, p < 0.001). On multivariate analysis, only APACHE II score and late but not early AKI [odds ratio (OR) 1.1 (95% confidence interval 1.0–1.1) and 15.1 (1.8–130.7), respectively] were associated with mortality.
Conclusions
AKI is a frequent complication of 2009 influenza A (H1N1) viral pneumonia. AKI developing after 2 days in ICU appears to be associated with different risk factors than early AKI, and is related to a higher mortality rate.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common complication in patients admitted to the intensive care unit (ICU), with a prevalence rate ranging from 16% to 35% in ICU patients, depending on the definition used, reaching 75% for patients in shock; it is associated with a high mortality rate [1–5].
There is very limited information concerning the incidence, risk factors, and impact on mortality of AKI in patients with 2009 influenza A (H1N1) viral pneumonia requiring mechanical ventilation [6–10]. Trimarchi et al. [11] found that AKI was present in 64% of ICU patients with pandemic 2009 influenza A (H1N1) and was associated with 83% mortality. Rello et al. [7] found, in a population of 32 patients with H1N1 influenza requiring ICU admission, that 21% required renal replacement therapy (RRT). Other studies have reported a prevalence rate of AKI in patients with H1N1 influenza virus infection of 25% and 33% [12, 13]. In an autopsy study of 21 fatal cases of 2009 influenza A (H1N1), 9 patients (43%) were reported to have developed AKI, 4 required dialysis [14], and all had mild to moderate renal acute tubular necrosis on microscopic examination.
The aim of this study is to evaluate the incidence, risk factors, and impact on mortality of AKI in critically ill patients with 2009 influenza A (H1N1) viral pneumonia requiring mechanical ventilation. In addition, we hypothesized that AKI diagnosed soon after ICU admission had different clinical characteristics and impact on mortality than AKI diagnosed later in the course of the illness.
Patients and methods
Study design
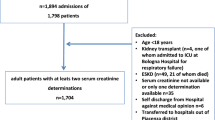
We conducted an observational cohort study enrolling all consecutive patients older than 18 years of age, with the diagnosis of confirmed or probable pandemic 2009 influenza A (H1N1) viral pneumonia, diagnosed as defined by the World Health Organization [15], and requiring mechanical ventilation, admitted to 13 ICUs in Argentine, Chile, and Uruguay, from May 1, 2009 to September 31, 2009. The Ethics Committee of each participating institution approved the study protocol. From the original cohort, patients with chronic renal failure, missing data or unknown ICU discharge status were excluded from the analysis.
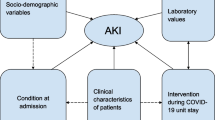
Data collection
Data were collected by accessing each patient’s clinical records. For each patient, we collected demographic data, Acute Physiology and Chronic Health Evaluation (APACHE) II score using the worst values within the first 24 h after ICU admission, and the presence of comorbidities. Although the use of more modern severity scoring systems would have seemed more advisable, the used score was widely available and still allows for group comparisons. We collected on admission and on daily basis at 8:00 a.m. information on arterial blood gases, serum creatinine and bilirubin concentration, blood platelet count, vasoactive drugs dosage, as well as development of bacterial pneumonia and requirement for RRT. Information was recorded daily until death, ICU discharge or day 28, whichever came first. Day 1 started at 8:00 a.m. on the first ICU day.
Nasopharyngeal swab specimens were collected on admission, and bronchial aspirate samples were obtained after tracheal intubation. Specimens were placed in transport medium and kept at 2–4°C. Reverse-transcription polymerase chain reaction (RT-PCR) testing was done in accordance with published guidelines from the US Centers for Disease Control and Prevention [15]. A positive RT-PCR test in a respiratory sample (nasopharyngeal swab or tracheal aspirate) was required for confirmation of the diagnosis of 2009 influenza A (H1N1) pulmonary virus infection.
Definitions
AKI was classified according to the risk of renal failure, injury to the kidney, failure of kidney function, loss of kidney function, and end-stage kidney disease (RIFLE) criteria with a modification of the urine output criterion [1–3]. For this study, the RIFLE outcome categories loss and end-stage kidney disease were not evaluated [3]. Baseline serum creatinine values were estimated using the Modification of Diet in Renal Disease (MDRD) equation, as recommended by the Acute Dialysis Quality Initiative (ADQI) Working Group (assuming a lower limit of normal baseline glomerular filtration rate of 75 ml/min) and similar to previous studies [1–3]. For analysis, patients were assigned their worst RIFLE category according to either serum creatinine (the maximum value over a given time period) or urine output criteria. Early AKI was defined as that occurring on admission or on 8:00 a.m. data on day 1 or day 2. Late AKI was defined as that occurring after day 2 data.
Use of vasopressor was defined as the requirement for norepinephrine at any dosage or dopamine at dosage >5 μg/kg/min. Hematological dysfunction was defined as coagulation Sequential Organ Failure Assessment (SOFA) score higher than 2. Fluid balance was calculated as the difference between fluid input and fluid output. Fluid input included all fluids infused by intravenous or enteral routes. Fluid output included urine output, volume of gastric residue, and fluid loss from drains.
Bacterial pneumonia as a complication of viral pneumonia was diagnosed in the presence of purulent sputum and significant growth of a potentially pathogenic microorganism in a tracheal aspirate sample culture accompanied by fever or an increase in white blood cell count. Bacteremia was diagnosed when a potentially pathogenic microorganism grew in more than one blood culture.
Statistical analysis
Outcome variables were compared between patients without AKI and patients with AKI, as well as between patients with early and late AKI. Continuous variables are expressed as mean (standard deviation, SD) or median (interquartile range) and were compared using Student’s t test or analysis of variance (ANOVA) with post hoc Scheffé test. For nonparametric variables, Kruskal–Wallis test was used. Categorical variables were expressed as proportions and were compared by the χ 2 or Fisher exact test. Multivariate analysis was performed using ICU mortality as the dependent variable, including in the maximal model the variables associated with mortality (p < 0.1) on univariate analysis. The odds for dying is expressed as the odds ratio (OR) and its 95% confidence interval (CI). Two-sided p value less than 0.05 was considered statistically significant.
Results
General characteristics
During the observation period, 115 patients were admitted to the ICU with the diagnosis of 2009 influenza A (H1N1) viral pneumonia requiring mechanical ventilation. Six patients were excluded because of chronic renal failure, and 25 because of missing data.
Characteristics of the 84 patients included are shown in Table 1. Diagnosis was confirmed by positive PCR test in respiratory samples in 56 (67%) cases. No patient was lost to follow-up to the specific time end points.
Acute kidney injury
AKI developed in 43 (51%) of 84 patients with influenza A (H1N1) viral pneumonia, and 20 needed RRT. Patients with risk (5/43, 12%), injury (11/43, 25%), and failure (27/43, 63%) had mortality of 40%, 64%, and 78%, respectively.
Patients with AKI were, as compared with patients without AKI, more likely to be male and obese, and had higher APACHE II score and greater ICU mortality. Noninvasive ventilation (NIV) was used less often in patients with AKI than in patients without AKI. Organ dysfunction was also more severe in patients with AKI, as indicated by higher prevalence of shock, and lower PaO2/FiO2 ratio and blood platelet count (Table 1). As the observed difference in APACHE II score between patients without and with AKI could be due to the renal component of the score, we recalculated the APACHE II score without the renal component, finding it to be not significantly different between non-AKI and AKI (p = 0.65) or between early and late AKI (p = 0.32).
There was no difference (comparison between groups not shown) between the non-AKI and the AKI groups in (data presented as median [IQR], percentage or mean ± SD for the entire group of 84 patients) the prevalence of different comorbidities, the NIV failure rate (29 of 33 who received NIV [87.5%]), days from onset of symptoms to ICU admission (6 [7–9]), prevalence of bacterial pneumonia as a complication (27/84 [32%]) or prevalence of bacteremia as a complication (8/84 [9.5%]). In addition, mean arterial pressure (81 ± 21 mmHg), tidal volume delivered (480 ± 108 ml/kg), peak airway pressure (30 ± 7 cmH2O), plateau airway pressure (25 ± 6 cmH2O), arterial pH (7.25 ± 0.34), PaCO2 (47 ± 19 mmHg), white blood cell count (11,159 ± 7,506 cells/μl), lymphocyte count (915 ± 852 cells/μl), serum lactate dehydrogenase (LDH) activity (1,185 ± 1,121 U/l), and lactate serum concentration (2.3 ± 2.1 mmol/l) were not significantly different between the two groups. Of 77 patients who received treatment with neuraminidase inhibitors, 41 (53%) died, whereas among 7 who did not receive treatment, 5 (71%) died (p = 0.30).
Early versus late AKI
Early AKI was found in 28 patients (33% of all patients), and late AKI in 15 (18% of all patients) (Table 1).
When comparing early versus late AKI, some differences not obvious in the AKI versus non-AKI comparison became evident. Male predominance, as compared with the non-AKI population, was observed in both early and late AKI. The APACHE II score, however, was higher than in non-AKI patients in early but not in late AKI.
Early AKI did not impact duration of mechanical ventilation or ICU length of stay, and mortality was nonsignificantly higher than in non-AKI patients. Only patients with late AKI had, as compared with patients without AKI, a nonsignificant trend towards more prolonged duration of mechanical ventilation and ICU and hospital length of stay, and significantly higher mortality (Table 1).
Similarly, as compared with patients without AKI, in patients with early but not late AKI, the difference in PaO2/FiO2 ratio, blood platelet count, and serum bilirubin concentration on ICU admission reached statistical significance. ICU mortality was higher in late than in early AKI (Table 1).
Other variables [prevalence of comorbidities, bacterial pneumonia as complication, bacteremia, heart rate, mean arterial pressure, tidal volume delivered, peak and plateau airway pressure, white blood cell and lymphocyte counts, international normalized ratio (INR), and serum LDH activity] were comparable in patients with early versus late AKI (not shown).
Among patients with early AKI (n = 28), 15 of 20 (75%) whose renal function did not improve over time died, whereas 2 of 8 (25%) whose renal function improved died (Fig. 1).
The number of patients with AKI receiving RRT was 9 of 28 in the early AKI and 10 of 15 in the late AKI group. Of those, four (one before day 14 and three after day 14 of RRT) in the early AKI group and one (before day 14 of RRT) in the late AKI group came off RRT and survived. One additional patient without AKI received RRT in the context of multiorgan dysfunction as per the criterion of the attending physician.
Variables associated with mortality
Only the APACHE II score, the diagnosis of cardiovascular, hematological, respiratory failure, and the diagnosis of late AKI were associated with mortality on univariate analysis. Early AKI was not related to mortality. Since RRT is known to be associated with mortality, and RRT was used less frequently in early than in late AKI, it is possible that the difference in mortality observed in early and late AKI was due to the different mortality rate associated with RRT. Among 19 patients receiving RRT, 14 (74%) died, whereas among 24 patients not receiving RRT, 16 (67%) died (p = 0.4). Thus the impact of RRT on mortality did not reach statistical significance, and RRT was not associated with mortality on multivariate analysis.
On multivariate analysis, only APACHE II score on admission and the diagnosis of late AKI were associated with mortality (Table 2).
Discussion
Several publications have reported the clinical characteristics and outcomes of critically ill patients with 2009 influenza A (H1N1). However, many aspects of the disease remain to be studied, including the prevalence and impact on mortality of organ dysfunction. Specifically, there is very limited information concerning the clinical characteristics of patients with 2009 influenza A (H1N1) and AKI.
The 51% prevalence of AKI in our series is somewhat lower than the 67% reported by Sood et al. in patients with pandemic H1N1 influenza admitted to the ICU [9], but similar to the prevalence reported for general ICU patients (20–75%) using the same RIFLE criteria [16]. Furthermore, the rate of AKI within the first 48 h (33%) is in line with the currently reported incidence in ICUs [1]. Although we cannot explain the difference from the previously reported incidence of AKI in pandemic 2009 influenza A (H1N1) [9], it is possible that different treatment strategies could be related to differences in the prevalence of AKI. In fact, most of the patients in Sood et al.’s study [9] had AKI by the urine output criterion and only 25% by the serum creatinine criterion, whereas in our series patients were nonoliguric on average (mean urine output 0.9 ml/kg/h). The prevalence of acute kidney injury in general ICU patients reported in the SOAP study [17] was lower than in our cases (36%), but in that study [17] diagnostic criteria indicative of more severe renal injury (serum creatinine >3.5 mg/dl or urine output <500 ml in 24 h) were used.
The distribution of patients in the different AKI classes (risk, injury, and failure) in patients with pandemic H1N1 influenza has not been previously reported. In the present report, it was 12%, 25%, and 63%, respectively. AKI class distribution reported in general ICU patients by Hoste et al. [18] was 18%, 40%, and 42%, respectively (recalculated from the original data).
The mortality of patients without AKI in the present series (39%) was much higher than the 5% [17] or 16% [18] reported in general ICU patients without AKI and the 17% in patients with pandemic H1N1 influenza [18]. Patients in those series [17, 18] were general ICU patients with less severity. For instance, in the SOAP study [17], about two-thirds of patients were on mechanical ventilation, less than one-quarter had respiratory failure, and only one-quarter had sepsis on admission. Our patients were all on mechanical ventilation, all had acute respiratory distress syndrome (ARDS), and 44% were in shock. Genetic background, date of censorship for mortality reporting, or nonobvious differences in treatment could also explain to some extent the observed dissimilarities.
As expected, AKI was generally diagnosed in sicker patients. Patients with AKI, as compared with patients without AKI, had higher APACHE II score and higher incidence of organ dysfunction (cardiovascular, respiratory, hematological) on admission. APACHE IInonrenal was not different between patients without and with AKI, indicating that it is the renal component of the score that determines the detected difference, and that risk factors not captured by the APACHE II score are related to the development of AKI.
According to our hypothesis, we found that the time of onset of AKI characterized two different populations. Patients with early AKI had only slightly and nonsignificantly higher mortality rate than patients without AKI, whereas patients with late AKI had significantly higher mortality than patients with either non-AKI or early AKI. In the study by Payen et al. [17], patients with early AKI had similar mortality rates to patients with late AKI. We cannot explain this discrepancy based on our results. Different availability of the use of RRT could explain these differences. Our results (higher mortality rate of late versus early AKI, and low mortality rate in those patients with early AKI whose renal function improves over time) are biologically plausible. Early AKI, probably determined to some extent by perfusion abnormalities in the context of insufficient or still ongoing resuscitation, is associated with a lower mortality rate than late AKI, which generally appears in combination with sepsis, multiple organ failure, and use of nephrotoxic agents. However, the lack of urinary indices or information concerning the response to fluid challenge makes our interpretation of the lower mortality rate of early versus late AKI purely speculative. It is very likely that the different mortality rate in early versus late AKI is due to the higher rate of resolution of renal dysfunction and the associated lesser requirement for RRT in early compared with late AKI.
There is a lack of information on the incidence and mechanisms of AKI in viral infections. Tentative explanations for AKI in patients with pandemic 2009 influenza A (H1N1) would be those proposed for AKI in general critically ill patients, including insufficient resuscitation and, in the context of the inflammatory response, perfusion failure and cell injury. Rhabdomyolysis, which certainly could contribute to AKI, has been reported in patients with pandemic 2009 influenza A (H1N1) [8, 19]. Whether there is virus present in renal tissue that could induce specific effects on renal function has not been reported as yet.
Patients with late AKI had a similar APACHE II score to patients without AKI. This result suggests that events taking place after admission (whose severity is not reflected in the admission APACHE II score) explain the development of AKI during the ICU course.
It is possible that, as RRT was used less frequently in early than in late AKI, the observed mortality difference in the two groups was due to the different use of RRT. In our study, the impact on mortality of the use of RRT did not reach statistical significance. Of 20 patients receiving RRT, 14 died and only 6 survived (p = 0.09). Consequently, although it is possible that this lack of significance is due to the small sample size, our results indicate that, regardless of the different use of RRT, early AKI is associated with a lower mortality rate than late AKI.
Limitations
A major limitation of this study is its observational nature, allowing only the study of associations but precluding the assessment of cause and effect relationships. Second, the lack of information pertaining to many confounders (such as delay in oseltamivir treatment, availability, timing of renal replacement therapy, use of goal-directed sepsis therapy, ability to clear the virus, and use of nephrotoxic agents) forestalls the control of important variables that might play a role in the relationship between H1N1 influenza and AKI. In addition, this lack of information prevents us from speculating as to the causes of the development of late AKI. In addition, chronic renal failure, as self-reported or recorded in the patients’ medical records, was an exclusion criterion. However, we could not determine whether elevated baseline serum creatinine was early AKI or rather indicated stable chronic renal failure. Finally, our results on the analysis of patients from a specific geographic area may not be generalizable to other areas.
Interpretation
AKI developing early after ICU admission that resolves over time is probably related to hemodynamic abnormalities rather than to inflammatory or sepsis-induced mechanisms. If this abnormal hemodynamics resolves (patients with early AKI that resolves over time), the mortality rate is comparable to that of patients with normal renal function. AKI that develops later in the course of the disease, appearing in the context of multiorgan dysfunction, is associated with a very high mortality rate. The severity of patients with late AKI is not captured on admission by the APACHE II score, suggesting that events taking place after ICU admission, and possibly amenable to preventive measures, are involved in the development of late AKI.
Conclusions
Patients with influenza A (H1N1) viral pneumonia have a high incidence of AKI. Late but not early AKI is associated with a large impact on mortality.
References
Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, Metnitz PG (2009) Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med 35:1692–1702
Bagshaw M, George C, Bellomo R for the ANZICS Database Management Committee (2008) Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care 12:R47
Ostermann M, Chang RW (2007) Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med 35:1837–1843
Tejerina E, Frutos-Vivar F, Restrepo MI, Anzueto A, Abroug F, Palizas F, Gonzalez M, D’Empaire G, Apezteguia C, Esteban A (2006) Incidence, risk factors, and outcome of ventilator-associated pneumonia. J Crit Care 21:56–65
Thakar CV, Christianson A, Freyberg R, Almenoff P, Render ML (2009) Incidence and outcomes of acute kidney injury in intensive care units: a Veterans Administration study. Crit Care Med 37:2552–2558
The ANZIC influenza investigators, Webb SA, Pettilä V, Seppelt I, Bellomo R et al (2009) Critical care services and 2009 H1N1 influenza in Australia and New Zealand. NEJM 361:1925–1934
Rello J, Rodríguez A, Ibéñez P, Socías L, Cebrián J, Marqués A, Guerrero J, Ruiz-Santana S, Márquez E, Del Nogal-Saez F, Álvarez-Lerma F, Martínez S, Ferrer M, Avellanas M, Granada R, Maraví-Poma E, Albert P, Sierra R, Vidaur L, Ortiz P, Prieto del Portillo I, Galván B, León-Gil C; H1N1 SEMICYUC Working Group (2009) Intensive care adult patients with severe respiratory failure caused by influenza A (H1N1) in Spain. Crit Care 13:R148
Domínguez-Cherit G, Lapinsky SE, Macías AE, Pinto R, Espinosa-Pérez L, de la Torre A, Poblano-Morales M, Baltazar-Torres JA, Bautista E, Martínez A, Martínez MA, Rivero E, Valdez R, Ruiz-Palacios G, Hernández M, Stewart TE, Fowler RA (2009) Critically Ill patients with 2009 influenza A (H1N1) in Mexico. JAMA 302:1880–1887
Sood MM, Rigatto C, Zarychanski R, Komenda P, Sood AR, Bueti J, Reslerova M, Roberts D, Mojica J, Kumar A (2010) Acute kidney injury in critically Ill patients infected with 2009 Pandemic Influenza A (H1N1): report from a Canadian Province. Am J Kidney Dis 55:848–855
Fowler RA, Lapinsky SE, Hallett D, Detsky AS, Sibbald WJ, Slutsky AS, Stewart TE (2003) Critically ill patients with severe acute respiratory syndrome. Toronto SARS Critical Care Group. JAMA 290:367–373
Trimarchi H, Greloni G, Campolo-Girard V, Giannasi S, Pomeranz V, San-Roman E, Lombi F, Barcan L, Forrester M, Algranati S, Iriarte R, Rosa-Diez G (2010) H1N1 infection and the kidney in critically ill patients. J Nephrol [Epub ahead of print]
Ugarte S, Arancibia F, Soto R (2010) Influenza A pandemics: Clinical and organizational aspects: The experience in Chile. Crit Care Med 38:133–137
Pérez-Padilla R, de la Rosa-Zamboni D, Ponce de León S, Hernández M, Quiñones-Falconi F, Bautista E, Ramírez-Venegas A, Rojas-Serrano J, Ormsby CE, Corrales A, Higuera A, Mondragón E, Cordova-Villalobos JA (2009) INER Working Group on Influenza. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med 361:680–689
Mauad T, Hajjar LA, Callegari GD, da Silva LF, Schout D, Galas FR, Alves VA, Malheiros DM, Auler JO Jr, Ferreira AF, Borsato MR, Bezerra SM, Gutierrez PS, Caldini ET, Pasqualucci CA, Dolhnikoff M, Saldiva PH (2010) Lung pathology in fatal novel human influenza A (H1N1) infection. Am J Respir Crit Care Med 181:72–79
Pandemic (H1N1). Geneva: World Health Organization. (Accessed November 20, 2009, at http://www.who.int/csr/disease/swineflu/en/index.html)
Joannidis M, Metnitz PG (2005) Epidemiology and natural history of acute renal failure in the ICU. Crit Care Clin 21:239–249
Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL (2008) Sepsis Occurrence in Acutely Ill patients (SOAP) investigators. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care 2008:R74
Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA (2006) RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care:R73
Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, Stelfox T, Bagshaw S, Choong K, Lamontagne F, Turgeon AF, Lapinsky S, Ahern SP, Smith O, Siddiqui F, Jouvet P, Khwaja K, McIntyre L, Menon K, Hutchison J, Hornstein D, Joffe A, Lauzier F, Singh J, Karachi T, Wiebe K, Olafson K, Ramsey C, Sharma S, Dodek P, Meade M, Hall R, Fowler RA (2009) Critically ill patients with 2009 influenza A (H1N1) infection in Canada. JAMA 302:1872–1879 Canadian Critical Care Trials Group H1N1 Collaborative
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in an editorial available at: doi:10.1007/s00134-011-2196-2; related material can be found at: doi:10.1007/s00134-011-2166-8 and doi:10.1007/s00134-011-2183-7.
Participating units
Participating units
Argentina
Hospital General de Agudos Dalmacio Vélez Sarsfield (CABA). Valdez P, Baskard MZ.
Hospital Universitario Universidad Abierta Interamericana (CABA). Chiappero G, Morales J.
Hospital Donación Francisco Santojanni (CABA). Saldarini F, Borello S.
Hospital Luis Carlos Lagomaggiore (Mendoza). Chena A, Zakalik G.
Hospital Universitario Austral (Pilar). Alvarez J, Pratesi P.
Spain
Hospital Universitario de Getafe (Madrid). Nin N, Frutos F, Lorente JA, Cortés I.
Chile
Instituto Nacional de Tórax (Santiago de Chile). Mora F, Valenzuela H, Ferreira L.
Hospital Regional de Concepción, Concepción, Chile. Ortega C, Ferreira L.
Uruguay
Hospital Español Juan J Crottogini. Buroni M, Villariño C, Hurtado J.
Sanatorio Cudam Colon. Chassale L, Bayardo G.
Hospital Maciel (Montevideo). Echevarría E, Bagnulo H.
Sanatorio CASMU. Cardinal P, Deicas A.
Hospital General de las Fuerzas Armadas. Cardinal P.
Rights and permissions
About this article
Cite this article
Nin, N., Lorente, J.A., Soto, L. et al. Acute kidney injury in critically ill patients with 2009 influenza A (H1N1) viral pneumonia: an observational study. Intensive Care Med 37, 768–774 (2011). https://doi.org/10.1007/s00134-011-2167-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2167-7